Abstract
Intentional carbon monoxide (CO) poisoning has become rapidly increased occurrence, also if the surviving patient is burnt and unconscious, the patient's burn wound is likely to be severely deep and to need flap surgery. A 44-year-old female patient suffered from a deep contact burn to the left posterior lower leg during intentional CO poisoning. The patient underwent escharotomy and treatment with a latissimus dorsi muscle neuro-vascularized free flap and scalp skin grafts. While harvesting 0.008 inches (300 cm2) of the scalp skin, some 25 cm2 of the skin was accidentally harvested as a thick split-thickness skin graft (SSG) from the right occipital scalp. Interfollicular epidermal and dermal regeneration was achieved at eleven days postoperatively at the thick SSG donor site. The patient's deep burn wound was reconstructed by two staged surgeries. The patient was able to walk with the help of a supportive shoe one year postoperatively.
In recent decades, suicide by burning coal briquettes and barbecue charcoal, which causes carbon monoxide (CO) poisoning, has increased rapidly in East Asia12. Intentional CO poisoning by burning coal briquettes occurs in enclosed spaces in residential areas.
The consciousness of the patient in the current case could be recovered within the ambulance due to the early detection of her condition by her housemate while she was attempting suicide in the bathroom. During unconsciousness caused by CO poisoning, a burning charcoal briquette contacted the posterior aspect of her left lower leg, resulting in a severe burn injury.
The authors attempted to use an latissimus dorsi (LD) muscle neuro-vascularized free flap to restore the muscle defects in the posterior-lateral aspect of the left lower leg and scalp split-thickness skin grafts (SSGs) to cover the transferred muscle after escharectomy of the burn wound. During scalp graft harvest, a thick scalp wound (25 cm2) at the donor site occurred partially due to a loosened dermatome screw. However, this wound achieved early scarless healing.
This study presents a case of a lower leg salvage procedure being performed using an LD muscle neurovascularized free flap and scalp SSGs, followed by the early and scar-less regenerative healing of a scalp donor site after the harvest of a thick (0.035-inch) SSG. An IRB (No. 2018-10-001) waiver for this case report was obtained from Bestian Seoul Hospital in Seoul, Republic of Korea. The patient provided written informed consent for the publication and the use of her images.
A 44-year-old female patient was hospitalized with a severe burn on the left posterior lower leg. While attempting to commit suicide by burning charcoal briquettes in an enclosed bathroom, the patient was rendered unconscious by the CO gas generated from the burning briquettes; the posterior aspect of her left lower leg contacted a burning briquette, which resulted in a severe burn. She was able to recover consciousness due to the early detection of her condition by her housemate during the suicide attempt.
The patient underwent fasciotomy in the emergency room, and damage to the posterior and lateral compartment muscles of the left lower leg was confirmed, but the circulation in the anterior skin, ankle and foot of the left lower leg was not compromised (Fig. 1). Computed tomography and magnetic resonance imaging (Fig. 2) of the left lower leg showed extensive damage to the muscles, except for portions of the medial soleus, anterior tibialis and posterior tibialis muscles.
The patient's scalp was shaved before the procedure and shampooed with povidone solution. Under endotracheal general anaesthesia, the damaged tissues of the left posterior and lateral compartments, except suspicious tissues in the anterior compartment of the left lower leg, were debrided a sural artery, two sural veins and motor branch of a tibial nerve to be connected to the damaged gastrocnemius muscle at the popliteal fossa were prepared as recipient pedicles for a muscle free flap.
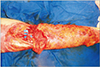
A large portion of the LD muscle (30×15 cm2 in size), including pedicles of a thoracodorsal artery, two thoracodorsal veins and a thoracodorsal nerve, was harvested from the left thorax. Microanastomosis of one artery, two veins and nerve between the donor and recipient pedicles were performed using 9-0 nylon sutures under 3.5× loupe magnification. The LD muscle free flap was used to cover the debrided wound of the posterior aspect of the left lower leg (Fig. 3).
