Abstract
Backgrounds/Aims
Pure laparoscopic living donor right hemihepatectomy (PLDRH) has been performed in many experienced centers. However, portal vein variations still remain challenging thus disturbing the widespread of PLDRH in many centers. PLDRH when integrated with 3-dimensional laparoscopy and indocyanine green (ICG) near-infrared fluorescence cholangiography is safe and feasible.
Methods
We reviewed 19 donors with separated right anterior and right posterior portal veins who underwent living donor right hemihepatectomy between January 2014 and December 2016. We compared the clinical outcomes of PLDRH and conventional open right hemihepatectomy (CDRH).
Results
6 donors (31.6%) underwent PLDRH while 13 donors (68.4%) underwent CDRH. There was no intraoperative complications, transfusions and open conversions in the PLDRH donors. The total operative time was longer in PLDRH (356.5 vs. 244.5 minutes, p=0.003). However, the length of hospital stay (8.5 vs. 9.0 days, p=0.703), blood loss (450.0 vs. 393.6 ml, p=0.557) and complication rate (16.6% vs.27.3%; p=0.327) did not differ between the two groups.
Laparoscopic surgery is widely and diversely utilized in various surgical areas providing several advantages compared to open surgery in terms of faster postoperative recovery, shorter hospital stays, and better cosmetic outcomes.12 Laparoscopic hepatectomy has developed relatively slowly compared to other abdominal surgeries due to the long learning curve, technical difficulties, risk of bleeding and questionable long-term outcomes. However, recent studies have reported excellent results of laparoscopic liver resection. Since then, utilization of laparoscopy in liver resection has gradually expanded.34
Great concerns have been raised regarding the application of pure laparoscopic living donor hepatectomy in living donor liver transplantation. This is attributed to the technical challenges of the procedure and concerns regarding donor safety.5 Several studies from highly specialized centers reported satisfactory outcomes of pure laparoscopic living donor hepatectomy for adults. However, most of these studies are based on donors selected under strict selection criteria.6789
Anatomical variations of the portal vein represent a major obstacle to pure laparoscopic donor hepatectomy. Type II and III variations of the right portal vein represent a major obstacles in donor surgery and can be a reason for donor exclusion since additional manipulations of the liver graft is required such as venoplasty or grafting. In addition, bile duct variation can also be accompanied.
Due to advances in laparoscopic equipment such as 3-dimensional (3D) flexible scope and indocyanine green (ICG) near-infrared fluorescence cholangiography, laparoscopic donor surgery has become a safe alternative to routine open donor hepatectomy.
The aim of this study is to evaluate the safety and feasibility of pure laparoscopic donor right hemi-hepatectomy (PLDRH) in donors with type II and III portal vein anatomic variations compared to conventional open donor hemi-hepatectomy (CDRH).
Donors with separate anterior and posterior portal veins who underwent living-donor right hemihepatectomy at Seoul National University Hospital (SNUH), South Korea from January 2014 to December 2016 were retrospectively reviewed and analyzed. The clinical outcomes of donors who underwent PLDRH and CDRH groups were compared. This study was approved by the institutional review board at SNUH. Informed consent was waived by the IRB due to the retrospective study design.
The donor evaluation process practiced at Seoul National University Hospital is described in details elsewhere.1011 Dynamic triphasic computed tomography (CT) and magnetic resonance cholangiography (MRCP) using specific contrast media (PRIMOVIST) were taken to confirm the preoperative anatomic variation.
The surgical technique of PLDRH has been described elsewhere.11 The donor was placed supine, with legs apart, in the reversed Trendelenburg position. The surgeon stands between the donor's legs, and the assistant and camera operator stand on the donor's left side. Pneumoperitoneum was established and maintained at 12 mmHg. Four 12-mm trocars and 15-mm trocar were inserted.
