This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Various pre- and perioperative risk factors have been reported in association with blood loss in knee arthroplasty. However, the effect of the uncovered cancellous surface on blood loss in simultaneous bilateral total knee arthroplasty (SBTKA) by different prosthetic designs is not well elucidated. Therefore, this study aimed to compare the blood loss and transfusion rate between different knee prostheses in SBTKA and to identify risk factors that influence blood loss and transfusion after SBTKA.
Methods
Demographic and perioperative data of patients who underwent SBTKA using either a closed-box or an open-box femoral component of posterior-stabilized fixed-bearing (PS FB) knee system were retrospectively reviewed. The calculated blood loss (CBL) and blood transfusion rate were compared by using Student t-test and confirmed with multivariate regression analysis.
Results
There was no significant difference in preoperative parameters between 54 closed-box and 56 open-box PS FB TKAs. The CBL of the closed-box TKA group was 135.23 mL less (95% confidence interval [CI], −215.30 to −55.16; p = 0.001) than that of the open-box TKA group. However, the blood transfusion rates of the closed- and open-box TKA groups were not significantly different (24.1% and 38.5%, p = 0.11). For each additional minute of total operative time, 3.75 mL (95% CI, 1.75 to 5.76; p < 0.001) of blood loss was anticipated. For each additional mg/dL of preoperative hemoglobin, 71% (p < 0.001) reduction of blood transfusion probability was predicted.
Conclusions
The use of closed- and open-box knee prostheses resulted in a significant difference in blood loss in SBTKA. Prolonged operative time also significantly increased CBL. Therefore, strategies to control the bleeding surface and shorten operative duration may be considered if blood loss is of special concern. The preoperative hemoglobin was the only factor that affects the probability of blood transfusion in SBTKA.
Go to :

