1. Dee R. Total replacement arthroplasty of the elbow for rheumatoid arthritis. J Bone Joint Surg Br. 1972; 54(1):88–95. PMID:
5011749.

2. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986; 68(5):669–674. PMID:
3722222.

3. Giannicola G, Sacchetti FM, Antonietti G, Piccioli A, Postacchini R, Cinotti G. Radial head, radiocapitellar and total elbow arthroplasties: a review of recent literature. Injury. 2014; 45(2):428–436. PMID:
24112701.

4. Hackl M, Muller LP, Leschinger T, Wegmann K. Total elbow arthroplasty in traumatic and post-traumatic bone defects. Orthopade. 2017; 46(12):990–1000. PMID:
29098354.
5. Lami D, Chivot M, Caubere A, Galland A, Argenson JN. First-line management of distal humerus fracture by total elbow arthroplasty in geriatric traumatology: results in a 21-patient series at a minimum 2 years' follow-up. Orthop Traumatol Surg Res. 2017; 103(6):891–897. PMID:
28733108.

6. Mansat P, Bonnevialle N, Rongieres M, Bonnevialle P. Bone, Joint Trauma Study Group (GETRAUM). The role of total elbow arthroplasty in traumatology. Orthop Traumatol Surg Res. 2014; 100(6 Suppl):S293–S298. PMID:
25164351.

7. Pogliacomi F, Schiavi P, Defilippo M, et al. Total elbow arthroplasty following complex fractures of the distal humerus: results in patients over 65 years of age. Acta Biomed. 2016; 87(2):148–155. PMID:
27648996.
8. Pooley J, Salvador Carreno J. Total elbow joint replacement for fractures in the elderly: functional and radiological outcomes. Injury. 2015; 46 Suppl 5:S37–S42. PMID:
26362422.
9. Rajaee SS, Lin CA, Moon CN. Primary total elbow arthroplasty for distal humeral fractures in elderly patients: a nationwide analysis. J Shoulder Elbow Surg. 2016; 25(11):1854–1860. PMID:
27528540.

10. Schoch BS, Werthel JD, Sanchez-Sotelo J, Morrey BF, Morrey M. Total elbow arthroplasty for primary osteoarthritis. J Shoulder Elbow Surg. 2017; 26(8):1355–1359. PMID:
28734537.

11. Brinkman JM, de Vos MJ, Eygendaal D. Failure mechanisms in uncemented Kudo type 5 elbow prosthesis in patients with rheumatoid arthritis: 7 of 49 ulnar components revised because of loosening after 2-10 years. Acta Orthop. 2007; 78(2):263–270. PMID:
17464617.

12. Kim HJ, Kim JY, Kee YM, Rhee YG. Total elbow arthroplasty under unfavourable soft tissue conditions. Int Orthop. 2018; 42(2):367–374. PMID:
29209741.

13. Kim JM, Mudgal CS, Konopka JF, Jupiter JB. Complications of total elbow arthroplasty. J Am Acad Orthop Surg. 2011; 19(6):328–339. PMID:
21628644.

14. Klug A, Gramlich Y, Buckup J, Schweigkofler U, Hoffmann R, Schmidt-Horlohe K. Trends in total elbow arthroplasty: a nationwide analysis in Germany from 2005 to 2014. Int Orthop. 2018; 42(4):883–889. PMID:
29423639.

15. Park SE, Kim JY, Cho SW, Rhee SK, Kwon SY. Complications and revision rate compared by type of total elbow arthroplasty. J Shoulder Elbow Surg. 2013; 22(8):1121–1127. PMID:
23664747.

16. Toulemonde J, Ancelin D, Azoulay V, Bonnevialle N, Rongieres M, Mansat P. Complications and revisions after semi-constrained total elbow arthroplasty: a mono-centre analysis of one hundred cases. Int Orthop. 2016; 40(1):73–80. PMID:
26435264.

17. Welsink CL, Lambers KT, van Deurzen DF, Eygendaal D, van den Bekerom MP. Total elbow arthroplasty: a systematic review. JBJS Rev. 2017; 5(7):e4.
18. Kudo H, Iwano K. Total elbow arthroplasty with a non-constrained surface-replacement prosthesis in patients who have rheumatoid arthritis: a long-term follow-up study. J Bone Joint Surg Am. 1990; 72(3):355–362. PMID:
2312530.

