Abstract
Background
The slide-swing skin flap is a combination of transposition and adjacent skin sliding and can be used to close large, round defects with a flap that is smaller than the primary defect to produce aesthetically good results.
Objective
To evaluate the efficacy and safety of the slide-swing skin flap for various surgical defects caused by skin tumor excisions.
Methods
This retrospective case series, which includes 33 Asian patients between the ages of 25 and 86 years, describes the slide-swing skin flap after primary excision for malignant or premalignant skin conditions. The outcomes were assessed 12 weeks after surgery using the patient and observer scar assessment scale (POSAS).
Results
Patients were 25 male and 8 female, and the causes of surgery were various malignant skin tumors including malignant melanoma, dermatofibrosarcoma protuberans, and malignant nodular hidradenoma. Tumors were on the lower limb in eleven patients, back in nine patients, chest in five patients, face in three patients, buttock in three patients and two patients had tumors in other locations. The mean defect size was 3.5×3.1±1.9×2.2 cm (range, 1.4×0.9~9.0×12.0 cm). The mean patient POSAS total score was 9.7±3.0 and mean patient overall opinion score was 1.8±0.7. The mean observer POSAS total score was 11.0±2.7 and mean observer overall opinion score was 1.9±0.5. All flaps survived and postoperative recoveries were uneventful.
Surgical excision of benign and malignant skin tumors creates surgical defects with a variety of sizes and shapes. For small defects, primary closure after undermining surrounding tissues is optimal, but when defects are too large to enable primary closure or to produce aesthetically acceptable results, reconstruction using a local flap or skin graft is mandatory1.
The slide-swing skin flap technique, also known as slide-swing plasty, is a type of transposition flap that was developed by Schrudde and Petrovici234. However, it does not only show transposition like other transposition flaps, but instead shows a combination of transposition with skin sliding, so is in part based on the principle of Z-plasty2. This technique is usually used to close large, round defects but is also effective for defects with oval or hemispherical shapes. Methods such as the Limberg flap generally require round defects to change the geometric figure, which requires additional excision of healthy skin. Also, the flap should be cut to exactly the same size as the defect5. The slide-swing skin flap allows the incision line to be adjusted to the shape of the defect. Then, the lifted flap is pushed into the primary defect and the adjacent skin surrounding the defect is slid into primary and secondary defects without sacrificing healthy skin. Therefore, in this technique, the flap used for closure is designed to be smaller than the defect and the resulting scar is relatively small.
Herein, we report our experiences using the slide-swing skin flap for the reconstruction of surgical defects after the excision of malignant skin tumors of variable sizes and anatomical locations.
A retrospective chart review was conducted to identify all patients with a surgical defect after the excision of a primary malignant or premalignant skin tumor treated by slide-swing skin flap reconstruction at the Veterans Health Service Medical Center and Gachon University Gil Medical Center between 2011 and 2017. Data were collected on tumor location, tumor type, defect size after primary tumor excision and intraoperative and postoperative complications, such as, wound dehiscence, flap necrosis or flap failure. We received the patient's consent form about this study and publishing all photographic materials. Approval for this study was obtained from the Institutional Review Board of the Veterans Health Service Medical Center and Gachon University Gil Medical Center (IRB no. BOHUN 2018-02-004, GDIRB2018-365).
A round or oval defect was first created during a wide local excision with sufficient healthy margins, and then a slide-swing skin flap was designed alongside the surgical defect (Fig. 1A). Two lines (AD' and AB') bordering the surgical defect were drawn at right angles (α) to each other. A rounded flap (flap AB'C) was then designed with sides that would form an acute angle (β) if they were extended. This flap (AB'C) was then swung into the primary defect. Another flap, DBB', was slid into the secondary defect, that is, into the origin site of flap AB'C. This swing-slide movement between flaps AB'C and DBB' is the equivalent of the asymmetric exchange plasty (DABC) with the basic incision (AB) as seen in the Z-plasty. Additional wide undermining and advancing of the skin around the surgical defect causes a reduction in defect size (Fig. 1B), which means that flap AB'C can be smaller than the surgical defect. Both the primary and secondary defects, were covered with a combination of transposition flap AB'C and skin sliding flap DBB' and sutured into place (Fig. 1C). If necessary, burrow triangles were excised to eliminate standing cone deformities.
Twelve weeks post-surgery, a physician observed the wounds and made objective clinical assessments. The patient and observer scar assessment scale (POSAS) was used to assess scar quality6. The POSAS consists of two separate six-item scales (observer scale and patient scale). The patient scale measures pain, itching, color, stiffness, thickness, and irregularity. Two trained dermatosurgeons assessed the observer component which measured vascularity, pigmentation, thickness, relief, pliability, and surface area. All questions are graded on a 10-point scale with one indicating the best possible score and 10 indicating the worst possible score. The scores from the six questions on the patient and observer scales were summed to be total (combined) scores ranging from 6 to 60 (6 representing normal skin and 60 representing the worst imaginable scar) for both patient and observer scales.
