Abstract
Background
A history of osteoporotic fractures is strongly associated with the subsequent osteoporotic fractures. To prevent subsequent fractures, the diagnosis and treatment of osteoporosis following osteoporotic fractures are very important. A distal radius fracture (DRF) is the second most common type of osteoporotic fracture in South Korea. We analyzed the rate of osteoporosis diagnosis within 6 months post-DRF.
Methods
We used data from the Korean Health Insurance Review and Assessment Service nationwide claims database from 2010 to 2016. International Classification of Diseases, 10th revision codes and procedures codes were used to identify patients aged over 50 years with newly diagnosed DRFs; the osteoporosis assessments of these patients were then analyzed. We used Cochran-Armitage trend test to examine trends in osteoporosis diagnosis.
Results
A search of database identified 77,209 DRFs in patient aged above 50 years of age from 2011 to 2016. Among these patients, only 19,305 (25.0%) underwent diagnostic examination for osteoporosis. The number of osteoporosis examinations increased slightly, but not significantly, every year (P=0.061).
Osteoporosis and related fractures are major health concerns in the elderly.[1] Osteoporosis can result in osteoporotic fractures of the hip, spine, humerus, and wrist.[23] These osteoporotic fractures reduce the quality of life and are a major cause of hospitalization in elderly patients.[45] Patients with a history of osteoporotic fractures have a higher risk of a subsequent fracture than those without any such history.[6] To prevent subsequent osteoporotic fractures, the diagnosis and treatment of osteoporosis following osteoporotic fractures are very important.
The diagnosis of osteoporosis is the first step in its management, and involves evaluation of the bone mineral density (BMD) or quantitative computed tomography (QCT) examination.[7] The next step is prescribing anti-osteoporotic medication, such as bisphosphonate, selective estrogen receptor modulators, parathyroid hormones, and so on.[8]
A distal radius fractures (DRFs) occurs in middle-aged women and men and are a risk predictor of subsequent osteoporotic fractures.[910] DRF is the second most common type of osteoporotic fracture in South Korea.[1]
In this study, we evaluated the rate of osteoporosis examination, as the first step in osteoporosis management, among Korean patients with DRFs from 2011 to 2016.
We used healthcare utilization data from the Korean Health Insurance Review and Assessment Service (HIRA) nationwide claims database. Almost 97% of the Korean population is currently covered by this national insurance system.[1112]
The International Classification of Diseases, 10th revision (ICD-10) codes and procedure codes were used to identify patients aged over 50 years with newly diagnosed DRFs from 2010 to 2016, i.e., diagnosis codes S52.5 (fracture of lower end of radius) and S52.6 (fracture of lower end of both ulna and radius) and treatment codes N0607 and N0617 (open reduction of ulna or radius), N0603 and N0613 (open reduction of ulna and radius), N0993 (closed pinning of ulnar or radius), N0994 (closed pinning of ulnar and radius), N0983 (external fixation of forearm bone), and N0643 (closed reduction of forearm bone).
We included only one record per patient and set the wash-out period to 1 year (2010). Cases with multiple fractures were excluded from the study because of the possibility of high-energy trauma. We also excluded patients with Paget disease and cancer, and those who had undergone an osteoporosis examination before the fracture.
We determined whether each patient had undergone an osteoporosis examination within 6 months post-fracture. According to physician's guide for osteoporosis 2018,[13] it is recommend that osteoporosis patients be examined using QCT (HC 343) or dual X-ray absorptiometry (HC 341 and HC 342 for single and multiple sites, respectively).
Baseline characteristics were analyzed with the χ2 test. We used Cochran-Armitage trend test to examine trends in osteoporosis diagnosis. The statistical analyses were performed using SAS for Windows software (version 9.4; SAS Institute, Cary, NC, USA).
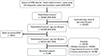
The HIRA database search revealed 702,001 DRFs from 2010 to 2016; among these, 374,073 were excluded due to duplicated data, death or patient age under 50 years. After applying the 1-year washout period, 297,911 DRFs remained, of which 77,209 that met all of the inclusion criteria were included in the final analysis (Fig. 1).
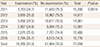
The number of DRFs treated annually decreased over time, 15,206 in 2011 to 10,778 in 2016. Of the 77,209 DRF cases, 19,305 (25.0%) underwent diagnostic examinations for osteoporosis. From 2011 to 2016, the rate of osteoporosis examination showed an increasing trend (P=0.061). The average rate of osteoporosis assessment over the 6-year period was 25.0% (Table 1).
Worldwide, osteoporosis patients undergo BMD evaluation or QCT examination. According to our data, QCT was used about 36.0% of cases in 2011, but in only 13.0% in 2016. The rate of BMD evaluation increased from roughly 64.0% in 2011 to 87.0% in 2016 (Fig. 2).