19. Iwamoto T, Ikegami H, Suzuki T, et al. The history and future of unlinked total elbow arthroplasty. Keio J Med. 2018; 67(2):19–25. PMID:
28835585.

20. Kaufmann RA, D'Auria JL, Schneppendahl J. Total elbow arthroplasty: elbow biomechanics and failure. J Hand Surg Am. 2019; 44(8):687–692. PMID:
30770149.

21. Kodama A, Mizuseki T, Adachi N. Macroscopic investigation of failed Kudo type 5 total elbow arthroplasty. J Shoulder Elbow Surg. 2018; 27(8):1380–1385. PMID:
30016691.

22. Kodama A, Mizuseki T, Adachi N. Kudo type-5 total elbow arthroplasty for patients with rheumatoid arthritis: a minimum ten-year follow-up study. Bone Joint J. 2017; 99(6):818–823. PMID:
28566403.
23. Ramirez MA, Cheung EV, Murthi AM. Revision total elbow arthroplasty. J Am Acad Orthop Surg. 2017; 25(8):e166–e174. PMID:
28737619.

24. Figgie MP, Wright TM, Drinkwater D. Bioengineering Working Group. What design and material factors impact the wear and corrosion performance in total elbow arthroplasties? Clin Orthop Relat Res. 2014; 472(12):3770–3776. PMID:
25024029.

25. Aldridge JM 3rd, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis: a 10- to 31-year survival analysis. J Bone Joint Surg Br. 2006; 88(4):509–514. PMID:
16567787.
26. King EA, Favre P, Eldemerdash A, Bischoff JE, Palmer M, Lawton JN. Physiological loading of the Coonrad/Morrey, Nexel, and Discovery elbow systems: evaluation by finite element analysis. J Hand Surg Am. 2019; 44(1):61.e1–61.e9. PMID:
29908927.

27. Jeon IH, Morrey BF, Sanchez-Sotelo J. Ulnar component surface finish influenced the outcome of primary Coonrad-Morrey total elbow arthroplasty. J Shoulder Elbow Surg. 2012; 21(9):1229–1235. PMID:
22104128.

28. Shi LL, Zurakowski D, Jones DG, Koris MJ, Thornhill TS. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J Bone Joint Surg Am. 2007; 89(7):1467–1475. PMID:
17606785.

29. Pham TT, Delclaux S, Huguet S, Wargny M, Bonnevialle N, Mansat P. Coonrad-Morrey total elbow arthroplasty for patients with rheumatoid arthritis: 54 prostheses reviewed at 7 years' average follow-up (maximum, 16 years). J Shoulder Elbow Surg. 2018; 27(3):398–403. PMID:
29306664.

30. Kiran M, Jariwala A, Wigderowitz C. Medium term outcomes of primary and revision Coonrad-Morrey total elbow replacement. Indian J Orthop. 2015; 49(2):233–238. PMID:
26015615.

31. Barthel PY, Mansat P, Sirveaux F, Dap F, Mole D, Dautel G. Is total elbow arthroplasty indicated in the treatment of traumatic sequelae? 19 Cases of Coonrad-Morrey(®) reviewed at a mean follow-up of 5.2 years. Orthop Traumatol Surg Res. 2014; 100(1):113–118. PMID:
24370486.
32. Mansat P, Bonnevialle N, Rongieres M, Mansat M, Bonnevialle P. Experience with the Coonrad-Morrey total elbow arthroplasty: 78 consecutive total elbow arthroplasties reviewed with an average 5 years of follow-up. J Shoulder Elbow Surg. 2013; 22(11):1461–1468. PMID:
24138820.

33. Mansat P, Bonnevialle N, Rongieres M, Mansat M, Bonnevialle P. French Society for Shoulder and Elbow SOFEC. Results with a minimum of 10 years follow-up of the Coonrad/Morrey total elbow arthroplasty. Orthop Traumatol Surg Res. 2013; 99(6 Suppl):S337–S343. PMID:
23932914.

34. Schneeberger AG, Meyer DC, Yian EH. Coonrad-Morrey total elbow replacement for primary and revision surgery: a 2- to 7.5-year follow-up study. J Shoulder Elbow Surg. 2007; 16(3 Suppl):S47–S54. PMID:
16963289.

35. Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis: a ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998; 80(9):1327–1335. PMID:
9759818.