Keywords: Knee, Arthroplasty, Prosthesis, Bilateral, Blood loss, Transfusion
Total knee arthroplasty (TKA) is a successful surgical procedure for restoring knee joint function and relieving pain in end-stage knee arthropathy. Approximately 20% of patients have severe pain on both knees and 10% of patients undergo contralateral TKA within 1 year after the first procedure.
1) Therefore, simultaneous bilateral TKA (SBTKA) could provide advantages including the single operation, shortened total recovery time, and reduced perioperative cost. However, significantly higher perioperative morbidity has been demonstrated after SBTKA than after unilateral TKA (UTKA).
23) One of the major concerns in SBTKA is that the procedure can lead to a more substantial blood loss because of large exposure, deep soft-tissue dissection, and sinus bleeding from cancellous and uncovered surfaces after bone resection,
4567) resulting in a transfusion rate of 44.7% to 55%.
89) Although blood transfusion is the standard management of blood loss, it can increase the risk of complications such as cardiovascular volume overload, blood-transmitted disease, allergic reaction, and periprosthetic joint infection.
1011) Various pre- and perioperative risk factors including age, sex, race, body mass index (BMI), preoperative hemoglobin (Hb) level, comorbidity, and duration of operation have been reported in association with blood loss and postoperative blood transfusion in UTKA,
81213) and these factors might be assumed to be implicated in the bilateral procedure. However, there are few studies that investigated the significance of these potential determinants in SBTKA.
Additionally, evidence is sparse on the effect of different knee prosthetic designs on perioperative blood loss. The posterior-stabilized (PS) and cruciate-retaining (CR) designs of a similar knee prosthesis model were reported to result in different blood loss following UTKA.
714) The housing area of the distal femoral bone cut in PS TKA was supposed to be the source of bleeding and increasing perioperative blood loss. However, there was no difference in blood transfusion between the knee prosthetic designs.
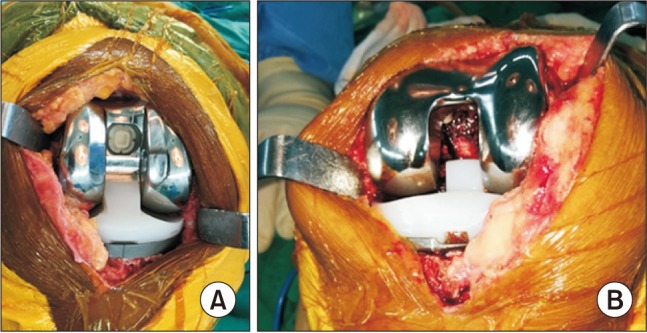
714) As stated above, SBTKA will cause more substantial blood loss; thus, the different knee prostheses may have more influence on blood loss and the requirement for blood transfusion in the bilateral procedure. At our institution, we have implanted two different designs of PS fixed-bearing (PS FB) femoral prostheses in TKA: closed-box design and open-box design that covers and uncovers cancellous bone of the distal femoral housing, respectively. However, the benefit of the closed-box femoral component in SBTKA is still unclear. Hence, this study aimed to compare the drain output (DO), calculated blood loss (CBL), and allogeneic blood transfusion rate between SBTKAs that implanted different knee designs; and to identify the risk factors that may be associated with CBL and blood transfusion. We hypothesized that implantation of the less exposed trimmed-cancellous surface (closed box) may reduce blood loss when compared to the more exposed cancellous bone (open box), particularly in SBTKA (
Fig. 1).
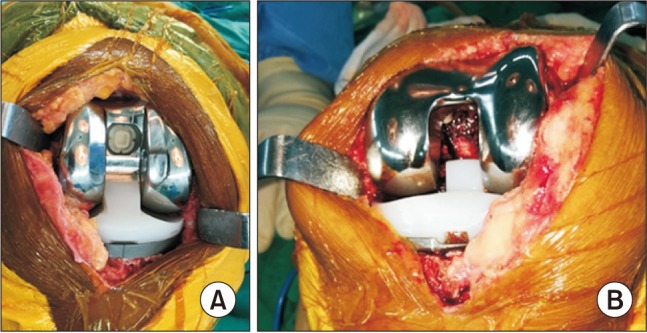 | Fig. 1(A) The closed-box prosthesis fully covers cancellous bone of the distal femoral housing. (B) Bleeding from the area of trimmed cancellous surface may be responsible for the significantly higher calculated blood loss in the open-box prosthesis group than that in the closed-box prosthesis group.
|
METHODS
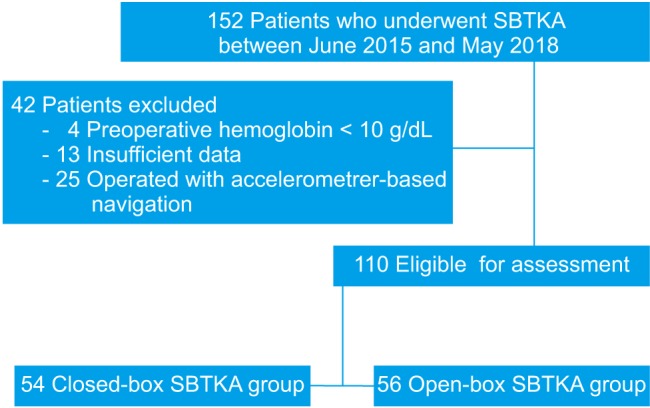
We retrospectively analyzed the prospectively collected data of 152 patients who underwent SBTKA using either the closed-box or open-box femoral prosthesis design from June 2015 to May 2018. Four patients with preoperative Hb less than 10 g/dL, 13 patients with incomplete data, and 25 patients operated with accelerometer-based navigation were excluded. A total of 110 SBTKA patients (54 closed-box and 56 open-box TKAs) remained for assessment (
Fig. 2). The study was approved by the Institutional Review Board of Naresuan University with the study registry of TCTR20180220001.
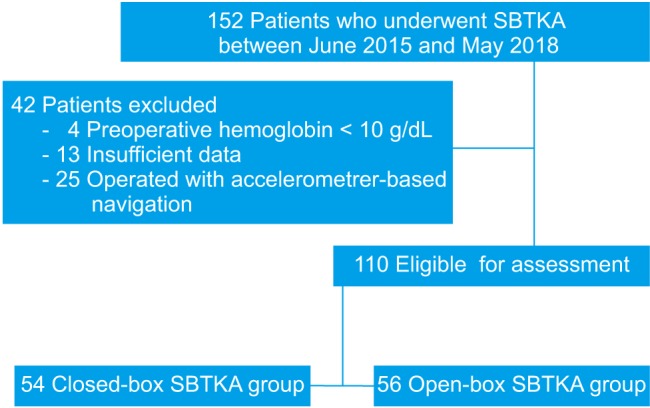 | Fig. 2Study flowchart. SBTKA: simultaneous bilateral total knee arthroplasty.
|
All surgical procedures were performed by a single surgeon (AL) with an identical surgical technique through a standard medial parapatellar approach. All the patients underwent regional anesthesia and received a periarticular injection with a multidrug mixture (0.5% Marcaine, 20 mL [AstraZeneca, Lund, Sweden], 30 mg Ketorolac [Siu Guan, Chiayi, Taiwan], 5 mg morphine sulfate, and 300 µg adrenaline [1:1000, 0.3 mL]). The procedure was done under tourniquet control of 250 mmHg by inflating before the incision. Following an arthrotomy, a distal femoral cut was performed with an intramedullary guide system while a proximal tibial cut was done with an extramedullary guide system. After completion of the bone cut, the opening of the femoral medullary canal was closed with a bone plug. All the knees were implanted with a cemented PS FB TKA system. There were two types of knee prosthesis used during the study period: closed-box TKA (PFC Sigma; DePuy Synthes, Warsaw, IN, USA) and open-box TKA (NexGen LPS; Zimmer Biomet, Warsaw, IN, USA). The patella was resurfaced in all cases of the closed-box group but in none of the cases in the open-box group. A vacuum drain was applied, and then 15 mg/kg of topical tranexamic acid (TXA) was poured into the knee joint before closure of the arthrotomy. A compressive dressing was applied and the tourniquet was deflated. The drains were closed for 3 hours in all knees.
An identical postoperative protocol was conducted for every patient. During the first 48 hours, intravenous (IV) patient-controlled analgesia morphine (on-demand bolus of 0.5 mg of morphine sulfate with a 5-minute lockout period) and 30 mg of ketorolac every 8 hours were administered for pain control. After 48 hours, all the catheters and drains were discarded, and then 250 mg of naproxen was given every 12 hours orally combined with additional 2 mg of IV morphine as rescue analgesia for breakthrough pain. The serum Hb level was monitored at 24, 48, and 72 hours after the index surgery. The patients began postoperative physiotherapy on the day after surgery. Postoperative thromboembolic prophylaxis consisted of low-molecular-weight heparin injected subcutaneously daily for 2 days and oral warfarin for 10 days.
The outcome parameters including demographic data, total operative time (TOT), DO, postoperative Hb, blood transfusion rate, and length of stay (LOS) were routinely recorded by the independent physicians (PV, KR) at our institution. The total blood volume (TBV) and CBL were calculated by using the equation of Nadler et al.
15) and the Hb balance method,
16) respectively:
The difference between the preoperative and lowest Hb was applied to the Hb balance method. The blood transfusion threshold for our SBTKA procedure is postoperative Hb level below 9.0 g/dL.
Statistical Analysis
Descriptive statistics were used as appropriate. The unpaired Student t-test was used to compare the difference of measured outcomes (DO, CBL, TOT, and LOS) between the two groups. Blood transfusion rate was compared between the two groups by using chi-square test. Multivariate regression analysis, controlling for age, BMI, American Society of Anesthesiologist (ASA) physical status classification, preoperative Hb, TOT, and type of knee prosthesis, was used for analysis of factors associated with the CBL and blood transfusion rate. Statistical significance was defined as p < 0.05. Stata/MP ver. 15.0 (Stata Corp., College Station, TX, USA) was used for all analyses. A post hoc analysis revealed that the sample size of this study had 88.2% power to detect a difference in the mean CBL of 120 mL with a standard deviation of 250 mL and an alpha of 0.05.
Go to :

