This article has been
cited by other articles in ScienceCentral.
Abstract
This study was performed to describe the longitudinal management of recurrent temporomandibular joint (TMJ) ankylosis from infancy to adulthood in perspective of surgical and orthodontic treatment. A 2-year-old girl was referred with chief complaints of restricted mouth opening and micrognathia due to bilateral TMJ ankylosis. For stage I treatment during early childhood (6 years old), high condylectomy and interpositional arthroplasty were performed. However, TMJ ankylosis recurred and symptoms of obstructive sleep apnea (OSA) developed. For stage II treatment during early adolescence (12 years old), gap arthroplasty, coronoidectomy, bilateral mandibular distraction osteogenesis, and orthodontic treatment with extraction of the four first premolars were performed. However, TMJ ankylosis recurred. Because the OSA symptoms reappeared, she began to use a continuous positive airway pressure device. For stage III treatment after completion of growth (20 years old), low condylectomy, coronoidectomy, reconstruction of the bilateral TMJs with artificial prostheses along with counterclockwise rotational advancement of the mandible, genioglossus advancement, and orthodontic treatment were performed. After stage III treatment, the amount of mouth opening exhibited a significant increase. Mandibular advancement and ramus lengthening resulted in significant improvement in the facial profile, Class I relationships, and normal overbite/overjet. The OSA symptoms were also relieved. These outcomes were stable at the one-year follow-up visit. Since the treatment modalities for TMJ ankylosis differ according to the duration of ankylosis, patient age, and degree of deformity, the treatment flowchart suggested in this report could be used as an effective guideline for determining the appropriate timing and methods for the treatment of TMJ ankylosis.
Keywords: Temporomandibular joint ankylosis, Distraction osteogenesis, Reconstruction, Artificial prosthesis
INTRODUCTION
The onset of temporomandibular joint (TMJ) ankylosis at early age can result in severe functional and esthetic problems, including limited mouth opening, mandibular retrusion, and facial asymmetry.
123 In order to minimize these problems, TMJ ankylosis should be treated as soon as it is detected.
4 Condylectomy, gap arthroplasty, interpositional arthroplasty, mandibular distraction osteogenesis (MDO), and TMJ reconstruction have been used as treatment modalities for TMJ ankylosis.
Although condylectomy and gap arthroplasty can result in pseudo-articulation, these procedures have some side effects such as anterior openbite in bilateral cases, premature contact on the affected side and openbite on the unaffected side in unilateral cases, and recurrent TMJ ankylosis.
5 For prevention of re-ankylosis, interpositional arthroplasty has been performed using autogenous grafts (e.g., temporal muscle flap, dermis fat) or alloplastic materials (e.g., acrylic, silastic).
6 However, gradual collapse of the gap by contraction forces from the masticatory muscles can also lead to recurrent TMJ ankylosis.
6
MDO in conjunction with arthroplasty can transport the osteotomized bone toward the area of the glenoid fossa. The soft tissue between the transported segment and the glenoid fossa area can function as a new disc.
789 However, it is controversial whether MDO can be performed simultaneously with arthroplasty.
Conventional TMJ reconstruction involves the surgical removal of ankylosed bone and replacement with an autogenous bone graft (e.g., costochondral, clavicular, or metatarsal bone). A costochondral graft offers advantages in terms of its morphological similarity with the condyle and capacity for regeneration and growth.
3 However, this procedure has some limitations, including donor site morbidity, an unpredictable growth pattern, and re-ankylosis.
10 If patients have a history of previous TMJ surgeries and recurrent TMJ ankylosis, TMJ reconstruction using an artificial prosthesis can be adopted as an alternative approach.
111213
In order to understand the treatment flow for TMJ ankylosis, it is necessary to perform longitudinal followup for patients with recurrent ankylosis despite a series of conventional surgical treatments. Here we describe the longitudinal management of recurrent TMJ ankylosis in a young girl from infancy to adulthood in perspective of surgical and orthodontic treatment.
CASE REPORT
Patient
A 2-year-old infant girl visited the Department of Orthodontics, Seoul National University Dental Hospital, Seoul, South Korea. The patient exhibited a convex profile and a large overjet (5.0 mm) (
Figure 1 and
Table 1). The maximum mouth opening was 7 mm due to the bony ankylosis in both TMJs. Trauma during delivery or after birth was suspected to be the cause of ankylosis in this patient because there was no history of infection in the medical record.
Lateral cephalometric analysis exhibited a skeletal Class II relationship (ANB, 13.0°), mandibular retrusion (SNB, 65.0°), a large mandibular plane angle (SN-MP, 53.0°), and a short ramus height (29.0 mm) (
Figure 1 and
Table 1).
Treatment
A three-stage approach was inevitably performed to resolve recurrent TMJ ankylosis and other skeletodental problems.
Stage I treatment during early childhood
Objectives and treatment plan
The objectives were as follows: (1) to remove the ankylosed part of TMJ and rehabilitate jaw function, and (2) to allow the chance of normal mandibular growth.
High condylectomy and interpositional arthroplasty were recommended to lower the risk of mandibular growth inhibition. And the patient's parents were informed of the possibility of re-ankylosis.
Treatment progress
