INTRODUCTION
Psoriasis is a common, chronic, inflammatory and immuneediated skin disease associated with cardiovascular comorbidities
1.
The Psoriasis Area and Severity Index (PASI) is the currently preferred tool to assess disease severity and to evaluate the efficacy of the treatment
2. Since the method is limited by physician-dependent scoring, many laboratory markers have been studied in psoriasis to find an objective tool to assess disease activity
3456789101112.
The levels of serum C-reactive protein (CRP) and neutrophil-lymphocyte ratio (NLR), both of which are inexpensive and easily accessible markers, have been reported to be elevated in patients with psoriasis, and in some studies, CRP and NLR were found to be correlated with the disease activity regarding as PASI
891011. Moreover, elevated levels of both CRP and NLR have been demonstrated to be related with cardiovascular diseases (CVD) and with cardiovascular comorbidities in psoriasis
910111213.
In the search for objective assessment tools for psoriasis, CRP and NLR have been used to demonstrate treatment efficacy in psoriasis. But the few studies on this topic have mostly been performed among patients receiving biologic agents
314151617.
The present study sought to evaluate the levels of CRP and NLR in patients with psoriasis under different systemic treatment modalities, including narrow-band ultraviolet B (NBVB), acitretin, methotrexate (MTX), cyclosporine, adalimumab (ADA), etanercept (ETA), and ustekinumab (UST).
Go to :

MATERIALS AND METHODS
Study population and protocols
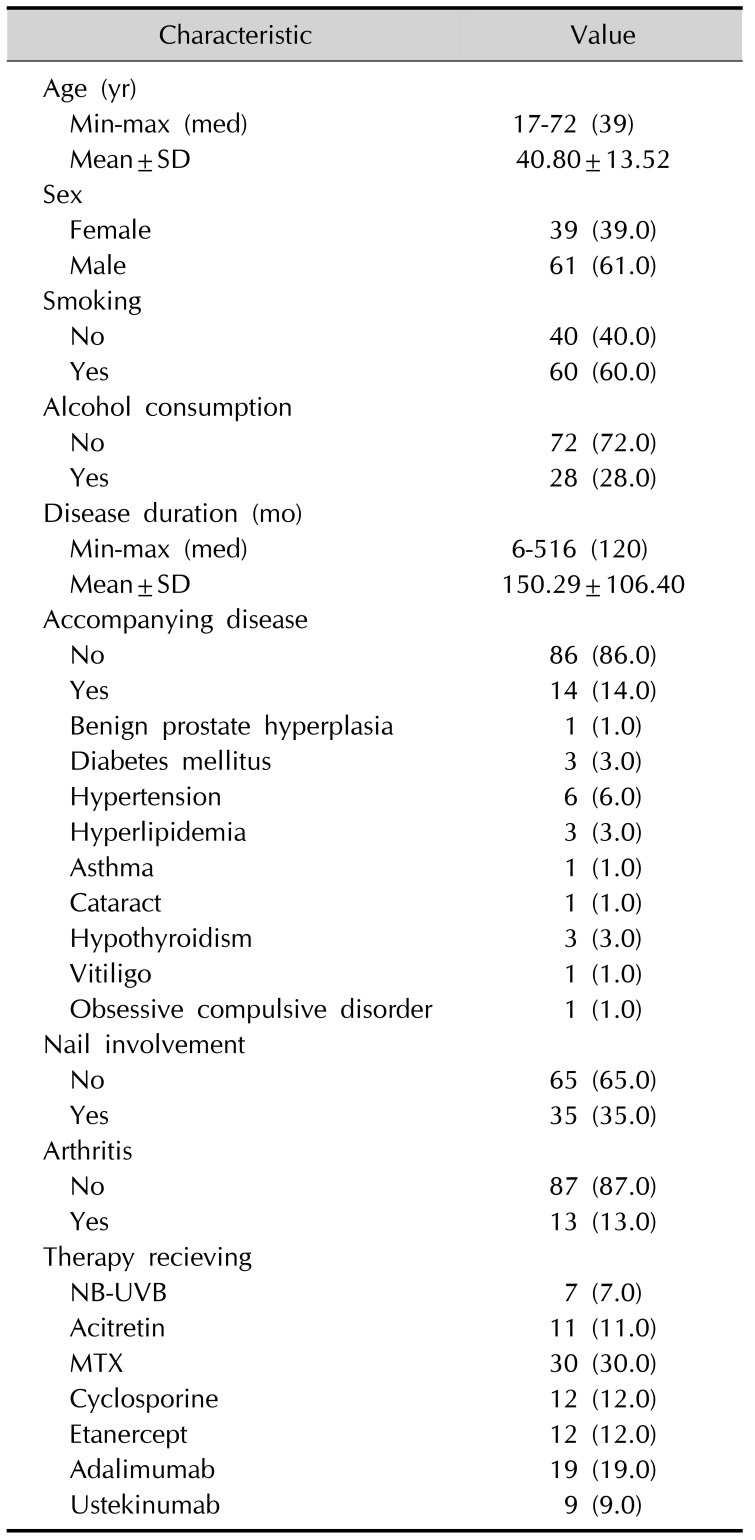
A single-centre observational study was performed. One hundred outpatients diagnosed with chronic plaque type psoriasis by a clinical or histopathological examination were recruited from the Department of Dermatology.