While viewing with the Endoeye Flex 3D laparoscope (Olympus, Tokyo, Japan), the right liver was mobilized by dividing the round, falciform, right coronary and triangular ligaments with the Thunderbeat (Olympus Tokyo, Japan). The middle hepatic vein (MHV) and right hepatic vein (RHV) were exposed from above. The right portion of segment I was mobilized to enable dissection of the anterior aspect of the inferior vena cava (IVC) by dividing small venous branches with intracorporeal ties or endoclips. The right inferior hepatic vein was divided using Hem-O-Lok clips (Weck Closure System, Research Triangle Park, NC) or transected later with the RHV using an endostapler (Echelon Flex Powered Vascular Stapler, Ethicon, Somerville, NJ) if the size was considered large enough for anastomosis. The area between the liver and IVC was carefully dissected as high as possible, followed by insertion of the Goldfinger (Ethicon Endosurgery, Cincinnati, OH) to create a tunnel. A nelaton tube was inserted through the tunnel to lift the cutting area of the liver in the posterior-to-anterior direction. After dividing the cystic artery and duct, the right side of the hilum was exposed and dissected. The right hepatic artery (RHA) and right portal vein (RPV) branches were identified. The exact transection plane of the liver is determined by ICG near-infrared fluorescence camera (PINPOINT Endoscopic Fluorescence Imaging System, NOVADAQ, Mississauga, ON, Canada).
The superficial layer of the liver parenchyme is divided using an energy device (Thunderbeat, Olympus, Tokyo, Japan). The deep portion of the parenchyme is transected by cavitron ultrasonic suction aspirator (CUSA®, Valleylab, Inc., Boulder, CO, USA) along the MHV. Larger veins draining segments V and VIII are preserved, clipped and divided to be reconstructed on the back table.
Real-time ICG near-infrared fluorescence cholangiography is used to identify the ideal transection point of the right hepatic ducts (RHDs). The liver graft is placed in a laparoscopic endo-bag (LapBag®, Sejong Medical Co., Ltd., Gyeonggi-do, Korea). Pfannenstiel incision is prepared at the suprapubic area allowing for future extraction of the graft. First, the RHA is clipped and divided. Then, the RPV branches are divided with laparoscopic stapler. Finally, the main RHV and the IVC ligament are divided with laparoscopic vascular staplers. The liver graft is extracted through the pre-made Pfannenstiel incision.
The Pfannenstiel incision is closed and re-insufflation is done. The resection surface and vascular and bile duct stumps are checked for bleeding or bile staining. Fibrin glue sealant (Greenplast, Green Cross Corp., Seoul, Korea) is applied to the cut surface of the liver and bile duct stumps. The remnant left liver is then fixed by suturing the divided falciform ligament.
On the back table, Y-graft from recipient is used in case there is a distance between the right anterior portal vein and right posterior portal vein as in type III and direct venoplasty was performed in trifurcations like Type II or relatively close distance in Type III.
Continuous variables were compared using Student's t test and categorical variables using by the chi-square test or Fisher's exact test, as appropriate. Continuous variables are expressed as median value with range or mean value with standard deviation while categorical variables are expressed as numbers and percentages. A two-tailed p value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS software version 22.0 (SPSS Inc., Chicago, IL).
During the study period, 19 donors with type II or type III portal vein variations underwent living donor right hemihepatectomy and were included in this study. Six donors (31.6%) underwent PLDRH, while 13 donors (68.4%) underwent CDRH.
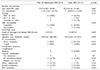
Table 1 summarizes the baseline characteristics of both groups. There was no significant difference between laparoscopic and open living donors.
Table 2 summarizes the operative outcomes of both groups. There was no significant difference between the open and laparoscopic groups, except the operative time. The total operative time was longer in the laparoscopic group (356.5 vs. 262.8 minutes, p=0.02). None of the donors had intraoperative complications and none required perioperative transfusions. Most donors with type II or type III portal vein variations also had multiple bile duct opening regardless of the surgical approach (83.3% vs. 76.9%, p=0.627). There was no significant difference in the overall complication rate between the two groups (16.7% vs. 27.3%, p=0.627) and the biliary complication rate was also insignificant (16.7% vs. 15.4%, p=0.316). All donors fully recovered without further complications and there was no reoperation or readmission.
The baseline characteristics and perioperative outcomes of the recipients are described in Table 3. There was no significant difference between the two groups regarding baseline clinical characteristics including age, sex, etiology, Child-Pugh and MELD score. In the PLDRH group, Y-grafts were used in thee (50%) recipients and three (50%) recipients underwent direct venoplasty. Y-grafts were used in seven (53.8%) recipients in the CDRH group while direct venoplasty was performed six (46.2%) recipients.