RESULTS
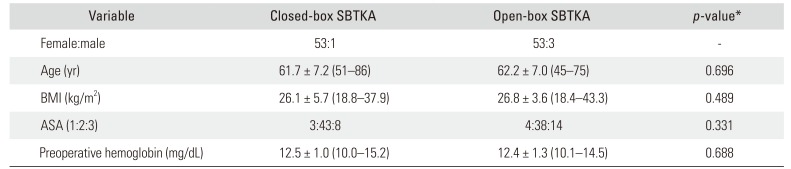
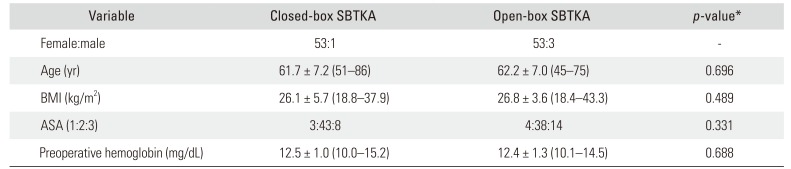
There was no significant difference between two groups (54 closed-box and 56 open-box TKAs) in terms of demographics and preoperative Hb level (
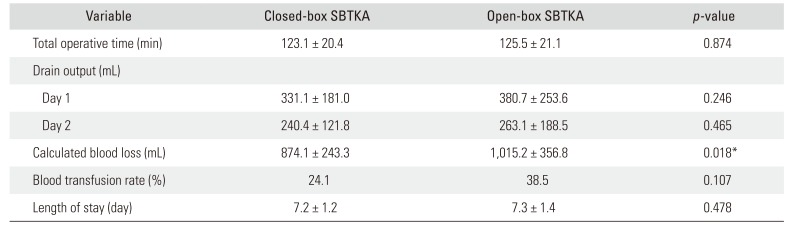
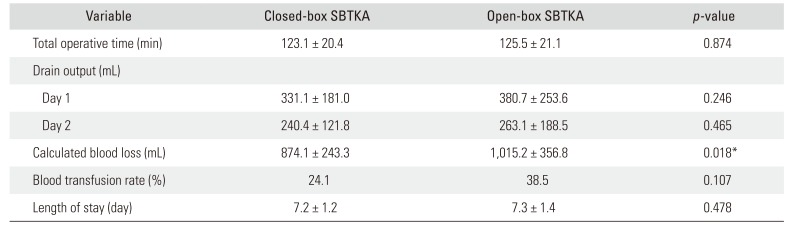
Table 1). The TOT and LOS were not different between closed-box and open-box TKAs (
Table 2). The DOs on day 1 and 2 in open-box SBTKA were greater than those in closed-box SBTKA, but there was no statistical significance. The CBL in closed-box SBTKA was significantly lower than that in open-box SBTKA (874.1 ± 243.3 vs. 1,015.2 ± 356.8 mL;
p = 0.02) as presented in
Table 2.
Table 1
Demographic Characteristics
|
Variable |
Closed-box SBTKA |
Open-box SBTKA |
p-value*
|
|
Female:male |
53:1 |
53:3 |
- |
|
Age (yr) |
61.7 ± 7.2 (51–86) |
62.2 ± 7.0 (45–75) |
0.696 |
|
BMI (kg/m2) |
26.1 ± 5.7 (18.8–37.9) |
26.8 ± 3.6 (18.4–43.3) |
0.489 |
|
ASA (1:2:3) |
3:43:8 |
4:38:14 |
0.331 |
|
Preoperative hemoglobin (mg/dL) |
12.5 ± 1.0 (10.0–15.2) |
12.4 ± 1.3 (10.1–14.5) |
0.688 |