Data on the baseline demographics, clinical characteristics (including information about the duration of psoriasis, medical history, tobacco smoking and alcohol habits), concomitant arthritis and/or nail involvement were recorded. The inclusion criteria for patients were as follows: 1) patients with chronic plaque type psoriasis, 2) aged greater than 18 years, 3) who had not received any topical and/or systemic psoriasis treatment prior to 6 months, and 4) who had a clinical indication to initiate systemic therapy for psoriasis according to the European psoriasis treatment guideline
18.
The exclusion criteria included a lack of co-operability, any contraindication for the treatment, any significant infection, immunodeficiency, pregnancy or breastfeeding, the use of systemic and/or topical treatment during the last 6 months before the inclusion, and malignancy.
Treatment regimes
The appropriate treatment modality was decided upon together with the patient, according to the psoriasis treatment guidelines
18 and the patients' characteristics. Each patient was started on one of the following psoriasis treatment: NB-UVB, acitretin, cyclosporine, MTX, ADA, ETA or UST. Before and during the treatment, each patient underwent laboratory and physical controls, as recommended in the treatment guidelines
18.
The treatment regimes were as follows: ETA 50 mg subcutaneous (SC) injection once a week, an initial dose of ADA 80 mg and 40 mg SC injection every other week thereafter. UST was administrated SC (45 mg) at weeks 0, 4, and every 12 weeks thereafter. MTX doses were 15±25 mg subcutaneously once a week, cyclosporine was administered orally every day (2.5~5 mg/kg), acitretin was administered orally (10~25 mg/day), and NB-UVB (7002k Cabinet; Waldmann, Villingen-Schwenningen, Germany) was administered three times a week with a gradual increase in dosing.
None of the patients received any topical treatments other than moisturizers.
Evaluation of inflammatory markers and PASI
The serum CRP and complete blood count were measured at the baseline/before treatment and at 12 weeks of treatment.
Psoriasis was graded according to the PASI calculated at the baseline and at 12 weeks of treatment by a singlelinded dermatologist.
The study was reviewed and approved by Şişli Hamidiye Etfal Training and Research Hospital Clinical Research Ethics Committee (IRB no. 574, 10/01/2016), and all the individuals provided written informed consent. The study was carried out according to the principles expressed in the Declaration of Helsinki.
Statistical analyses
The Number Cruncher Statistical System 2007 (Kaysville, UT, USA) program was used for the statistical analysis. The descriptive data were expressed with mean± tandard deviation, numeric variables and percentages. In the analysis of normally distributed variables, a Student's t-test was applied to examine the differences between the two groups. The differences between the two independent groups were examined using the non-parametric Mann–Whitney U-test for non-normally distributed variables. The comparisons between three or more groups of non-normally distributed were evaluated with a Kruskal–Wallis test and Wilcoxon Student's t-test using Bonferroni's correction for multiple comparisons. The intragroup comparisons of normally distributed data were performed with paired samples test, whereas the non-normally distributed data of intragroup comparisons were evaluated with a Wilcoxon signed ranks test. A Pearson χ2 test was used to compare qualitative variables. The correlation analysis was performed by calculating Pearson and Spearman's rank correlation, and p<0.05 was considered statistically significant.
