Abstract
Purpose
A retrospective analysis of mid- to long-term clinical and radiological outcomes of Korean patients over 60 years of age who underwent hip arthroplasty using a cementless rectangular tapered stem according to Dorr proximal femur geography.
Materials and Methods
From January 2007 to December 2013, 107 patients (112 hips) underwent hip arthroplasty using the C2 stem. The mean age of patients was 77.4 years (range, 60–91 years) and the mean follow-up duration was 91.1 months (range, 60–116 months). All patients were evaluated clinically and radiologically with special attention to Dorr femoral bone classification, implant fixation, radiolucent line (RLL), and thigh pain.
Results
All implants demonstrated radiographic evidence of stable fixation by bone ingrowth without any change in position. The mean Harris hip score improved from 65.5±16.0 (preoperative) to 90.5±15.9 (final follow-up) (P<0.001). Incidence of RLLs, stress shielding, and thigh pain was highest in patients with Dorr type A (RLL, P=0.021; stress shielding, P=0.030; thigh pain, P<0.001). One stem revision was performed due to deep infection. The Kaplan–Meier survival rate of the femoral stem was 97.6%.
Conclusion
The overall survival rate of the C2 stems was greater than 97%; there were no significant differences in survival of the C2 stem according to the Dorr classification. The incidences of RLL of thigh pain and RLL were significantly different among Dorr classifications and (highest in patients with Dorr type A).
Hip arthroplasty has emerged as one of the most successful orthopedic interventions. Many long-term follow-up studies have reported clinical success including patient satisfaction, pain reduction, functional improvement, and the absence of further surgery1). Various cementless stems have been developed to improve clinical outcomes and promote firm fixation123). Cementless rectangular tapered stems, which are fixed at the femoral metaphyseal-diaphyseal junction and provide stability mediated by three-point fixation in the proximal part of the diaphysis, have shown excellent clinical results456). Recent studies have shown that cementless rectangular tapered stems are associated with improved clinical outcomes compared with cemented stems78). Importantly, however, proximal radiolucency, calcar resorption, stress shielding, and thigh pain remain possible adverse events when cementless stems are used91011). The C2 stem (LimaCorporate SpA, Udine, Italy) is a rectangular tapered stem. To date, there have been no published clinical trials for the C2 stem among elderly Asian patients.
This study was designed to retrospectively evaluate the mid- to long-term clinical and radiological outcomes in Korean patients over 60 years of age who underwent hip arthroplasty using a cementless rectangular tapered stem; we hypothesized that these outcomes may vary depending on the proximal femur geometry.
The design and protocol of this retrospective study were approved by the Institutional Review Board of Inha University Hospital (IRB No. INHAUH 2018-12-025-001). Informed consent was waived due to its retrospective nature.
A total of 107 patients (112 hips) who received hip arthroplasty using a C2 cementless femoral stem between January 2007 and December 2013 were enrolled in this retrospective study. There were 27 men (27 hips) and 80 women (85 hips) of mean age 77.4 years (range, 60–91 years). The preoperative diagnoses were fracture (n=99), avascular necrosis (n=7), and osteoarthritis (n=6). Bipolar hemiarthroplasty was performed in 90 patients and total hip arthroplasty was used in 22 hips using ceramic bearing couples (DELTA-PF cup; LimaCorporate SpA). All primary hip arthroplasties were performed through the posterolateral approach by a single experienced surgeon. The mean follow-up duration was 91.1 months (range, 60–116 months).
The C2 femoral stem used in this study has a rectangular section with sharp edges and consists of a titanium alloy (Ti6Al4V) component (6% aluminum and 4% vanadium); the entire stem surface was sandblasted except for the neck region (Fig. 1). The microstructure of such a rough surface is designed to better induce bone ingrowth1213). This stem is classified as a C3-type stem according to the Mont classification514).
Patient follow-up was conducted at six weeks, six months, one year, and annually thereafter. We estimated Harris hip score (HHS), thigh pain, complications, and stem survival rate by reviewing patient charts just after surgery (i.e., postoperative) and at final follow-up. Thigh pain was assessed by hip physicians at follow-up visits, with a particular focus on starting pain and walking pain.