Table 2
Comparison of Perioperative Characteristics between the Closed-Box and Open-Box SBTKA
|
Variable |
Closed-box SBTKA |
Open-box SBTKA |
p-value |
|
Total operative time (min) |
123.1 ± 20.4 |
125.5 ± 21.1 |
0.874 |
|
Drain output (mL) |
|
|
|
|
Day 1 |
331.1 ± 181.0 |
380.7 ± 253.6 |
0.246 |
|
Day 2 |
240.4 ± 121.8 |
263.1 ± 188.5 |
0.465 |
|
Calculated blood loss (mL) |
874.1 ± 243.3 |
1,015.2 ± 356.8 |
0.018*
|
|
Blood transfusion rate (%) |
24.1 |
38.5 |
0.107 |
|
Length of stay (day) |
7.2 ± 1.2 |
7.3 ± 1.4 |
0.478 |

In multiple linear regression analysis, controlling for age, BMI, ASA, preoperative Hb, TOT, and type of knee prosthesis, the CBL of the closed-box was 135.2 mL less than that of the open-box TKA (95% confidence interval [CI], −215.3 to −55.2; p = 0.001). For each additional minute of TOT, 3.8 mL (95% CI, 1.8 to 5.8; p < 0.01) of blood loss was anticipated while age, BMI, and ASA had no significant effect on the CBL.
The blood transfusion rates of closed-box and open-box TKA groups were 24.1% and 38.5%, respectively (p = 0.11). With multiple logistic regression analysis, adjusting for age, BMI, ASA, preoperative Hb, TOT, and type of knee prosthesis, 71% reduction of blood transfusion probability was predicted for each additional mg/dL of preoperative Hb (p < 0.001), while other factors had no significant effect.
Go to :