Computed tomographic (CT) images and panoramic radiograph obtained before stage I treatment are presented in
Figure 2. At 6 years and 3 months of age, the upper 3 to 5 mm of the condyle was removed, and the cut surface was given a round shape (
Figure 2 and
Table 2). Interpositional arthroplasty was performed by reshaping of the articular eminence and placement of the temporal musculofascial flap in the glenoid fossa (
Figure 2 and
Table 2).
Treatment outcome
The maximum mouth opening increased from 7 to 22 mm.
Follow-up results
The mandible exhibited a downward and forward growth at one year after the stage I surgery (
Figure 2). However, when the patient was 11 years and 10 months old, the maximum mouth opening decreased from 22 to 14 mm. In addition, she developed symptoms of obstructive sleep apnea (OSA; apnea-hypopnea index, 96.7; lowest oxygen saturation, 64%).
CT images exhibited mandibular retrusion, chin point deviation to the right side, recurrence of TMJ ankylosis, deepening of the antegonial notch, and elongation of the coronoid process (
Figure 3).
Stage II treatment during early adolescence
Objectives and treatment plan
The objectives were as follows: (1) to remove the reankylosed portion of TMJ and increase the mouth opening, (2) to correct the mandibular retrusion and chin point deviation, (3) to establish normal occlusion, and (4) to restore the airway space.
Gap arthroplasty for the right TMJ and coronoidectomy of both sides were planned to remove the reankylosed portion and to increase the mouth opening, respectively. Bilateral MDO (BMDO) was planned to lengthen the mandibular body length and ramus height, correct the chin point deviation using differential distraction between the right and left sides, and increase the retroglossal airway volume.
1415
Treatment progress
Gap arthroplasty and coronoidectomy were performed at the age of 11 years and 11 months according to the treatment plan (
Figure 3 and
Table 2). Six months later, when the patient was 12 years and 5 months old (hand-wrist radiograph: R-IJ growth stage,
Figure 4),
16 two extraoral unidirectional distractors (KLS Martin Corporation, Tuttlingen, Germany) were placed with a downward vector in the posterior mandibular body (
Figure 5 and
Table 2). The maxillary first premolars were extracted and a total of four miniplates were installed at the infrazygomatic crest area and the symphysis area on both sides (
Figure 5). After a latency period of 5 days, active distraction at the rate of 1.0 mm/day was performed for 30 days on the right side and 19 days on the left side (
Figure 5 and
Table 2). During the distraction period, orthodontic treatment of the maxillary arch was started. When overcorrection of the mandibular dental midline was achieved, a two-month consolidation period was given. During the distraction and consolidation periods, Class III elastics (5/16 inch, 6 ounce) between the miniplates installed in the maxilla and mandible were used to mold the distracted bony segment and to minimize clockwise rotation of the mandible. At the time of removal of the distraction osteogenesis device, the mandibular first premolars were extracted and the orthodontic brackets were bonded on the mandibular arch. Post-BMDO orthodontic treatment was completed at the age of 14 years and 8 months (
Figure 6 and
Table 2).
Treatment outcomes
The treatment resulted in significant correction of the chin point deviation, an improvement in the facial profile, Class I canine and molar relationships, a normal overjet/overbite, and overcorrection of the mandibular dental midline (
Figure 6 and
Table 1). The maximum mouth opening increased from 14 to 33 mm.
Lateral cephalograms demonstrated mandibular advancement of 7 mm at the pogonion and increase in the retroglossal airway volume (
Figure 6 and
Table 1).
Follow-up results
One year after post-BMDO debonding, slight bite opening was observed due to clockwise rotation of the mandible (
Figure 7).
Five years after post-BMDO debonding, the maximum mouth opening decreased from 33 to 8 mm. CT images revealed re-ankylosis of both TMJs, particularly on the right side (
Figure 8). Because the upper airway space was decreased (
Figure 8), the patient had to use a continuous positive airway pressure device. In addition, the mandibular anterior teeth exhibited gingival recession caused by retraction forces from the labial frenum and muscles.
Stage III treatment after completion of growth
Despite a series of previous surgical interventions during stages I and II, re-ankylosis of the TMJs, skeletodental problems, and OSA symptoms were recurred at the age of 19 years and 4 months.
Objectives and treatment plans
The objectives were as follows: (1) to remove the reankylosed portion and increase the mouth opening; (2) to prevent the reankylosis; (3) to correct the mandibular retrusion and chin point deviation, (4) to establish normal occlusion, and (5) to restore the patency of the upper airway.
The three treatment options were suggested to the patient and her parents: (1) two-jaw surgery with counter- clockwise rotation for advancement of the maxillomandibular complex; (2) the same two-jaw surgery recommended in option 1 along with reconstruction of the bilateral TMJs using artificial prostheses; and (3) one-jaw surgery with counterclockwise rotational advancement of the mandible and reconstruction of the bilateral TMJs using artificial prostheses.
The patient and her parents chose option 3 because the procedure could resect the ankylotic bone and terminate the biologic ankylosis progression.
171819 Furthermore, they wanted to undergo a less invasive procedure.
Treatment progress
As a preparatory surgery, low condylectomy on the right side and coronoidectomy on both sides were performed. As a result, the patient developed a severe Class II openbite with chin deviation to the right side (