There was no significant difference in the operative time between the two groups (356.5 vs 244.5, p=0.076). One (16.7%) patient in the PLDRH group and two (15.4%) patients in the CDRH group underwent vascular intervention due to portal vein stenosis and/or thrombosis.
LDLT is considered a safe alternative to deceased donor liver transplantation. Although a lifesaving procedure, any harm to the donor is unacceptable. With improvements in surgical techniques and perioperative patient care, adult donor hepatectomy has become a safe procedure with acceptable outcomes. However, living donor hepatectomy still remains a major surgical procedure entailing unpredictable morbidities.11213 Most living donors have great concern that related with the large abdominal scar for CDRH. This sometimes caused a lot of psychological stresses affecting their decision to donate. In addition, the excess postoperative pain prolongs the hospital stay and delays their postoperative recovery.12
PLDRH was first reported by Soubrane et al. in 2013.14 Yet, unlike other abdominal surgeries, the expansion of PLDRH has been very slow. Various concerns have been raised regarding the safety of PLDRH. The second international consensus on left lateral sectionectomy held in Morioka addressed that PLDRH is in the developmental phase with unclear benefit-to-risk ratio and that the long-term outcomes of both the donor and recipient is unknown.5
Several studies from highly specialized centers reported satisfactory outcomes of PLDRH. However, these studies emphasized the importance of careful selection of appropriate donors for this approach. Furthermore, most of these studies report that donors with portal vein or hepatic duct anatomical variations or marginal liver grafts are considered unsuitable for PLDRH.6789 PLDRH was first performed in 2015 at the SNUH.15 The center is highly experienced in adult LDLT with different anatomical variations providing excellent outcomes. At the same time, laparoscopic hepatectomy for hepatic neoplasm is frequently performed at this center with great experience. This allowed for the easy and rapid adoption of PLDRH. With accumulating experience, more than 90% of PLDRH are currently performed via pure laparoscopic approach.816
In this study, the safety and feasibility of PLDRH in donors with type II and III portal vein variations has been evaluated. This is the first report that compares laparoscopic and open donor hepatectomy in donors with type II or III variations of portal vein.
PLDRH requires a cautious technique to achieve the complex balance between donor safety and sufficient graft quality. The key to success in PLDRH is the technical standardization of the procedure. The key features are the use of flexible 3D scope and ICG near-infrared fluorescence cholangiography.816 In this study, there was no significant difference between open and laparoscopic approaches regarding various operative variables except for the operative time. The total operative time was longer in laparoscopic approach compared to the standard open approach (356.5 vs. 262.8 minutes, p=0.02). This is related to the learning curve of the laparoscopic approach during the transition from open right hepatectomy to PLDRH. With accumulating experience, shorter operation time was accomplished.
Donor safety in LDLT is the main goal in any donor surgery. A living donor is a healthy person who is intentionally exposed to major a surgical procedure, in which a dominant proportion of their liver is resected. Therefore, any harm to these living donors is unacceptable. In this study, none of the donors experienced intraoperative complications and none required perioperative transfusions.
While there was no harm observed or documented in living donors, there was no significant difference between open and laparoscopic approaches in respect to postoperative hospital stay and complication rate. All donors fully recovered without any postoperative complications. Donors with dual portal vein variations were commonly associated with bile duct variations. The biliary complication rate in the study donors was relatively higher in both groups when compared with those without variation. However, the biliary complications rates were similar in both groups (16.6% vs. 27.3%, p=0.327).
The graft quality in laparoscopic donor hepatectomy may be inferior compared to its open counterpart in regards to the graft vasculature length. Therefore, the presence of a highly skilled recipient team is essential to allow for safe graft implantation. In this study, in the PLDRH group, Y-grafts were used in three recipients and direct venoplasty was performed in three other recipients. In the CDRH group, Y-grafts were used in seven recipients in the CDRH group and direct venoplasty was performed in six recipients. One patient in the PLDRH group and two patients in the CDRH group underwent vascular intervention due to portal vein stenosis and/or thrombosis. These recipients fully recovered after the radiological interventions.