Go to :

DISCUSSION
Several researchers have investigated the levels of inflammatory parameters in psoriasis and the association between the biomarkers and disease activity. Among many parameters, we chose to evaluate the levels of CRP and NLR since they are both reliable parameters indicating systemic inflammation and cardiovascular risks, as well easily accessible and inexpensive methods.
Psoriasis and CVD based on atherogenesis both share the immunoinflammatory mechanisms that provide the link between the two diseases
19. It has been suggested that systemic anti-inflammatory therapy might be beneficial in reducing the CVD risk among patients with psoriasis
1920. In this study, we prospectively analysed the effects of systemic treatments on inflammatory parameters in psoriasis over a period of 12 weeks.
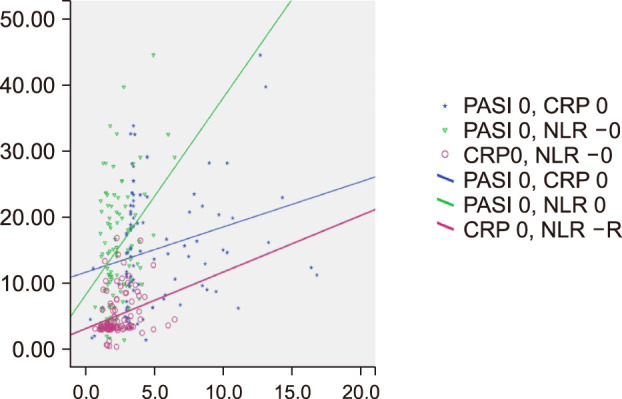
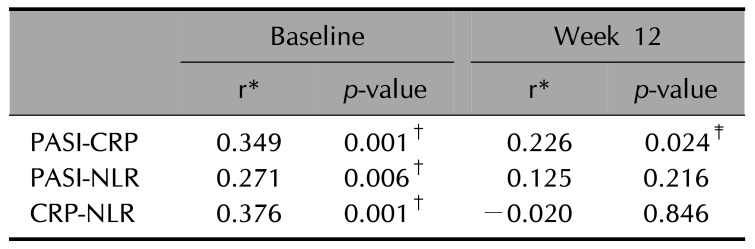
At the baseline evaluation prior to any treatment, the PASI scores were positively correlated with the CRP and NLR values. Moreover, CRP and NLR were also positively correlated. Since, PASI is an established tool in scoring disease severity, these findings may lead us to the suggestion that CRP and NLR might be objective laboratory markers indicating disease severity in psoriasis. Previous reports are in line with this hypothesis
89101112131415.
At week 12, a positive correlation between the PASI and CRP values was noted, but no correlation was found between CRP and NLR or between PASI and NLR.
