Abstract
Objective
Methods
Results
Figures and Tables
Figure 1
Miniscrew-assisted rapid palatal expansion appliance. A, Before expansion. B, After expansion.

Figure 2
Midpalatal suture opening width in periapical radiographic images (A) at T0 and (B) at T1 in separation and at T2 in non-separation cases. The midpalatal suture opening width was defined as the difference in distance (a′–a) between the mesial cementoenamel junctions of both upper central incisors.

Figure 3
Re-orientation in InVivo5® software. A, In the coronal view, the horizontal line connected with both infraorbital lower borders. B, In the sagittal view, the Frankfort horizontal plane was used.
Figure 4
Measurements of palate length and the maxillary first premolar (U4) palate depth. A, Baselines for palate length in a sagittal view: the horizontal line passing through incisive foramen and the vertical line passing through posterior nasal spine (PNS). B, The solid arrow indicates palate length, defined as a perpendicular length from the posterior border of incisive foramen to the horizontal line made by coronal plane through the PNS sagittally. C, In an axial view, the horizontal line passing through both U4 buccal tips. D, In a coronal slice including the horizontal line in C, a solid arrow indicates U4 palate depth, defined as the perpendicular length from the deepest point on the palate to the horizontal line connecting both palatal cementoenamel junction points of U4.

Figure 5
Schematic images of midpalatal suture maturation stages by midpalatal suture morphology, in accordance with the results reported by Angelieri et al.20 Stage A shows a straight high-density line of a midpalatal suture with little interdigitation; stage B shows a scalloped high-density line of a suture; stage C shows two parallel, scalloped, high-density lines both in the maxillary and palatine bones; stage D is characterized by the fusion of the midpalatal suture in the palatine bone; and in stage E, the midpalatal suture is not seen even in the maxillary portion.

Figure 6
Evaluations of grey scales for midpalatal suture density ratio. A, In the midpalatal suture. B, In the palatine process of the maxilla and soft palate, in accordance with the results reported by Grünheid et al.21
Figure 7
Correlations between midpalatal suture opening ratio and age (A), palate length (B), MPSM stage (C), MPSD ratio (D), SN-MP angle (E), and ANB angle (F). Best-fit lines with correlation coefficients, r by Pearson correlation analysis and rs by Spearman correlation analysis (A–C, p < 0.01; D–F, p > 0.05).

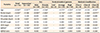
Table 2
Basic characteristics of the subjects (n = 31)

Values are presented as mean ± standard deviation (range) or number only.
MARPE, Miniscrew-assisted rapid palatal expansion; SN-MP, sella-nasion-mandibular plane; ANB, point A-nasion-point B; T0, initial; T1, when the midpalatal suture opening was confirmed in a periapical radiograph; T2, right after MARPE expansion stopped.
Table 3
Comparison of mean values among the entire patient group and the separation and non-separation groups
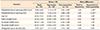
Table 4
Descriptive statistics of subgroups and comparison of the midpalatal suture opening ratio
Min, Minimum; max, maximum; IQR, interquartile range; MPSM, midpalatal suture maturation; SN-MP, sella-nasion-mandibular plane; ANB, point A-nasion-point B.
Mann–Whitney U test or Kruskal–Wallis test was performed because the data were not normally distributed.
*p < 0.05; **p < 0.01.
Refer to Figure 5 for definitions of MPSM stage.
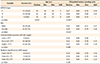
Table 5
Correlations between midpalatal suture opening ratio and variables in the entire patient group and subgroups
Vertical skeletal pattern by SN-MP angle: low, SN-MP < 27°; average, 27° ≤ SN-MP ≤ 37°; high, SN-MP > 37°.
Skeletal classification by ANB angle: Class I, 0° ≤ ANB ≤ 4°; Class II, ANB > 4°; Class III, ANB < 0°.
U4 and U6, The maxillary first premolar and molar respectively; SN-MP, sella-nasion-mandibular plane; ANB, point A-nasion-point B; MPSM, midpalatal suture maturation; MPSD, midpalatal suture density.
*p < 0.05; **p < 0.01.
†Pearson's correlation analysis was performed depending on the data normality, except for MPSM. For other subgroups, Spearman's rho, rs, was obtained by Spearman correlation analysis because the data were not normally distributed.
‡No statistical analysis was performed due to the small sample size.
§For MPSM, an ordinal scale, Spearman correlation analysis was performed.
Table 6
The determinant coefficient, R2 , values of midpalatal suture opening ratio corresponding to the number of independent variables
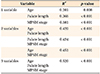
Table 7
Characteristics of the subjects in the non-separation group (n = 6)
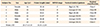
Vertical skeletal pattern by the SN-MP angle: low, SN-MP < 27°; average, 27° ≤ SN-MP ≤ 37°; high, SN-MP > 37°.
Skeletal classification by ANB angle: Class I, 0° ≤ ANB ≤ 4°; Class II, ANB > 4°; Class III, ANB < 0°.
MPSM, Midpalatal suture maturation; SD, standard deviation; SN-MP, sella-nasion-mandibular plane; ANB, point A-nasion-point B.
Refer to Figure 5 for definitions of MPSM stage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download