This article has been
cited by other articles in ScienceCentral.
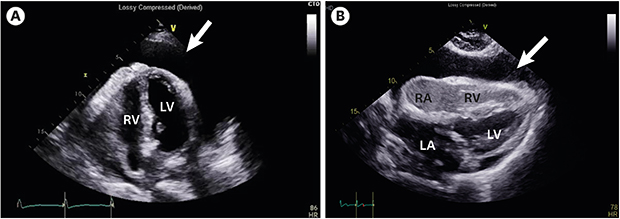
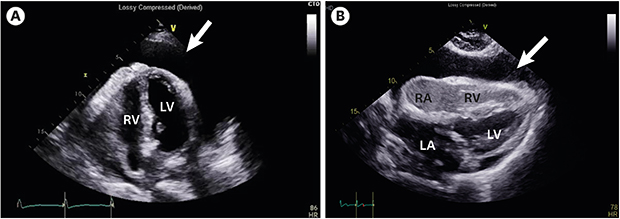
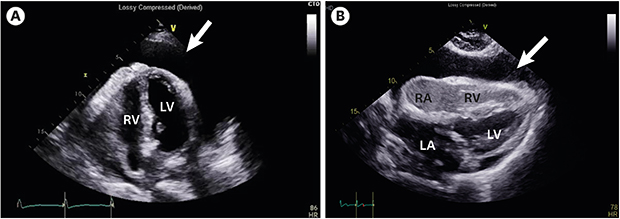
A 74-year-old woman presented with dyspnea and livedo reticularis (8 September 2016). For one month, the patient had been taking anti-tuberculosis (TB) drugs for TB pericarditis. Laboratory tests showed decreased hemoglobin (Hb) (7.3 from 11.9 g/dL) and elevated reticulocyte count (5.24%). One month prior to admission, the patient was diagnosed with TB pericarditis based on elevated (73.1 U/L) adenosine deaminase in the pericardial fluid (
Fig. 1A). On admission, echocardiography revealed a large pericardial effusion and dense spontaneous echo contrast (SEC). SEC looked like air bubbles (
Fig. 1B,
Supplementary Movie 1 and
2). Blood samples showed cold agglutination phenomenon, therefore at room temperature erythrocyte sediment rate was uninterpretable due to clumping. Levels of liver enzymes, bilirubin, inflammatory markers, electrolytes, creatinine, lactate dehydrogenase, and autoimmune antibodies were unremarkable. After one week, Hb level dropped to 6.7 g/dL and fever (38.3°C) developed, but there were no signs of infection except elevated (17.5 mg/L [normal < 5.0]) C-reactive protein. After 3 days, the patient displayed slight drowsiness. Brain magnetic resonance imaging revealed multiple embolic infarctions and microbleeds. Electrocardiography showed sustained sinus rhythm. Cold agglutinin titer was 1:128, haptoglobin was < 10 mg/dL (30–200), and direct and indirect Coombs tests were positive. Several hours later, the patient became comatose. Her Hb level dropped to 4.7 from 8.8 g/dL over 6 hours and she could not be revived.
This patient's clinical pictures (livedo reticularis, hemolysis and positive Coombs tests and cold agglutinin) imply cold agglutinin disease (CAD), presumably, rifampicin-induced. We speculate as to whether we should have stopped the suspected drug earlier and whether we should have started corticosteroid treatment or plasmapheresis, despite the absence of proven benefit. In a situation where erythrocytes aggregate regardless of cause, blood becomes echogenic because it is large enough to scatter ultrasound waves. SEC implies erythrocyte aggregation, precipitated by low shear rate and macromolecules, usually fibrinogens, in this case cold agglutinins, to overcome repulsive forces between erythrocytes.
1-3 There are only case reports about the development of autoimmune hemolytic anemia (AIHA) during TB treatment and patients with AIHA who had SEC in the right heart chambers with venous thromboembolic events.
4-6 An increased risk of thromboembolic events in CAD has been reported.
7 To the best of our knowledge, there is no report on intense SEC in drug-induced AIHA.
Ethics statement
The requirement for patient consent was waived by the Institutional Review Board of Daegu Catholic University Medical Center (CR-19-065).





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download