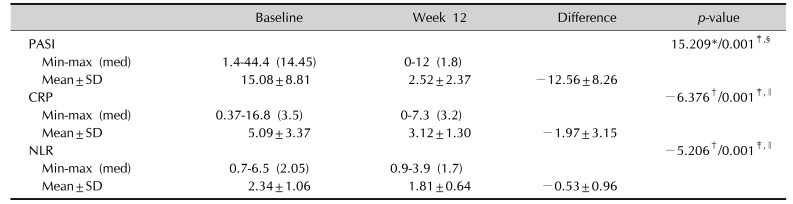
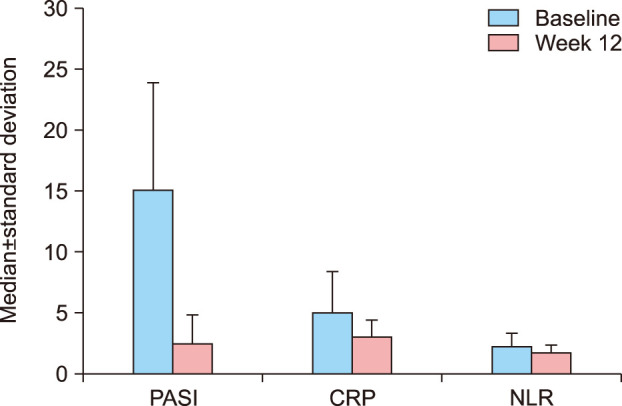
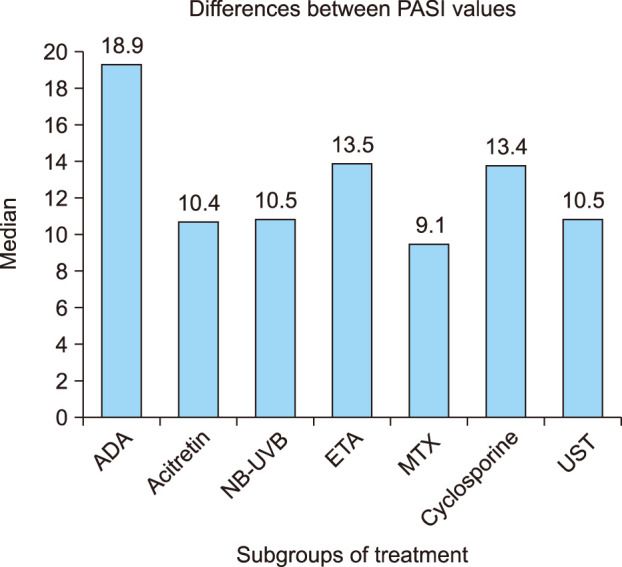
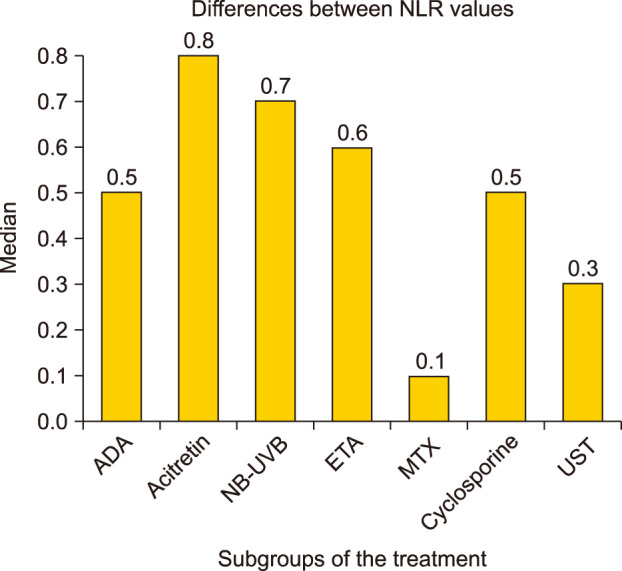
The present study revealed a statistically significant decrease in the values of PASI, serum CRP, and NLR in the study group who received different therapies, including acitretin, MTX, cyclosporine, ADA, ETA, UST, and NB-UVB for a period of 12 weeks.