Figure 8 and
Table 1).
During 8 months of pre-TMJ-reconstruction orthodontic treatment, the mandible slightly rotated counter-clockwise through physiologic repositioning (
Figure 9). Reconstruction of the bilateral TMJs was performed using artificial prostheses (Biomet Microfixation TMJ replacement system, Warsaw, IN, USA): (1) Following Risdon and pre-auricular incision, the masseter and medial pterygoid muscles were reflected and the lateral surface of the ramus was contoured; (2) Once the fossa component of the artificial prosthesis was installed, the mandible was advanced with counterclockwise rotation using a surgical wafer; (3) Intermaxillary fixation was performed; (4) The mandibular component of the artificial prosthesis was fixed in the correct position; and (5) genioglossus advancement procedure was performed to pull the genioglossus/geniohyoid muscles forward for alleviation of the OSA symptoms. One month after surgery, post-TMJ-reconstruction orthodontic treatment was initiated and continued for three-and-half months (
Table 2).
Treatment outcomes
The patient's facial profile exhibited a significant improvement and Class I canine and molar relationships were obtained along with a normal overjet/overbite (
Figure 10 and
Table 1). Fortunately, gingival recession in the mandibular anterior teeth area was not aggravated (
Figure 10), and the patient refused to undergo gingival grafting. The maximum mouth opening increased from 14 to 38 mm.
Lateral cephalogram exhibited mandibular advancement by 18 mm at the pogonion and an increase in the ramus height by 5 mm (
Figures 10,
Table 1). Although the patient refused to undergo post-treatment polysomnography, her OSA symptoms relieved and the airway volume increased from 9.4 to 15.8 mL on the CT images (
Figure 11).
Follow-up results
Class I canine and molar relationships and normal overbite/overjet were well maintained at the one-year follow-up visit (
Figure 12).
This case report was reviewed and approved by the institutional review board at Seoul National University Dental Hospital (ERI18012). The patient gave us a written informed consent for publication of her data.
DISCUSSION
In the present report, the longitudinal management of recurrent TMJ ankylosis from infancy to adulthood via orthodontic and surgical approach was described (
Figure 13,
Table 2).
Functional and esthetic rehabilitation of patients with TMJ ankylosis is challenging because of technical difficulties and a high incidence of recurrence. Surgical skills and post-operative management including early mouth opening exercise, appropriate physiotherapy, and close follow-ups are important factors for achieving successful outcomes.
47
Henry and Wolford
11 evaluated patients who underwent multiple TMJ surgeries and reported a higher success rate with custom-made total joint prostheses than with various autogenous grafts (88% vs. 13–31%). Wolford et al.
20 demonstrated adequate function of artificial TMJ prostheses during a follow-up period of 5 to 8 years. However, such prostheses are also associated with problems such as wear, mobility or fracture of the implant, hypersensitivity, a foreign body reaction, and heterotropic bone formation.
1221
On the basis of the findings from this case, we would like to suggest a treatment flow-chart for the management of TMJ ankylosis according to the growth stage (
Figure 14). Primarily, the flowchart shows that the treatment-involved area increases with the duration of ankylosis, patient's age, and degree of deformity.
First, when TMJ ankylosis is detected in early childhood, high condylectomy and interpositional arthroplasty are recommended to remove the ankylosed portion, to achieve functional rehabilitation, and to provide the opportunity for normal growth of the mandible.
Second, when TMJ ankylosis is detected or recurs in early adolescence, high or low condylectomy, interpositional or gap arthroplasty, coronoidectomy, or MDO and pre- and post-MDO orthodontic treatment are recommended to correct mandibular retrusion and/or facial asymmetry, to achieve Class I occlusion, and/or to relieve the OSA symptoms. Since the mandible is still growing at this stage, there is a possibility of aggravation of facial asymmetry and/or mandibular retrusion. Therefore, when progressive TMJ ankylotic change in adolescent patients cannot be arrested despite a series of surgical interventions, further surgical approaches including TMJ reconstruction using artificial prostheses should be delayed until completion of growth.
Finally, in adult patients, two-jaw or one-jaw surgery, TMJ reconstruction using artificial prostheses along with counterclockwise rotation of the maxillomandibular complex, genioglossus advancement procedure, and pre- and post-TMJ-reconstruction orthodontic treatment can be performed to exterminate the ankylosis, to correct mandibular retrusion and/or facial asymmetry, to achieve Class I occlusion, and/or to relieve the OSA symptoms.
The findings from this case suggest that it is necessary to consider the diverse factors of individual patients and meticulously observe the treatment outcomes and prognosis.
CONCLUSION
Since the treatment modalities for TMJ ankylosis differ according to the duration of ankylosis, patient age, and degree of deformity, the treatment flowchart suggested in this report could be used as an effective guideline for determining the appropriate timing and methods for the treatment of TMJ ankylosis.
Figures and Tables
Figure 1
Initial visit. Facial and intraoral photographs (A, B, C), posteroanterior and lateral cephalograms (D, E), and a panoramic radiograph (F) obtained at age of 2 years and 4 months.

