Abstract
대상과 방법
초록
Purpose
Materials and Methods
Results
Figures and Tables
 | Fig. 2Graphs of the usefulness of diffusion-weighted MRI depending on the anatomic position (vertebral body; A and posterior element; B), evaluated by each reader (reader 1, reader 2, and reader 3). |
 | Fig. 4MR images of an 82-year-old man with prostate cancer. Sagittal T1-weighted (A), sagittal T2-weighted turbo spin-echo (B), and sagittal fat-suppressed contrast-enhanced T1-weighted MR images showing probable metastasis at T7–T9 spinal segments (C). Diffusion-weighted MR images [b = 1000 (D) and apparent diffusion coefficient map (E)] also showing probable metastasis at T7–T9 spinal segments, along with a small probable metastasis at the T3 spinal segment (arrows on D and E). Sagittal T1-weighted (A), sagittal T2-weighted turbo spin-echo (B), and sagittal fat-suppressed contrast-enhanced T1-weighted MR images showing no definite spinal metastasis at the T3 spinal segment (C).MR = magnetic resonance
|
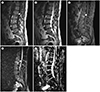 | Fig. 5MR images of a 66-year-old man with hepatocellular carcinoma.
A. Sagittal T1-weighted turbo spin-echo MR image showing a hypointense round nodular lesion (arrow) at the L2 vertebral body.
B. Sagittal T2-weighted MR image showing an isointense lesion (arrow) at the same location.
C–E. Sagittal fat-suppressed contrast-enhanced T1-weighted MR image showing peripheral enhancement of the L2 lesion (arrow on C). The patient's positron emission tomography-CT report showed this lesion as one of probable metastasis. Diffusion-weighted MR images [b = 1000 (D) and apparent diffusion coefficient map (E)] showing no diffusion restriction in the L2 lesion (arrows on D and E).
MR = magnetic resonance
|
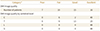
Table 1
Usefulness of DW-MRI at Each Anatomic Location

Data on the number of subjects.
*The patients were divided in 14 categories based on the total number of changes in the confidence rating (probable metastatic, equivocal, and probable benign segments) between sessions 1 (conventional, T1- and T2-weighted image, and contrast-enhanced MRI) and 2 (additional DW-MRI after conventional imaging) as follows: Category 1, decreased number of probable metastatic segments, no change in equivocal segments, or increased number of probable benign segments; Category 2, decreased number of probable metastatic segments, decreased number of equivocal segments, or increased number of probable benign segments; Category 3, no change of probable metastatic segments, decreased number of equivocal segments, or increased number of probable benign segments; Category 4, increased number of probable metastatic segments, decreased number of equivocal segments, or no change in probable benign segments; Category 5, increased number of probable metastatic segments, no change in equivocal segments, or decreased number of probable benign segments; Category 6, increased number of probable metastatic segments, decreased number of equivocal segments, or decreased number of probable benign segments; Category 7, increased number of probable metastatic segments, decreased number of equivocal segments, or increased number of probable benign segments; Category 8, decreased number of probable metastatic segments, increased number of equivocal segments, or no change in probable benign segments; Category 9, decreased number of probable metastatic segments, increased number of equivocal segments, or increased number of probable benign segments; Category 10, decreased number of probable metastatic segments, increased number of equivocal segments, or decreased number of probable benign segments; Category 11, no change in probable metastatic segments, increased number of equivocal segments, or decreased number of probable benign segments; Category 12, increased number of probable metastatic segments, increased number of equivocal segments, or decreased number of probable benign segments; Category 13, no change in probable metastatic segments, no change in equivocal segments, and no change in probable benign segments; and Category 14, all segments are probably benign in both the sessions. DW-MRI was useful in categories 1, 2, 3, 4, 5, 6, and 7. The use of DW-MRI was equivocal in categories 8, 9, 10, 11, and 12. DW-MRI was not useful in Category 13. No metastasis was presumed in Category 14.
DW-MRI = diffusion-weighted MRI
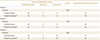
Table 2
Usefulness of Diffusion-Weighted MRI Depending on the Clinical Information and Number of Involved Segments on Conventional MRI at Each Anatomic Location

Data on the number of subjects, except when mentioned otherwise.
*Data are expressed as mean ± standard deviation, with the ranges enclosed in parentheses.
†Primary cancers, except lung and prostate or breast cancers, are classified as miscellaneous.
‡Cases of no possible radiographic or CT scan within 6 months from the MRI to evaluate the metastatic type are classified as unknown.
Table 4
Quality of DW-MRI
Data on the number of subjects.
*The patients were divided in 4 grades based on the number of spinal segments not visible on DW-MRI because of artifacts: poor (0), more than 5 segments are not visible; fair (1), 3–4 segments are not visible; good (2), 1–2 segments are not visible; excellent (3), all the spinal segments are visible.
DW-MRI = diffusion-weighted MRI, DWI = diffusion weighted image
Notes
Author Contributions
Conceptualization, K.Y.J., P.C., L.J.W.
data curation, K.Y.J., P.C., L.J.W.
investigation, K.Y.J., P.C., L.J.W.
methodology, L.E., K.Y., A.J.M., K.H.S.
project administration, L.J.W.
resources, K.Y.J., L.J.W.
supervision, L.J.W.
validation, K.Y.J.
writing—original draft, K.Y.J., L.E., L.J.W.
writing—review & editing, L.E., K.Y., A.J.M., K.H.S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download