Table 2 shows the proportion of patients who underwent osteoporosis examinations within 6 months post-fractures, according to their baseline characteristics. Overall, males with fractures were less likely to undergo osteoporosis testing females (10.0% vs. 30.0%). Older patients were more likely to undergo osteoporosis examinations, especially those aged from 70 to 79 (39.9%). Patients visited a tertiary hospital had the highest rate of osteoporosis examinations (32.9%).
DRFs tend to be managed less frequently than hip and spine fractures,[14] despite the fact that they predict subsequent osteoporotic fractures.[61516] DRFs are the second most common type of osteoporotic fracture in Korea [117] and have showed the fastest rate of increase.[18] Physicians who treat DRFs should consider examination for osteoporosis.
The BMD was evaluated in less than 15% of patients with osteoporotic fractures in a retrospective cohort study conducted in Manitoba, Canada.[1920] In South Korea, the rate of BMD evaluation after osteoporotic fracture increased from 42.0% in 2005 to 53.9% in 2010.[3] In this study, we sought to determine the rate of osteoporosis assessment after DRFs in South Korea.
Two kinds of assessment are approved by the Korean HIRA for osteoporosis: BMD and QCT examination. Evaluation of the BMD at the lumbar spine and hip is currently the gold standard for diagnosing osteoporosis.[17] Compared with BMD evaluations, QCT has superior sensitivity for diagnosing osteoporosis and monitoring changes in bone density, and also allows simultaneous evaluation of the trabecular bone microarchitectural and mechanical property; nevertheless, it is still considered only as an adjunctive method, due to its high radiation dose.[21]
The rate of BMD examination after osteoporotic fractures has gradually increased according to some reports, due its ease and cost effectiveness.[322] We found that the rate of BMD examination increased from 64.0% in 2011 to 87.0% in 2016, while that of QCT examination decreased from 36.0% in 2011 to 13.0% in 2016.
Osteoporosis screening just after fractures has been performed under the Korean healthcare system for osteoporotic fracture patients since 2015.[3] However, we found that the rate of osteoporosis assessment had increased only slightly since that time. This may be because the DRF patients were younger than those with hip or spine fractures, and BMD evaluation has been shown to be performed infrequently among younger patients.[222324] Clinicians tend to be less likely to order osteoporosis examinations in patients with DRFs compared with those with hip or spine fractures. In our study, most of the DRFs occurred in patients in their 60s. Moreover, orthopedic surgeons may tend to concentrate on treating the fracture, rather than managing osteoporosis, as the first physicians to encounter patients with DRFs.[252627]
We found that female gender, medical insurance and older age were associated with a higher likelihood of osteoporosis assessment, except for patients in their 80s and above due to comorbidities and lower compliance. In addition, patients seen at larger hospitals were more likely to undergo osteoporosis assessments; in a previous study, patients seen at public health centers were most likely to undergo BMD evaluations.[22] We found that the number of examinations performed in public healthcare centers was small compared with other medical institutes, which precluded meaningful comparison. This disparity might be caused by differences in procedure codes.
Previous studies used short and long arm cast codes as procedure codes, while we thought that these codes could be used in various situations, rather than just DRFs, such as elbow fractures or triangular fibrocartilage complex injury. Patients with medical insurance tended to be examined more frequently than those under the medical benefit system, but only marginally (32.8% vs. 31.1%).
The study had several limitations. First, the incidences rates for DRFs calculated based on medical claims database might be underestimated, because such fractures are not always diagnosed and treated in healthcare institutions. In South Korea, some patients prefer traditional oriental medicine clinics or bonesetters. Second, the use of ICD-10 codes may have led to misclassification of DRFs, although to mitigate this problem we used both ICD-10 codes and procedure codes. Third, anti-osteoporosis medication use after the osteoporosis examinations was not assessed; osteoporosis treatment within 6 months post-DRFs should be evaluated in future studies.
In conclusion, this study showed osteoporosis examination are ordered at an inadequate rate in cases with DRFs. Physician who treat DRFs in patients over 50 years of age should suspect osteoporosis and order examinations accordingly.
Figures and Tables
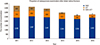 | Fig. 2The different types of osteoporosis examinations performed. BMD, bone mineral density; QCT, quantitative computed tomography. |
Acknowledgments
This study used the Korean Health Insurance Review and Assessment Service (HIRA) nationwide claims database (M20190306600). The authors would like to thank HIRA. This research was supported by the Soonchunhyang University Research Fund.
Notes
References
1. Kwon GD, Jang S, Lee A, et al. Incidence and mortality after distal radius fractures in adults aged 50 years and older in Korea. J Korean Med Sci. 2016; 31:630–634.

2. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005; 16 Suppl 2:S3–S7.

3. Park CH, Lee YK, Ha YC. Change of bone mineral density measurement among patients with osteoporotic fractures in Korean population using national claim database. J Bone Metab. 2017; 24:183–186.

4. Choi HJ, Shin CS, Ha YC, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012; 30:54–58.

5. Kwon HY, Ha YC, Yoo JI. Health-related quality of life in accordance with fracture history and comorbidities in Korean patients with osteoporosis. J Bone Metab. 2016; 23:199–206.

6. Cuddihy MT, Gabriel SE, Crowson CS, et al. Osteoporosis intervention following distal forearm fractures: a missed opportunity? Arch Intern Med. 2002; 162:421–426.

7. Mao SS, Li D, Luo Y, et al. Application of quantitative computed tomography for assessment of trabecular bone mineral density, microarchitecture and mechanical property. Clin Imaging. 2016; 40:330–338.

8. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014; 25:2359–2381.

9. Gong HS, Oh WS, Chung MS, et al. Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Joint Surg Am. 2009; 91:2376–2380.

10. Freedman BA, Potter BK, Nesti LJ, et al. Missed opportunities in patients with osteoporosis and distal radius fractures. Clin Orthop Relat Res. 2007; 454:202–206.

11. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.

12. Park SB, Kim J, Jeong JH, et al. Prevalence and incidence of osteoporosis and osteoporotic vertebral fracture in Korea: Nationwide epidemiological study focusing on differences in socioeconomic status. Spine (Phila Pa 1976). 2016; 41:328–336.

13. Korean Society for Bone and Mineral Research. 2018 Physician's guide for osteoporosis. Seoul: Korean Society for Bone and Mineral Research;2018.
14. Jung Y, Ko Y, Kim HY, et al. Gender differences in anti-osteoporosis drug treatment after osteoporotic fractures. J Bone Miner Metab. 2019; 37:134–141.

15. Rozental TD, Makhni EC, Day CS, et al. Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Joint Surg Am. 2008; 90:953–961.

16. Mallmin H, Ljunghall S. Distal radius fracture is an early sign of general osteoporosis: bone mass measurements in a population-based study. Osteoporos Int. 1994; 4:357–361.

17. Yoo JH, Moon SH, Ha YC, et al. Osteoporotic fracture: 2015 Position statement of the Korean Society for Bone and Mineral Research. J Bone Metab. 2015; 22:175–181.

18. Kim HY, Ha YC, Kim TY, et al. Healthcare costs of osteoporotic fracture in Korea: Information from the national health insurance claims database, 2008-2011. J Bone Metab. 2017; 24:125–133.

19. Giangregorio LM, Leslie WD. Time since prior fracture is a risk modifier for 10-year osteoporotic fractures. J Bone Miner Res. 2010; 25:1400–1405.

20. Metge CJ, Leslie WD, Manness LJ, et al. Postfracture care for older women: gaps between optimal care and actual care. Can Fam Physician. 2008; 54:1270–1276.
21. Burghardt AJ, Link TM, Majumdar S. High-resolution computed tomography for clinical imaging of bone microarchitecture. Clin Orthop Relat Res. 2011; 469:2179–2193.

22. Kim JW, Ha YC, Lee YK. Factors affecting bone mineral density measurement after fracture in South Korea. J Bone Metab. 2017; 24:217–222.

23. Roerholt C, Eiken P, Abrahamsen B. Initiation of anti-osteoporotic therapy in patients with recent fractures: a nationwide analysis of prescription rates and persistence. Osteoporos Int. 2009; 20:299–307.

24. Cadarette SM, Katz JN, Brookhart MA, et al. Trends in drug prescribing for osteoporosis after hip fracture, 1995-2004. J Rheumatol. 2008; 35:319–326.
25. Kim SR, Ha YC, Park YG, et al. Orthopedic surgeon's awareness can improve osteoporosis treatment following hip fracture: a prospective cohort study. J Korean Med Sci. 2011; 26:1501–1507.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download