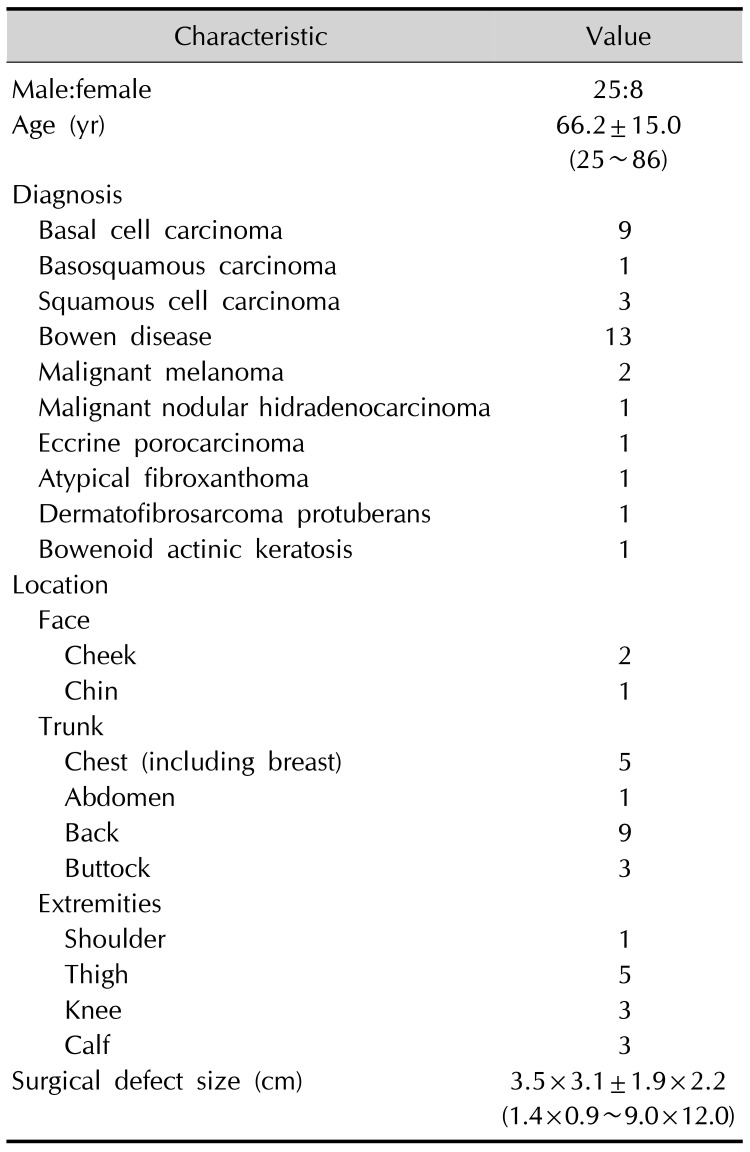
A total of 33 patients (25 male and 8 female) who underwent slide-swing skin flap reconstruction were identified. The mean age was 66.2±15.0 (range, 25~86) years. Slide-swing skin flaps were used to reconstruct surgical defects caused by the excision of Bowen disease in thirty-three cases, basal cell carcinoma in nine cases, squamous cell carcinoma in three cases, malignant melanoma in two cases, and basosquamous cell carcinoma, porocarcinoma, malignant nodular hidradenoma, dermatofibrosarcoma protuberans, atypical fibroxanthoma, and Bowenoid actinic keratosis in one case each. Tumors were located on the lower limb in eleven patients, back in nine patients, chest in five patients, face in three patients, buttock in three patients, and two patients had tumors in other locations. Surgical defects varied in size from 1.4×0.9 to 9.0×12.0 cm (mean±standard variation, 3.5×3.1±1.9×2.2 cm). Postoperative recovery was uneventful in all cases and, with the exception of focal superficial skin necrosis in several patients, there were no serious complications. Patient and defect information is summarized in Table 1.