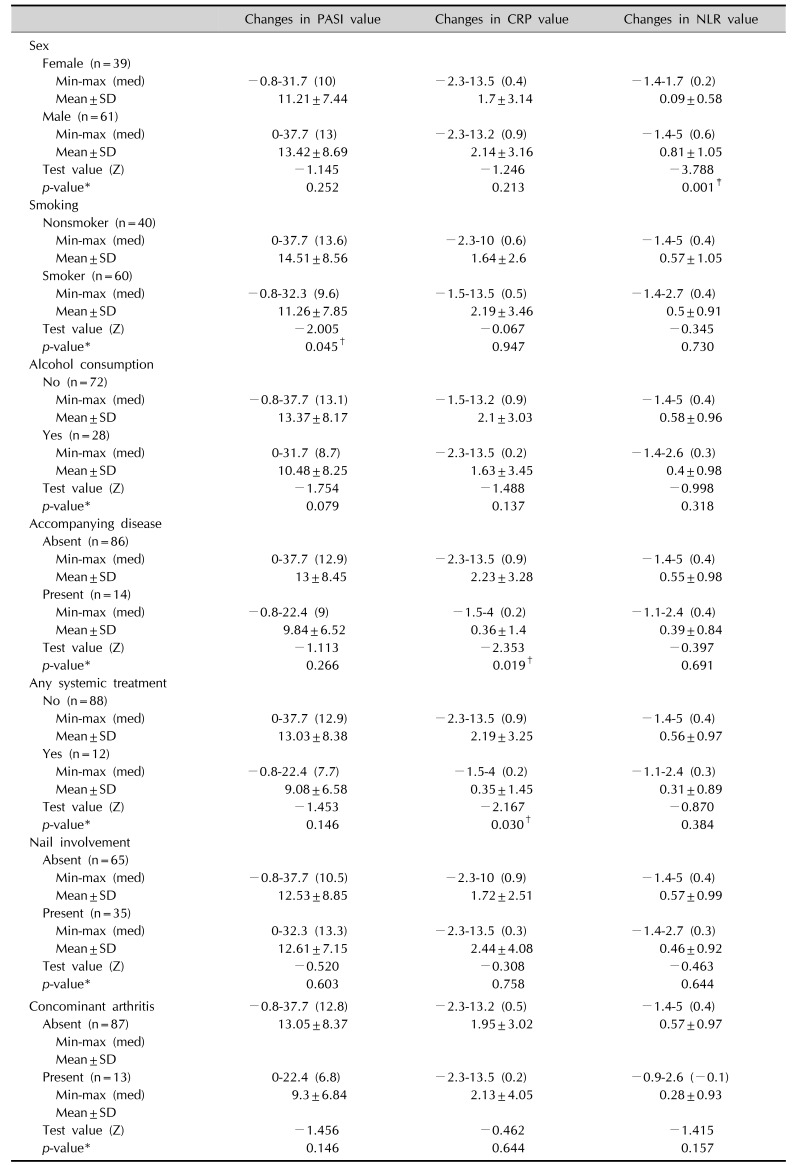
When we evaluated the changes in CRP and NLR according to patients' characteristics, we found that the decrease in NLR values was statistically higher in males than in females. The higher NLR values in males at the baseline may explain this. Still, it cannot be ruled out that a different gender-based response to the treatment may be present.
Median reductions in PASI were greater in non-smokers than in patients who are smokers, which may lead to the suggestion that smoker psoriasis patients may not respond to therapy as well as non-smokers. Smoking has already been shown to be related to the severity of psoriasis
2122, but data on the impact of smoking on therapy response is insufficient. In a recent retrospective study, no statistical difference in terms of clinical improvement in psoriasis among non-smokers and smokers on various systemic treatment regimens was found
23. But if larger epidemiologic studies confirm this relationship, strict guidelines for smokers with psoriasis may be implemented.
The reductions in CRP levels were significantly lower in psoriasis patients who had an accompanying disease than in those who did not. We believe that the ongoing inflammation due to accompanying disease may lead to late or low-response levels of CRP.
Interestingly, although it is known that nail involvement and the occurrence of psoriatic arthritis is related to severe inflammation, no impact was seen in terms of parameter changes
24.
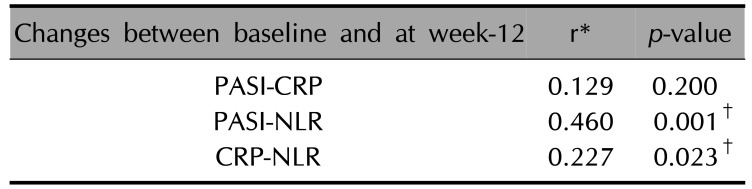
Treatment success, defined as a decrease in the PASI score, was paralleled by reduced serum levels of NLR, but not with CRP. The correspondence between decreases in the NLR levels and PASI scores suggests that NLR and psoriasis severity may be linked. The reduction in CRP levels and NLR was also correlated.