Figure 2
Stage I treatment. Computed tomographic images obtained before high condylectomy and interpositional arthroplasty (A; age, 6 years and 1 month), a panoramic radiograph obtained just after high condylectomy and interpositional arthroplasty (B; age, 6 years and 3 months), and a lateral cephalogram obtained at one year after high condylectomy and interpositional arthroplasty (C; age, 7 years and 2 months).

Figure 3
Stage II treatment. Computed tomographic images obtained before (A; age, 11 years and 10 months) and after gap arthroplasty of the right temporomandibular joint and bilateral coronoidectomy (B; age, 11 years and 11 months).
Figure 4
Stage II treatment. Facial and intraoral photographs and a hand-wrist radiograph obtained just before bilateral mandibular distraction osteogenesis (age, 12 years and 5 months). The dotted line in the intraoral photograph indicates the mandibular dental midline.

Figure 5
Stage II treatment. Facial and intraoral photographs, posteroanterior and lateral cephalograms, and a panoramic radiographs obtained at the end of the distraction period (30 mm of distraction on the right side and 19 mm on the left side) and in the middle of post-bilateral mandibular distraction osteogenesis orthodontic treatment (age, 12 years and 6 months).

Figure 6
Stage II treatment. Facial and intraoral photographs, posteroanterior and lateral cephalograms, and a panoramic radiographs obtained at the first debonding (age, 14 years and 8 months).

Figure 7
Facial and intraoral photographs, posteroanterior and lateral cephalograms, and a panoramic radiograph obtained one year after stage II treatment (age, 15 years and 8 months).

Figure 8
Stage III treatment. Computed tomographic images obtained at 4 years and 8 months after stage II treatment (A), facial and intraoral photos (B), and posteroanterior and lateral cephalograms and a panoramic radiograph (C) obtained after low condylectomy on the right side and coronoidectomy on the left side (age, 19 years and 4 months).

Figure 9
Stage III treatment. Intraoral photographs (A, upper low: 6 months after preoperative orthodontic treatment, lower low: 3 weeks after temporomandibular joint (TMJ) reconstruction surgery), posteroanterior and lateral cephalograms, and panoramic radiographs (B) obtained before and after TMJ reconstructive surgery of both sides and three dimensional facial computed tomographic images (C) obtained after reconstruction of TMJs using artificial prostheses.

Figure 10
Stage III treatment. Facial and intraoral photographs, posteroanterior and lateral cephalograms, and a panoramic radiograph obtained at the second debonding (age, 20 years and 5 months).

Figure 11
Stage III treatment. Changes in the total volume and minimum area of the upper airway before (A; age, 19 years and 4 months) and after reconstruction of temporomandibular joints using artificial prosthesis (B; age, 20 years and 5 months).