One observer who had not been involved in the surgical procedures evaluated all radiographs. Preoperative radiographs were evaluated for Dorr type15), calcar-canal (CC) ratio, and cortical index (CI)16). Osteolytic lesions were recorded when they were detected during follow-up. Radiologic results (i.e., fit and fill, percentage of the canal filled by the stem at four levels) were evaluated using anteroposterior-view radiographs conducted at the five-year follow-up. These levels were named by Dorr et al.17) as calcar fill, metaphyseal fill, midstem, and distal fill. The presence of radiolucent lines (RLLs) and stress shielding were evaluated at final follow-up. The presence and extent of RLLs at the bone implant were measured according to Gruen criteria18). Stress shielding of the proximal femur was categorized into degrees of severity using Engh's classification19).
Kaplan–Meier survival analysis was performed with the end point of revision time for any reason. Statistical analysis was performed using the ANOVA test for the results of the three Dorr-type groups. Preoperative and postoperative HHS were compared using a two-sample t-test. A comparison of fit and fill between with and without RLLs was conducted using an independent t-test. A P-value <0.05 was considered statistically significant. IBM SPSS ver. 19.0 statistical software (IBM Corp., Armonk, NY, USA) was used to analyze the data.
Preoperative femoral geometry was classified using the Dorr classification system (type A [n=20], type B [n=49], type C [n=43]). RLLs were observed in Gruen zones 1, 2, and 7 in 15 hips (13.4%). Generally, the lines appeared 2 to 12 months after arthroplasty (Fig. 2, 3). After the appearance of RLL, five hips (33.3%) remained unchanged with gradual sclerotic change of the outer margin. RLLs according to Dorr type are as follows: type A (n=6), type B (n=7), and type C (n=2). Patients with Dorr type C had significantly fewer RLL (4.7%) compared to types A (30.0%) and B (14.3%) (P=0.021) Stress shielding was observed in 48 cases and there was a significant difference between Dorr types: 12 in type A (60.0%), 24 in type B (49.0%), and 12 in type C (27.9%) (P=0.030) (Table 1, Fig. 4).
Calcar fill, CC ratio, and CI were 94.39±3.16%, 0.57±0.03, and 0.53±0.04 at five-year follow-up, respectively; these values were not significantly different among patients with Dorr types A, B, and C. Metaphyseal fill, midstem fill, distal fill, and lateral proximal fill were 95.77±2.82%, 81.45±5.49%, 69.16±12.58%, and 81.32±7.54% at five-year follow-up, respectively (Table 1). In those experiencing RLL, metaphyseal fill, midstem fill, distal fill, and lateral proximal fill were 94.27±4.60%, 83.47±5.85%, 72.69±14.43%, and 83.15±8.24%, respectively. Calcar fill was significantly lower in the group with RLL compared with the non-RLL group (P=0.033) (Table 2). There were no significant differences between Dorr types and the focal osteolytic area detected in two hips in Gruen zone 1 at postoperative two years and remained without change in size until final follow-up. No changes in the position of implants, including stem subsidence, were detected in this study.
There was a significant improvement in the mean HHS at final follow-up (90.5±15.9) compared with preoperative values (65.5±16.0) (P≤0.01). Pre- and postoperative HHS did not vary significantly among Dorr types. Nine patients (8.0%) experienced occasional activity-related thigh pain that was related to Dorr type (P=0.006) and RLL (P≤0.01) (Table 1, Fig. 4). Thigh pain was relieved in all patients within two years of surgery.
Two cases of periprosthetic femoral fracture occurred during stem implantation. All hips were treated with circumferential wiring and healed without complication. Hip dislocation was noted in three hips and all cases were treated with closed reduction and hip brace fitting. One stem revision was performed due to deep infection.
Cementless stems can be divided into different categories depending on their conceptual approach (i.e., fit and fill, proximal fitting, distal taper). The rectangular tapered stem was designed to fill the proximal femur as much as possible while reducing: i) the force delivered to the distal femur and ii) the biomechanical bending stiffness with the aim of limiting postoperative stress shielding and thigh pain. The Zweymüller stem, a typical rectangular tapered stem designed in Europe, reported to provide initial stability both axially and rotationally81220). The Zweymüller stem showed excellent clinical results in older patients with Dorr type B and C femoral geometry6112122). However, other papers reported complications associated with this stem type (e.g., thigh pain, proximal radiolucency, calcar resorption, stress shielding, and subsidence)91023).