The main purpose of the study was to investigate whether any of the treatment options for psoriasis provide a better anti-inflammatory effect, demonstrated as reductions in CRP and NLR values. Beyond that, we wanted to emphasize that the anti-inflammatory effect could prevent cardiovascular events in patients with psoriasis. In line with our study, some other studies have been performed, but the results of these studies evaluating the cardiovascular events in psoriasis patients under anti-inflammatory treatment have been conflictory
202526. Fewer reports have investigated the changes in laboratory markers under sytemic therapy, and they have been mostly conducted among psoriasis patients recieving the tumor necrosis factor (TNF) blocker or MTX therapy. In different studies, significant reductions in PASI, CRP, interleukin-6, TNF-α, resistin and lipoprotein and an increase in adiponectin were found in patients under various systemic treatments
3471527. Montaudié et al.
28 observed a higher decrease in CRP levels in patients in a biologic agent therapy (infliximab, ETA, ADA, and UST) group than in a conventional systemic therapy (MTX, cyclosporine, and acitretin) group. They found no correlation between the reduction in CRP, erithrocyte sedimentation rate, HbA1c, and PASI
28.
In a distinct departure from the literature, we wanted to evaluate the effects of several therapy agents used in psoriasis on CRP and NLR which are indicators of CVD and systemic inflammation.
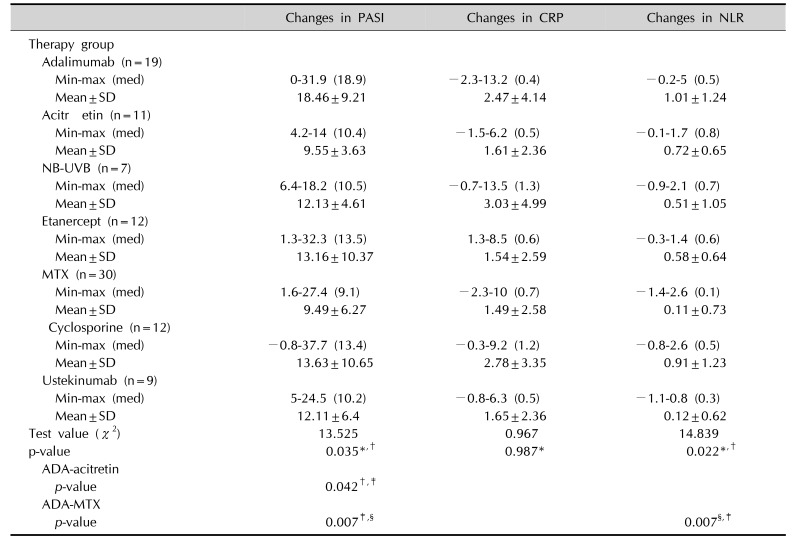
Concerning the changes in CRP levels and NLR and PASI scores after treatment, we found a statistically significant reduction in these values regardless of the type of treatment.
However, when analyses between two groups were performed, these differences had only two results of statistical significance: (1) the decrease in NLR values was statistically higher in ADA group compared with the MTX group, (2) the reduction in PASI scores was statistically higher in the ADA group than in the MTX and acitretin groups.
It is also noteworthy that although statistically significant decreases in the PASI, CRP, and NLR values were demonstrated in patients receiving MTX therapy in the present study, the MTX group had the least decreases in these values compared with other agents.
However, this trend must be viewed with caution because of the small number of patients in each treatment group, which makes the study unpowered. The short-term follow-up period of the study might be another explanation. During the follow-up period, none of the patients had any changes in their lives including, habits (smoking, alcohol, etc.), medical events, dietary habits, any treatment, sports, social activities, etc. Since this information is based on the declarations of the patients, it may be assumed as a limitation. The control group of the study did not consist of healthy subjects. Patients with psoriasis who are not receiving therapy were included as control group and after receiving psoriasis therapy for 12 weeks they presented the study group.
We believe that the results of the study should be acknowledged for several aspects. First of all, this is the first study examining the impact of so many treatment options in psoriasis on CRP and NLR. Moreover, both CRP and NLR are easily accessed parameters in daily practice that may be used to assess the disease activity and to evaluate the efficacy of treatment. And most importantly, since they are both markers of CVD, they may be used to determine the optimal therapy for psoriasis according to a patient's characteristics, preventing cardiovascular comorbidities.
We suggest that controlling the systemic inflammation in psoriasis may prevent cardiovascular comorbidities, which are known to be associated with severe psoriasis. Further studies addressing the impact of long-term systemic therapies on cardiovascular functions in patients with psoriasis are warranted.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download