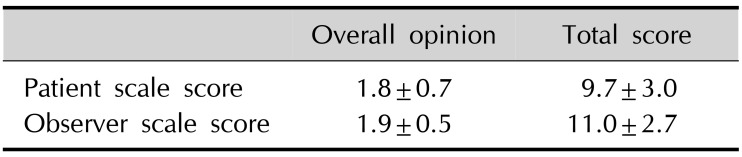
POSAS scores were collected from 29 of 33 patients. Patients responded to the scar outcomes as follows: pain (mean: 1.3), itching (mean: 1.2), color (mean: 1.7), stiffness (mean: 2.0), thickness (mean: 1.8), and irregularity (mean: 1.7). The mean patient POSAS total score was 9.7±3.0 (out of 60), and the mean patient overall opinion score was 1.8±0.7 (1 represents best possible score and 10 represents the worst possible score). Using the observer component of the POSAS, the scar outcomes were as follows: vascularity (mean: 1.9), pigmentation (mean: 1.2), thickness (mean: 1.9), relief (mean: 2.0), pliability (mean: 2.1), and surface area (mean: 1.8). The mean total observer score was 11.0±2.7 and the mean observer overall opinion score was 1.9±0.5. Lowest and highest observer scale values were 6 and 17, respectively. POSAS scores are summarized in Table 2.
The slide-swing skin flap is employed to close large round or oval defects using a combination of transposition and skin sliding. That is in part based on the principle of Z-plasty2. However, triangular skin flaps in Z-plasty are only undermined around flaps, but the slide-swing skin flap also uses the mobilization of the skin surrounding the defect. This mobilization of surrounding skin results in skin movement in all directions and exploits skin reserves around the defect, which allows the use of flaps smaller than the primary defect. There is also a difference between the slide-swing skin flap and conventional transposition flaps. The flap in the latter occurs at the midline of the defect while the former flap originate the bottom of the defect and the base of the flap is slightly wider than the apex as shown in Fig. 1A257. In addition, no further normal skin sacrifice is required, unlike the Limberg flap589. Slide-swing skin flaps may be employed on almost all parts of the body. There have been three basic types of the slide-swing skin flap. Type one is used to close a round defect. Type two uses an oblong flap to close a defect. Type three use a straight stretch of the round defect edge when forming the flap. We applied mostly type one slide-swing skin flaps because most patients had round skin lesions, type two was used for some patients with oval shaped defects. We were successfully performed at various locations on the body with good POSAS scores. Defect closure is determined by size and location, and flap size is dependent on skin elasticity39, which is greatest in the trunk, especially the flanks, back, abdomen, and buttocks. In our 33 patients, the slide-swing skin flap was applied to the trunk of 18 patients. The largest defect treated was 9.0×12.0 cm on the back of a patient with melanoma (Fig. 2). In buttock lesions, with very high (worst) observer scale POSAS scores occurred in two patients. These patients were young, physically active female in their twenties and had relatively large defects of 4.0×4.0 cm and 1.5×1.5 cm, respectively. In addition, we thought that since the buttock area is a region where there is constant tension due to sitting that the scar is likely to become hypertrophic. In limbs, skin mobility is slightly limited, but we obtained excellent results in all 12 of cases. In general, there were no serious complication and all the flaps survived well. Most patients were satisfied with the postoperative results, showing low average total POSAS scores of 9.7±3.0 and overall opinion score of 1.8±0.7. In observer scale values, the total mean POSAS score was 11.0±2.7 and mean overall opinion score was 1.9±0.5, which were not different from those of the patient group, indicating high agreement between the two groups.
This slide-swing skin flap technique has several advantages for the repair of surgical defects234. First, it can be used to cover large defects because it involves the additional mobilization of adjacent surrounding healthy skin. Second, skin grafting is not required, and it does not involve the sacrifice of healthy skin as demonstrated by Fig. 2. Third, it results in smaller surgical scars2. Finally, the flap has a broad base that ensures a good blood supply. For these reasons, we applied the slide-swing skin flap among various types of flap options. Disadvantages of the slide-swing skin flap are that skin tension at suture sites is high and trapdoor scarring can occur, which means the technique may not be appropriate on curved surfaces, such as the face or shoulder8. Nevertheless, we executed this flap successfully on the face and the shoulder (Fig. 3). In designing a flap for the face, excess tissue near the defect is more important than the relaxed skin tension line5. Available tissue is manually determined by digital manipulation (pulling or pinching) for each individual case5. In the head and neck area, the more caudal the defect, the easier it is to use this method become of the elasticity of the skin. In case of Fig. 3A, since the lesion was located on the lower cheek and the patient was aged, we executed the flap without any tension despite a large defect. In case with a shoulder defect (Fig. 3C), we massively undermined the adjacent, surrounding tissue to avoid high tension and that flap survived well without complications. The limitations of the present study include the retrospective nature, small number of patients, mainly the eldely (mean 66 years), and lack of a comparative group with other types of flaps. Therefore, further large-scale studies will be necessary including young patients and comparing multiple surgical modalities.
In summary, this study shows that the slide-swing skin flap could serve as a useful, versatile method for covering various surgical defects with good cosmetic outcomes. To the best of our knowledge, this is the first study in the dermatologic literature to evaluate the efficacy and safety of the slide-swing skin flap.