Three scalp SSGs (0.008 inches thick, 300 cm2) were harvested from the frontal, parietal-vertex and occipital scalp. The scalp harvested from the right occipital area was accidentally harvested as a thick SSG (25 cm2) due to the loosening of a screw in the Zimmer® Air Dermatome (Zimmer, Inc., Warsaw, IN, USA) plate, and the donor wound surface was yellowish in colour and showed severed hair follicle units. The muscle flap was covered with meshed (1:3) scalp SSGs. The surgical wounds were dressed with Bactigras (Smith & Nephew Medical Suzhou, Ltd., Suzhou, China), antibiotic ointment, gauze, and elastic bandages. The left lower leg underwent long splinting with the knee extended and the ankle at a right angle.
The differences between the thickness of the grafts determined by histology and the adjusted thickness of the dermatome were compared. Setting the dermatome to a skin graft thickness of 0.008 inches yielded a graft with a histological thickness of 0.007 inches, and the thick skin graft harvested at the incorrect depth setting was 0.035 inches thick (Fig. 4), while using a depth setting of 0.016 inches yielded a re-harvested skin graft with a thickness of 0.012 inches.
Interfollicular epithelization was achieved at the scalp donor sites at nine days postoperatively for the 0.007-inch-thick harvest wounds and at eleven days postoperatively for the 0.035-inch-thick harvest wound (Fig. 5). The normal thickness of the scalp in the contralateral occipital area measured by ultrasonography (Esaote MyLab™One, Genoa, Italy) was 1.3 mm (0.051 inches) after surgery.
The distal part of the free muscle flap developed partial necrosis, and inflammatory discharge was drained through a tunnel between the muscle flap and the exposed fibular bone. The opening tunnel through the incision and elevation of the lateral margin of the muscle flap was repeatedly debrided with a fibular resection 15 cm in length to remove the residual injured extensor muscles of the anterior compartment and granulation tissue (Fig. 6). The remaining surface wounds were covered with a reharvested vertex skin sheet (100 cm2) at sixty-four days postoperatively.
Histological examination of a punch biopsy of the scalp donor site confirmed the regeneration of the epidermis and dermis at sixty-four days after the harvest of the thick 0.035-inch skin graft (Fig. 7). The harvested thick scalp SSG was 69% as thick as the normal scalp skin (0.035/0.051 inches).
The donor area of the LD muscle flap showed a long linear scar without significant functional impairment. The donor site of the thick scalp SSG achieved inconspicuous scar-less healing with good hair growth (Fig. 8), and the posterior lower leg wound healed with functioning LD muscle without limitations to the motion of the left knee (Fig. 9, 10). The patient's left leg and foot were supported by footwear with a steel ankle guard for walking due to ankle and foot motion restrictions after wound healing one year after surgery.
Over the past two decades, the use of coal briquettes in the home has decreased sharply, but in some homes, coal briquettes are still used as a heat source, and they are widely used for cooking in restaurants. Therefore, they are easy to buy at local stores in Korea. Intentional or unintentional CO poisoning can lead to severe, deep burns incurred while unconscious. Therefore, those related to CO poisoning have been reconstructed with various flaps3.
Posterior compartment leg defects can be reconstructed with a functional LD muscle free flap4. Our patient sustained severe, deep contact burns in all muscles of the left lower leg except for portions of anterior compartment muscles, the medial part of the gastrocnemius and soleus muscles and portions of deep posterior compartment muscles, and the defects were covered with a functional LD muscle free flap and scalp SSG. A functional LD muscle free flap was selected among the other flaps to restore the wide muscle deficit of the debrided wound (30×15 cm2). The LD muscle neuro-vascularized free flap restored the contraction function in the knee flexion position one year after surgery.