The C2 stem is very similar to the Zweymüller stem in terms of their design, shape, and surface-coating. The greatest difference between the Zweymüller stem and the C2 stem is that there is no proximal lateral shoulder in the C2 stem. Additionally, the C2 stem has: i) sharp edges and a rounded section beneath the medial neck side for increased calcar contact area and ii) a distal end with a thinner conical shape compared to other rectangular stems.
In our series, 15 cases (13.4%) experienced RLLs in Gruen zone 1 or 7. Importantly, however, these RLLs did not expand or impact stem stability. The fine motion of the femoral stem causes bone resorption, and the fibrous membrane fills the gap between the femoral stem and inner cortex. This gap appears radiolucent in plain radiography. Choy et al.24) reported that RLL (zone 3, 4, and 5) was observed in 15% of patients after performing hip arthroplasty in elderly patients using a C2 stem. Although the RLL incidence in our study (13.4%) is similar to this study, there are notable differences in the zones involved. While further studies to better understand this observation are warranted, this difference may be explained by the surgical techniques used. Patients with Dorr type C femoral geometry experienced significantly fewer RLL (4.7%) compared to those with type A (30.0%) and type B (14.3%). Dorr type A femurs have wide metaphysis and narrow diaphysis15). Because of these structural features, the rectangular tapered stem does not fit the metaphyseal-diaphyseal junction of Dorr type A femurs, which leads to the fine motion of the femoral stem and RLL.
The most common adverse event following hip arthroplasty is persistent thigh pain25). The incidence of thigh pain in patients treated with cementless femoral stems has been reported to range from 10% to 20%26). Although the cause of thigh pain has not yet been clearly defined, fixation stability and stress transfer from the femoral stem to the endocortex are two commonly cited hypotheses25262728). In our study, nine patients (8.0%) experienced occasional thigh pain that was related to activities. The incidence of thigh pain and RLL varied significantly according to Dorr type (highest in type A). These data suggest that RLL and thigh pain are associated with femoral geometry. The average bone mineral density of the proximal femur among older Asians is lower compared with the Western population2930). Therefore, the use of a small C2 stem for these patients may induce a high probability of micromotion at the proximal femur.
This study has a several limitations. First, this study is a retrospective study and thus may be subject to a selection bias. Specifically, the uneven distribution of Dorr types and over-representation of femur neck fracture among patients might bias the results. Second, this study is limited by the relatively small sample size (n=112) and lack of longer follow-up (mean, 91.1 months) to assess implant survivorship. Despite these noted limitations, we believe that the number of cases and the follow-up length were sufficient to allow for an objective analysis. This study is meaningful in suggesting a relationship between femoral geometry and thigh pain when using this kind of rectangular tapered stem in elderly Asian patients.
The clinical results of hip arthroplasties using a C2 stem revealed a stem survival rate of greater than 97%; survival rates according to Dorr classifications were not significantly different. The incidences of RLL and thigh pain were correlated to femoral geometry (highest for patients with Dorr type A). Special attention is recommended when performing hip arthroplasty using C2 stems in elderly patients with Dorr type A femoral bone classification.
Figures and Tables
 | Fig. 1C2 stem (LimaCorporate SpA, Udine, Italy); the titanium alloy (titanium, 6% aluminum, 4% vanadium) implant used in this study. © 2016 - LimaCorporate SpA. |
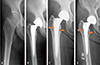 | Fig. 2(A) A 72-year-old female patient with Dorr type A. (B) The patient underwent hip arthroplasty for femur neck fracture. (C) Radiolucent lines in Gruen zone 1, 2 and 7 appeared one-year after hip arthroplasty. (D) Radiolucent lines had not progressed until seven-year after hip arthroplasty. |
 | Fig. 3(A) A 75-year-old male patient with Dorr type B. (B) The patient underwent hip arthroplasty for femur neck fracture. (C) Radiolucent lines in Gruen zone 1 and 7 initially appeared six-month after hip arthroplasty. (D) Radiolucent lines had not progressed until six-year after hip arthroplasty. |
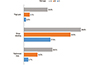 | Fig. 4Incidence of thigh pain, stress shielding, and radiolucent lines was the highest in Dorr type A (thigh pain, P≤0.001; stress shielding, P=0.030; thigh pain, P≤0.001) |
Table 1
Clinical and Radiological Results between Dorr Types