References
1. Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, Seul JH. Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg. 2012; 39:619–625. PMID: 23233887.

2. Schrudde J, Petrovici V. Slide-swing skin flap. In : Strauch B, Hall-Findlay EJ, Grabb WC, Vasconez LO, editors. Grabb's encyclopedia of flaps. Philadelphia: Lippincott;1998. p. 399–402.
3. Schrudde J, Petrovici V. The use of slide-swing plasty in closing skin defects: a clinical study based on 1,308 cases. Plast Reconstr Surg. 1981; 67:467–481. PMID: 7208690.
4. Schrudde J, Beinhoff U. Covering defects in the breast region by the slide-swing plasty. Aesthetic Plast Surg. 1989; 13:41–46. PMID: 2728998.

5. Grekin RC. Flap surgery. In : Lask GP, Moy RL, editors. Principles and techniques of cutaneous surgery. New York: McGraw Hill;1996. p. 309–328.
6. Shao K, Parker JC, Taylor L, Mitra N, Sobanko JF. Reliability of the patient and observer scar assessment scale when used with postsurgical scar photographs. Dermatol Surg. 2018; 44:1650–1652. PMID: 29381545.

7. Miller CJ. Design principles for transposition flaps: the rhombic (single-lobed), bilobed, and trilobed flaps. Dermatol Surg. 2014; 40 Suppl 9:S43–S52. PMID: 25158876.
8. Choi SM, Suh IS, Ha JW. The comparison of the clinical applicability of double z-rhomboid plasty and slide swing plasty. J Korean Soc Aesthetic Plast Surg. 1996; 2:24–31.
9. Rustemeyer J, Günther L, Bremerich A. Complications after nasal skin repair with local flaps and full-thickness skin grafts and implications of patients' contentment. Oral Maxillofac Surg. 2009; 13:15–19. PMID: 18936990.

Fig. 1
Application of the slide-swing skin flap. (A) Preoperative design of the surgical excision with safety margins and two flaps (DBB' and AB'C). (B) After tumor excision, wide undermining and additional mobilization of the adjacent skin tissue (arrows) reduced surgical defect size. (C) Postoperative view.
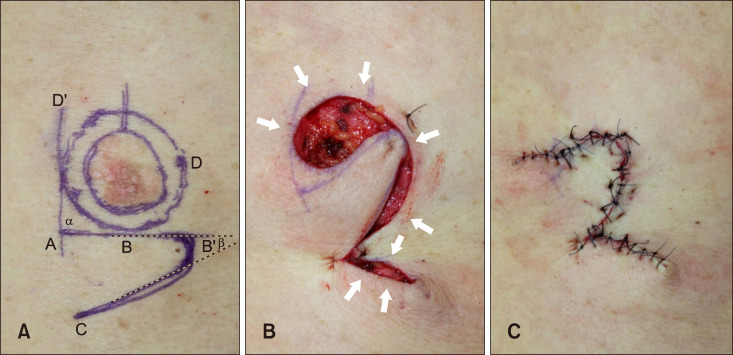
Fig. 2
A 41-year-old female with malignant melanoma on her back. (A) The lesion was 3.5×4.5 cm and the resultant surgical defect was 9.0×12.0 cm. (B) Postoperative view at 2 weeks.
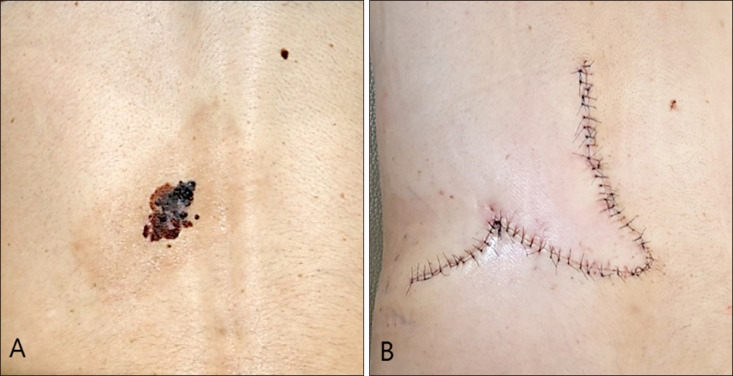
Fig. 3
An 82-year-old male with squamous cell carcinoma on his cheek. (A) The lesion was 3.0×2.6 cm. (B) Immediate postoperative view. A 70-year-old male with basal cell carcinoma on his right shoulder. (C) The lesion was 2.5×2.0 cm. (D) Postoperative view at 8 months.

Table 1
Patient and defect data




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download