Crawford5 first attempted to use the scalp for skin grafts to treat an extensive deep burn. Scalp SSGs have been used in the treatment of acute burns and in burn-related reconstruction surgeries and have rarely been used for the coverage of traumatic wounds or tumour excision defects678. Complications of the harvest of scalp SSGs from the hairy scalp skin have been reported to include alopecia, concrete scalp deformity and tufted scar deformity at the scalp donor site, as well as hair transfer at the recipient site. Previous reports have evaluated the results of using a scalp SSG based on the thickness of the dermatome depth setting without measuring the normal scalp thickness or the histological thickness of the scalp SSG678. A number of hypotheses have been proposed to explain the difference between the dermatome thickness setting and the measured skin graft thickness9. The histological thickness of the thigh SSG in paediatric patients represents a wide range of thicknesses around a median value close to the depth setting of the dermatome10.
The authors compared the thickness of the dermatome depth setting with the thickness measurement of the SSG biopsy. The difference facilitated judgement of the depth of the scalp donor site wound. In addition, the normal thickness of the donor skin was examined by non-invasive ultrasonography.
During graft harvest, a full-thickness skin flap was elevated due to the accidental loosening of a dermatome screw, and the repeated or excessively deep harvest of full-thickness scalp wounds can result in global alopecia68. The thickness of the accidentally grafted skin in this case was measured by histology to be 0.035 inches (0.89 mm), and the thickness of the contralateral occipital normal scalp was measured by ultrasound to be 0.051 inches (1.3 mm). Thus, the skin harvested in this accident was considered a thick scalp SSG. The donor site of this accidentally thick scalp SSG achieved inconspicuous scar-less healing.
In conclusion, a severe contact burn of the lower leg that occurred during intentional CO poisoning was salvaged using an LD muscle neuro-vascularized free flap and meshed and re-harvested sheet scalp SSGs. After the harvest of a thick SSG, the scalp donor sites suggested the possibility of treatment without hypertrophic scarring, different from other donor sites.
Figures and Tables
 | Fig. 1Fasciotomy of a severe burn wound involving the deep muscles of the posterior aspect of the left lower leg. |
 | Fig. 2Water-fat saturated T1-weighted magnetic resonance imaging of the proximal 1/3 of the left lower leg showing the border of the muscle damage marked with arrowheads. |
 | Fig. 4Thick skin graft with a histological thickness of 0.035 inches harvested at an incorrect depth setting (H&E, ×40). |
 | Fig. 5Scalp wound of the 0.035-inch-thick split-thickness skin graft donor site in the right occipital area showing complete epithelization 11 days after surgery. |
 | Fig. 6Re-exploration of the wound showing granulation tissue under the surface of the free flap, residual damaged muscle in the anterior compartment and exposed fibular bone 64 days after the first surgery. |
 | Fig. 7Regenerated tissue of the deep donor wound 64 days after surgery (H&E, ×12.5); arrowheads mark the border between residual reticular and regenerated fibrotic tissue. |
References
1. Chang SS, Chen YY, Yip PS, Lee WJ, Hagihara A, Gunnell D. Regional changes in charcoal-burning suicide rates in East/Southeast Asia from 1995 to 2011: a time trend analysis. PLoS Med. 2014; 11:e1001622.

2. Choi YR, Cha ES, Chang SS, Khang YH, Lee WJ. Suicide from carbon monoxide poisoning in South Korea: 2006-2012. J Affect Disord. 2014; 167:322–325.

3. Chai J, Song H, Sheng Z, Chen B, Yang H, Li L. Repair and reconstruction of massively damaged burn wounds. Burns. 2003; 29:726–732.

4. Rednam RS, Rinker BD. Reconstruction of posterior compartment of lower extremity using a functional latissimus dorsi free flap: a case report. Microsurgery. 2016; 36:77–80.

6. Gyger D, Genin B, Bugmann P, Lironi A, Coultre CL. Skin harvesting on the scalp in children: utopia or reality. Eur J Pediatr Surg. 1996; 6:166–169.

7. Weyandt GH, Bauer B, Berens N, Hamm H, Broecker EB. Split-skin grafting from the scalp: the hidden advantage. Dermatol Surg. 2009; 35:1873–1879.
8. Chang LY, Yang JY, Chuang SS, Hsiao CW. Use of the scalp as a donor site for large burn wound coverage: review of 150 patients. World J Surg. 1998; 22:296–299. discussion 299-300.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download