DISCUSSION
Blood loss is an inevitable morbidity after TKA and it is more substantial in patients with SBTKA.
17) Although ongoing bleeding from venous sinus of trimmed cancellous bone is responsible for blood loss after UTKA,
41418) studies that directly analyze the perioperative blood loss according to different prostheses are limited. Therefore, our study aims to differentiate the effect of different knee prostheses on blood loss in patients undergoing SBTKA.
In the current study, the closed-box SBTKA could significantly reduce CBL by 135.23 mL when compared to open-box SBTKA, even though patellar resurfacing was performed routinely in the closed-box group. Mahringer-Kunz et al.
7) assessed a series of 473 patients who underwent either PS or CR UTKA. They reported the CBL was significantly lower (by 46 mL) in CR UTKA. Cankaya et al.
14) also compared 50 CR UTKAs and 50 PS UTKAs and found that DO was 43 mL lower and CBL was 74 mL lower in CR UTKA. We agree with these previous studies: the area of the trimmed cancellous surface that was uncovered by prosthesis may be responsible for differences in CBL between different knee prosthetic designs,
56714) because the total DO was 72.36 mL less in closed-box TKA. However, the blood transfusion rate was not significantly different according to the selection of knee prosthesis, even in our SBTKA setting. Although an occlusion of the femoral opening hole with the bone plug was applied to reduce the blood loss, Torres-Claramunt et al.
19) reported a similar outcome regarding DO, postoperative Hb level, and transfusion rate when an open-box prosthesis was implanted with or without a femoral bone plug. In addition, Moo et al.
20) recently investigated the sealant effect of bone wax to reduce blood loss from exposing a trimmed cancellous surface in UTKA. They demonstrated less bleeding from the occluded nail hole and a significant decrease of total blood loss in the bone wax group than in the control group (987.9 vs. 1,183.5 mL). Other strategies including platelet-rich plasma and platelet gel applied to the bleeding surface before TKA wound closure could also reduce blood loss after the index surgery.
2122) Therefore, special techniques that control any bleeding surface may further minimize the perioperative blood loss regardless of femoral hole occlusion.
Some pre- and perioperative risk factors including age, sex, race, BMI, preoperative Hb level, comorbidity, and duration of operation have been reported to affect the CBL and postoperative blood transfusion of UTKA.
812132324) Preoperative Hb level is considered as a major predictor because lower preoperative Hb level may affect the gradient between baseline and physician transfusion trigger.
25) Patients aged more than 85 years have 3.5 times higher blood transfusion rate than do younger patients. Compromise of postoperative hematopoietic activity due to advanced age may be an explanation.
12) Prolonged operation time may be a result of difficult and extensive surgical dissection of the procedure and lead to more blood loss.
1325) A higher ASA score reflecting patient's comorbidity may confound clotting cascade.
812) Furthermore, male and Caucasian patients have a lower risk for blood transfusion after UTKA as shown in several studies.
81213) According to our study, each additional minute of TOT would result in 3.75 mL more CBL in SBTKA, but it had no effect on the blood transfusion requirement. The preoperative Hb level was the only factor affecting the blood transfusion rate with 71% less likely to get a blood transfusion for each additional mg/dL of preoperative Hb. Various blood-preserving techniques aimed at decreasing the complications from a blood transfusion have been described in contemporary orthopedic literature. Among these techniques, administration of TXA is one of the greatest avenues to decrease blood loss in SBTKA without increasing the risk of a thromboembolic event.
26272829) Chen et al.
26) revealed the effectiveness of IV TXA administration in SBTKA. Their results showed a significant decrease in blood loss (1,739.5 vs. 2,392.9 mL), DO (245.3 vs. 613.4 mL), transfusion rate (60% vs. 96.7%), and the average number of transfused blood units (1.9 vs. 4.1 units) with IV TXA when compared to SBTKA without TXA. Bagsby et al.,
27) Karaaslan et al.,
28) and Aggarwal et al.
29) all showed results that support the advantage of topical and IV administration of TXA in SBTKA patients. The effect of TXA may be one of the reasons why age, BMI, and ASA had an insignificant effect on CBL and blood transfusion rate in our study.
There are some limitations to the present study. First, our study group consisted of predominantly women. Therefore, we could not determine the effect of gender on CBL and blood transfusion rate in the analysis. Nevertheless, females have been associated with significantly less blood loss after UTKA when compared to males.
2324) Second, we prefer to routinely resurface the patella in closed-box SBTKA but not in open-box SBTKA. Despite this difference, closed-box SBTKA significantly reduced the CBL and DO when compared to open-box SBTKA. To the best of our knowledge, bleeding from resurfacing of the patella has not been well demonstrated and might not have confounded our result. Third, unlike other studies, our investigation found an insignificant impact of ASA, BMI, and age on CBL and postoperative blood transfusion. This may be due to the effect of TXA and narrow distribution of our study population. Fourth, our transfusion threshold according to the institutional protocol is higher than the conventional transfusion trigger. The difference in preoperative Hb and transfusion cut-off level may have caused different outcomes.
The use of closed- and open-box knee prostheses could result in a significant difference in blood loss in SBTKA. Prolonged operative time also significantly increased CBL. Therefore, strategies to control any bleeding surface and shorten operative duration may be considered if blood loss is of special concern. The preoperative Hb was the only factor that affects the probability of blood transfusion in SBTKA.
Go to :