Figure 12
Facial and intraoral photographs, posteroanterior and lateral cephalograms, and a panoramic radiograph obtained one year after debonding (age, 21 years and 5 months).

Figure 13
Superimpositions of lateral and posteroanterior cephalograms within each treatment stage.
BMDO, Bilateral mandibular distraction osteogenesis; TMJ, temporomandibular joint; pre-op. Orthod. Tx., pre-operative orthodontic treatment.

Figure 14
Treatment flowchart for the management of TMJ ankylosis according to the growth stage.
TMJ, Temporomandibular joint; MDO, mandibular distraction osteogenesis; Orthod. Tx, orthodontic treatment; Max. Occl., maxillary occlusal.

Table 1
Cephalometric analyses during three stages of treatment for recurrent temporomandibular joint ankylosis from infancy to adulthood
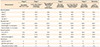
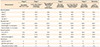
Table 2
Treatment progress for recurrent TMJ ankylosis from infancy to adulthood

ACKNOWLEDGEMENTS
The authors appreciate the patient in this case report. This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI18C1638).
References
1. Kazanjian VH. Temporomandibular joint ankylosis with mandibular retrusion. Am J Surg. 1955; 90:905–910.

2. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990; 48:1145–1151. discussion 1152.

3. Ko EW, Huang CS, Chen YR. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg. 1999; 57:789–798. discussion 799–800.

4. Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009; 67:1966–1978.

5. Vasconcelos BC, Bessa-Nogueira RV, Cypriano RV. Treatment of temporomandibular joint ankylosis by gap arthroplasty. Med Oral Patol Oral Cir Bucal. 2006; 11:E66–E69.
6. Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966; 24:405–409.
7. Cheung LK, Lo J. The long-term effect of transport distraction in the management of temporomandibular joint ankylosis. Plast Reconstr Surg. 2007; 119:1003–1009.

8. Stucki-McCormick SU. Reconstruction of the mandibular condyle using transport distraction osteogenesis. J Craniofac Surg. 1997; 8:48–52. discussion 53.

9. López EN, Dogliotti PL. Treatment of temporomandibular joint ankylosis in children: is it necessary to perform mandibular distraction simultaneously? J Craniofac Surg. 2004; 15:879–884. discussion 884–5.

10. Peltomäki T. Growth of a costochondral graft in the rat temporomandibular joint. J Oral Maxillofac Surg. 1992; 50:851–857. discussion 857–8.

11. Henry CH, Wolford LM. Reconstruction of the temporomandibular joint using a temporalis graft with or without simultaneous orthognathic surgery. J Oral Maxillofac Surg. 1995; 53:1250–1256. discussion 1256–7.

12. van Loon JP, de Bont GM, Boering G. Evaluation of temporomandibular joint prostheses: review of the literature from 1946 to 1994 and implications for future prosthesis designs. J Oral Maxillofac Surg. 1995; 53:984–996. discussion 996–7.
13. Wolford LM, Karras S, Mehra P. Concomitant temporomandibular joint and orthognathic surgery: a preliminary report. J Oral Maxillofac Surg. 2002; 60:356–362. discussion 362–3.

14. Coleta KE, Wolford LM, Gonçalves JR, Pinto Ados S, Cassano DS, Gonçalves DA. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part II--airway changes and stability. Int J Oral Maxillofac Surg. 2009; 38:228–235.

15. Yadav R, Bhutia O, Shukla G, Roychoudhury A. Distraction osteogenesis for management of obstructive sleep apnoea in temporomandibular joint ankylosis patients before the release of joint. J Craniomaxillofac Surg. 2014; 42:588–594.

16. Hägg U, Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982; 82:299–309.

17. Dela Coleta KE, Wolford LM, Gonçalves JR, Pinto Ados S, Pinto LP, Cassano DS. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part I--skeletal and dental stability. Int J Oral Maxillofac Surg. 2009; 38:126–138.

18. Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994; 52:2–10. discussion 11.

19. Wojczyńska A, Leiggener CS, Bredell M, Ettlin DA, Erni S, Gallo LM, et al. Alloplastic total temporomandibular joint replacements: do they perform like natural joints? Prospective cohort study with a historical control. Int J Oral Maxillofac Surg. 2016; 45:1213–1221.

20. Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg. 2015; 73:952–960.

21. Mercuri LG, Giobbie-Hurder A. Long-term outcomes after total alloplastic temporomandibular joint reconstruction following exposure to failed materials. J Oral Maxillofac Surg. 2004; 62:1088–1096.


















 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download