Table 2
Comparison of Fit and Fill between with and without RLLs

References
1. Simpson DJ, Kendrick BJ, Hughes M, et al. The migration patterns of two versions of the Furlong cementless femoral stem: a randomised, controlled trial using radiostereometric analysis. J Bone Joint Surg Br. 2010; 92:1356–1362.
2. Kim YH, Oh JH. A comparison of a conventional versus a short, anatomical metaphyseal-fitting cementless femoral stem in the treatment of patients with a fracture of the femoral neck. J Bone Joint Surg Br. 2012; 94:774–781.
3. Incavo SJ, Beynnon BD, Coughlin KM. Total hip arthroplasty with the Secur-Fit and Secur-Fit plus femoral stem design a brief follow-up report at 5 to 10 years. J Arthroplasty. 2008; 23:670–676.

4. Lee JM, Sim YS, Choi DS. Hip arthroplasty using the Bencox® Hip System: an evaluation of a consecutive series of one thousand cases. Hip Pelvis. 2018; 30:210–218.

5. Huo MH, Martin RP, Zatorski LE, Keggi KJ. Total hip arthroplasty using the Zweymuller stem implanted without cement. A prospective study of consecutive patients with minimum 3-year follow-up period. J Arthroplasty. 1995; 10:793–799.

7. Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M. Long-term results for the uncemented Zweymuller/Alloclassic hip endoprosthesis. A 15-year minimum follow-up of 320 hip operations. J Arthroplasty. 2009; 24:846–853.

8. Korovessis P, Repantis T. High medium-term survival of Zweymüller SLR-plus stem used in femoral revision. Clin Orthop Relat Res. 2009; 467:2032–2040.

9. Korovessis P, Repantis T, Zafiropoulos A. High medium-term survivorship and durability of Zweymüller-Plus total hip arthroplasty. Arch Orthop Trauma Surg. 2011; 131:603–611.

10. Kim HJ, Yoo JJ, Seo W, Kim MN, Kang T. Cementless total hip arthroplasty using the COREN hip system: a minimum five-year follow-up study. Hip Pelvis. 2018; 30:162–167.

11. Zweymüller KA, Schwarzinger UM, Steindl MS. Radiolucent lines and osteolysis along tapered straight cementless titanium hip stems: a comparison of 6-year and 10-year follow-up results in 95 patients. Acta Orthop. 2006; 77:871–876.

12. Delaunay C, Bonnomet F, North J, Jobard D, Cazeau C, Kempf JF. Grit-blasted titanium femoral stem in cementless primary total hip arthroplasty: a 5- to 10-year multicenter study. J Arthroplasty. 2001; 16:47–54.

13. Swanson TV. The tapered press fit total hip arthroplasty: a European alternative. J Arthroplasty. 2005; 20:4 Suppl 2. 63–67.
14. Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011; 93:500–509.

15. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242.

16. Dorr LD, Wan Z. Comparative results of a distal modular sleeve, circumferential coating, and stiffness relief using the Anatomic Porous Replacement II. J Arthroplasty. 1996; 11:419–428.

17. Dorr LD, Lewonowski K, Lucero M, Harris M, Wan Z. Failure mechanisms of anatomic porous replacement I cementless total hip replacement. Clin Orthop Relat Res. 1997; (334):157–167.

18. Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
19. Engh CA, Bobyn JD. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res. 1988; (231):7–28.

20. Grübl A, Chiari C, Giurea A, et al. Cementless total hip arthroplasty with the rectangular titanium Zweymuller stem. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2006; 88:2210–2215.

21. Schmotzer H, Clausen JD. Primary stability - the first step in successful cementless total hip replacement. In : Friedrich NF, Santore RF, editors. 25 years of biologic fixation: K. Zweymüller. München: Elsevier, Urban & Fischer;2007. p. 113–118.
22. Swanson TV. Benefits of posterior single-incision less-invasive THA using the SL-PLUS cementless stem. In : Friedrich NF, Santore RF, editors. 25 years of biologic fixation: K. Zweymüller. München: Elsevier, Urban & Fischer;2007. p. 179–190.
23. Turchetto L. Experience with the SL-PLUS system in special conditions. In : Friedrich NF, Santore RF, editors. 25 years of biologic fixation: K. Zweymüller. München: Elsevier, Urban & Fischer;2007. p. 107–111.
24. Choy WS, Ahn JH, Jeong HJ, et al. Cementless bipolar hemiarthroplasty for femoral neck fractures in elderly patients. J Korean Orthop Assoc. 2008; 43:703–709.

25. Park MS, Cho HM, Kim JH, Shin WJ. Cementless bipolar hemiarthroplasty using a rectangular cross-section stem for unstable intertrochanteric fractures. Hip Int. 2013; 23:316–322.

26. Vresilovic EJ, Hozack WJ, Rothman RH. Incidence of thigh pain after uncemented total hip arthroplasty as a function of femoral stem size. J Arthroplasty. 1996; 11:304–311.

27. Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992; 74:63–66.

28. Brown TE, Larson B, Shen F, Moskal JT. Thigh pain after cementless total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2002; 10:385–392.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download