ACKNOWLEDGEMENTS
We thank Atthakorn Jarusriwanna, MD (Faculty of Medicine, Naresuan University, Phitsanulok, Thailand), Nattharut Chaibhuddanugul, MD (Faculty of Medicine, Naresuan University, Phitsanulok, Thailand), Bhuwad Chinwatanawongwan, MD (Faculty of Medicine, Naresuan University, Phitsanulok, Thailand), Pariphat Chompoonutprapa, MD (Faculty of Medicine, Naresuan University, Phitsanulok, Thailand), Edward B. Rasor, Richard M. Glover (Faculty of Humanity, Naresuan University, Phitsanulok, Thailand), and Waykin Nopanitaya, PhD (Faculty of Medicine, Naresuan University, Phitsanulok, Thailand) for their technical assistance.
Go to :

Notes
Go to :

References
1. Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade: data from the Scottish Arthroplasty Project. Knee. 2006; 13(2):102–105. PMID:
16481171.

2. Kulshrestha V, Kumar S, Datta B, Sinha VK, Mittal G. Ninety-day morbidity and mortality in risk-screened and optimized patients undergoing two-team fast-track simultaneous bilateral TKA compared with unilateral TKA-A prospective study. J Arthroplasty. 2018; 33(3):752–760. PMID:
29102512.

3. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplasty. 2013; 28(7):1141–1147. PMID:
23518424.

4. Mylod AG Jr, France MP, Muser DE, Parsons JR. Perioperative blood loss associated with total knee arthroplasty: a comparison of procedures performed with and without cementing. J Bone Joint Surg Am. 1990; 72(7):1010–1012. PMID:
2384499.

5. Raut VV, Stone MH, Wroblewski BM. Reduction of postoperative blood loss after press-fit condylar knee arthroplasty with use of a femoral intramedullary plug. J Bone Joint Surg Am. 1993; 75(9):1356–1357. PMID:
8408156.

6. Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty: a prospective, randomized, multicenter study. J Bone Joint Surg Am. 1999; 81(11):1580–1588. PMID:
10565650.

7. Mahringer-Kunz A, Efe T, Fuchs-Winkelmann S, Schuttler KF, Paletta JR, Heyse TJ. Bleeding in TKA: posterior stabilized vs. cruciate retaining. Arch Orthop Trauma Surg. 2015; 135(6):867–870. PMID:
25917192.

8. Slover J, Lavery JA, Schwarzkopf R, Iorio R, Bosco J, Gold HT. Incidence and risk factors for blood transfusion in total joint arthroplasty: analysis of a statewide database. J Arthroplasty. 2017; 32(9):2684–2687. PMID:
28579446.

9. Jenny JY, Trojani C, Prudhon JL, et al. Simultaneous bilateral total knee arthroplasty: a multicenter feasibility study. Orthop Traumatol Surg Res. 2013; 99(2):191–195. PMID:
23465514.

10. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014; 96(4):272–278. PMID:
24553882.

11. Silliman CC, Fung YL, Ball JB, Khan SY. Transfusion-related acute lung injury (TRALI): current concepts and misconceptions. Blood Rev. 2009; 23(6):245–255. PMID:
19699017.

12. Yoshihara H, Yoneoka D. Predictors of allogeneic blood transfusion in total hip and knee arthroplasty in the United States, 2000-2009. J Arthroplasty. 2014; 29(9):1736–1740. PMID:
24891002.

13. Frisch NB, Wessell NM, Charters MA, Yu S, Jeffries JJ, Silverton CD. Predictors and complications of blood transfusion in total hip and knee arthroplasty. J Arthroplasty. 2014; 29(9 Suppl):189–192. PMID:
25007727.

14. Cankaya D, Ozkurt B, Aydin C, Tabak AY. No difference in blood loss between posterior-cruciate-ligament-retaining and posterior-cruciate-ligament-stabilized total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2014; 22(8):1865–1869. PMID:
24384945.

15. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962; 51(2):224–232. PMID:
21936146.
16. Chen JY, Chin PL, Moo IH, et al. Intravenous versus intraarticular tranexamic acid in total knee arthroplasty: a double-blinded randomised controlled noninferiority trial. Knee. 2016; 23(1):152–156. PMID:
26746044.

17. Qi Y, Tie K, Wang H, et al. Perioperative comparison of blood loss and complications between simultaneous bilateral and unilateral total knee arthroplasty for knee osteoarthritis. Knee. 2017; 24(6):1422–1427. PMID:
28974399.

18. Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005; 87(11):1480–1482. PMID:
16260662.
19. Torres-Claramunt R, Hinarejos P, Perez-Prieto D, et al. Sealing of the intramedullar femoral canal in a TKA does not reduce postoperative blood loss: a randomized prospective study. Knee. 2014; 21(4):853–857. PMID:
24842494.

20. Moo IH, Chen JY, Pagkaliwaga EH, Tan SW, Poon KB. Bone wax is effective in reducing blood loss after total knee arthroplasty. J Arthroplasty. 2017; 32(5):1483–1487. PMID:
28089184.

21. Aggarwal AK, Shashikanth VS, Marwaha N. Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop. 2014; 38(2):387–395. PMID:
24114251.

22. Gardner MJ, Demetrakopoulos D, Klepchick PR, Mooar PA. The efficacy of autologous platelet gel in pain control and blood loss in total knee arthroplasty: an analysis of the haemoglobin, narcotic requirement and range of motion. Int Orthop. 2007; 31(3):309–313. PMID:
16816947.
23. Cushner FD, Friedman RJ. Blood loss in total knee arthroplasty. Clin Orthop Relat Res. 1991; (269):98–101.

24. Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Int Orthop. 2007; 31(1):39–44. PMID:
16568327.

25. Noticewala MS, Nyce JD, Wang W, Geller JA, Macaulay W. Predicting need for allogeneic transfusion after total knee arthroplasty. J Arthroplasty. 2012; 27(6):961–967. PMID:
22608172.

26. Chen X, Cao X, Yang C, Guo K, Zhu Q, Zhu J. Effectiveness and safety of fixed-dose tranexamic acid in simultaneous bilateral total knee arthroplasty: a randomized double-blind controlled trial. J Arthroplasty. 2016; 31(11):2471–2475. PMID:
27167769.

27. Bagsby DT, Samujh CA, Vissing JL, Empson JA, Pomeroy DL, Malkani AL. Tranexamic acid decreases incidence of blood transfusion in simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2015; 30(12):2106–2109. PMID:
26235522.

28. Karaaslan F, Karaoglu S, Mermerkaya MU, Baktir A. Reducing blood loss in simultaneous bilateral total knee arthroplasty: combined intravenous-intra-articular tranexamic acid administration. A prospective randomized controlled trial. Knee. 2015; 22(2):131–135. PMID:
25659440.

29. Aggarwal AK, Singh N, Sudesh P. Topical vs intravenous tranexamic acid in reducing blood loss after bilateral total knee arthroplasty: a prospective study. J Arthroplasty. 2016; 31(7):1442–1448. PMID:
26947543.

Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download