This study has some limitations. First, the number of donors included is small. However, this issue is related to the lack of PLDRH in donor with anatomic variations. Moreover, the retrospective nature of the study may have some selection bias. This is related to that the cases with anatomical variation tends to be easily approached by the conventional open approach. In addition, this study is a single center experience with considerable experience in open liver surgery and LDLT.
In conclusion, PLDRH is a technically challenging procedure requiring several complex laparoscopic techniques. The presence of portal vein variations adds on further challenges. The current series support the safety and feasibility of PLDRH for donors with type II and III portal vein variations by surgeons with great experience in laparoscopic hepatobiliary surgery and LDLT.
Figures and Tables
Table 1
Comparison of preoperative characteristics between pure 3D laparoscopic and conventional open donor right hemi-hepatectomy

Table 2
Comparison of postoperative outcomes between pure 3D laparoscopic and conventional open donor right hemi-hepatectomy

References
1. Samstein B, Griesemer A, Halazun K, Kato T, Guarrera JV, Cherqui D, et al. Pure laparoscopic donor hepatectomies: ready for widespread adoption? Ann Surg. 2018; 268:602–609.
2. Au KP, Chok KSH. Minimally invasive donor hepatectomy, are we ready for prime time? World J Gastroenterol. 2018; 24:2698–2709.
3. Takahara T, Wakabayashi G, Beppu T, Aihara A, Hasegawa K, Gotohda N, et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci. 2015; 22:721–727.
4. Han HS, Shehta A, Ahn S, Yoon YS, Cho JY, Choi Y. Laparoscopic versus open liver resection for hepatocellular carcinoma: case-matched study with propensity score matching. J Hepatol. 2015; 63:643–650.
5. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–629.
6. Han HS, Cho JY, Yoon YS, Hwang DW, Kim YK, Shin HK, et al. Total laparoscopic living donor right hepatectomy. Surg Endosc. 2015; 29:184.
7. Kim KH, Kang SH, Jung DH, Yoon YI, Kim WJ, Shin MH, et al. Initial outcomes of pure laparoscopic living donor right hepatectomy in an experienced adult living donor liver transplant center. Transplantation. 2017; 101:1106–1110.
8. Lee KW, Hong SK, Suh KS, Kim HS, Ahn SW, Yoon KC, et al. One hundred fifteen cases of pure laparoscopic living donor right hepatectomy at a single center. Transplantation. 2018; 102:1878–1884.
9. Soubrane O, Kwon CH. Tips for pure laparoscopic right hepatectomy in the live donor. J Hepatobiliary Pancreat Sci. 2017; 24:E1–E5.
10. Yi NJ, Suh KS, Cho JY, Lee HW, Cho EH, Yang SH, et al. Three-quarters of right liver donors experienced postoperative complications. Liver Transpl. 2007; 13:797–806.
11. Lee KW, Kim SH, Han SS, Kim YK, Cho SY, You T, et al. Use of an upper midline incision for living donor partial hepatectomy: a series of 143 consecutive cases. Liver Transpl. 2011; 17:969–975.
12. Abecassis MM, Fisher RA, Olthoff KM, Freise CE, Rodrigo DR, Samstein B, et al. Complications of living donor hepatic lobectomy--a comprehensive report. Am J Transplant. 2012; 12:1208–1217.
13. Brige P, Hery G, Chopinet S, Palen A, Azoulay D, Gregoire E. Morbidity and mortality of hepatic right lobe living donors: systematic review and perspectives. J Gastrointestin Liver Dis. 2018; 27:169–178.
14. Soubrane O, Perdigao Cotta F, Scatton O. Pure laparoscopic right hepatectomy in a living donor. Am J Transplant. 2013; 13:2467–2471.
15. Suh KS, Hong SK, Yi NJ, Lee KW, Kim HS, Yoon KC, et al. Pure 3-dimensional laparoscopic extended right hepatectomy in a living donor. Liver Transpl. 2016; 22:1431–1436.
16. Suh KS, Hong SK, Lee KW, Yi NJ, Kim HS, Ahn SW, et al. Pure laparoscopic living donor hepatectomy: focus on 55 donors undergoing right hepatectomy. Am J Transplant. 2018; 18:434–443.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download