36. Morrey BF, Bryan RS, Dobyns JH, Linscheid RL. Total elbow arthroplasty: a five-year experience at the Mayo Clinic. J Bone Joint Surg Am. 1981; 63(7):1050–1063. PMID:
7276042.

37. Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C. Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop. 2006; 77(2):177–197. PMID:
16752278.

38. Mukka S, Berg G, Hassany HR, Koye AK, Sjoden G, Sayed-Noor AS. Semiconstrained total elbow arthroplasty for rheumatoid arthritis patients: clinical and radiological results of 1-8 years follow-up. Arch Orthop Trauma Surg. 2015; 135(5):595–600. PMID:
25733382.
39. Alizadehkhaiyat O, Al Mandhari A, Sinopidis C, Wood A, Frostick S. Total elbow arthroplasty: a prospective clinical outcome study of Discovery Elbow System with a 4-year mean follow-up. J Shoulder Elbow Surg. 2015; 24(1):52–59. PMID:
25441571.

40. Hastings H 2nd. Minimally constrained elbow implant arthroplasty: the discovery elbow system. Tech Hand Up Extrem Surg. 2004; 8(1):34–50. PMID:
16518239.

41. de Vos MJ, Wagener ML, Hannink G, van der Pluijm M, Verdonschot N, Eygendaal D. Short-term clinical results of revision elbow arthroplasty using the Latitude total elbow arthroplasty. Bone Joint J. 2016; 98(8):1086–1092. PMID:
27482022.

42. Wagener ML, de Vos MJ, Hannink G, van der Pluijm M, Verdonschot N, Eygendaal D. Mid-term clinical results of a modern convertible total elbow arthroplasty. Bone Joint J. 2015; 97(5):681–688. PMID:
25922464.

43. Prkic A, Welsink C, The B, van den, Eygendaal D. Why does total elbow arthroplasty fail today? A systematic review of recent literature. Arch Orthop Trauma Surg. 2017; 137(6):761–769. PMID:
28391430.

44. Krukhaug Y, Hallan G, Dybvik E, Lie SA, Furnes ON. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. J Shoulder Elbow Surg. 2018; 27(2):260–269. PMID:
29332662.

45. Hildebrand KA, Patterson SD, Regan WD, MacDermid JC, King GJ. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2000; 82(10):1379–1386. PMID:
11057465.

46. Rangarajan R, Papandrea RF, Cil A. Distal humeral hemiarthroplasty versus total elbow arthroplasty for acute distal humeral fractures. Orthopedics. 2017; 40(1):13–23. PMID:
28375524.

47. Lovy AJ, Keswani A, Koehler SM, Kim J, Hausman M. Short-term complications of distal humerus fractures in elderly patients: open reduction internal fixation versus total elbow arthroplasty. Geriatr Orthop Surg Rehabil. 2016; 7(1):39–44. PMID:
26929856.
48. Lapner M, King GJ. Elbow arthroplasty for distal humeral fractures. Instr Course Lect. 2014; 63:15–26. PMID:
24720290.
49. Zhang D, Chen N. Total elbow arthroplasty. J Hand Surg Am. 2019; 44(6):487–495. PMID:
30635202.

50. Schoch B, Wong J, Abboud J, Lazarus M, Getz C, Ramsey M. Results of total elbow arthroplasty in patients less than 50 years old. J Hand Surg Am. 2017; 42(10):797–802. PMID:
28823536.

51. McKee MD, Veillette CJ, Hall JA, et al. A multicenter, prospective, randomized, controlled trial of open reduction: internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg. 2009; 18(1):3–12. PMID:
18823799.
52. Barco R, Streubel PN, Morrey BF, Sanchez-Sotelo J. Total elbow arthroplasty for distal humeral fractures: a ten-year-minimum follow-up study. J Bone Joint Surg Am. 2017; 99(18):1524–1531. PMID:
28926381.
53. Jenkins PJ, Watts AC, Norwood T, Duckworth AD, Rymaszewski LA, McEachan JE. Total elbow replacement: outcome of 1,146 arthroplasties from the Scottish Arthroplasty Project. Acta Orthop. 2013; 84(2):119–123. PMID:
23485072.

54. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg. 2009; 18(3):449–456. PMID:
19393935.

55. Amirfeyz R, Blewitt N. Mid-term outcome of GSB-III total elbow arthroplasty in patients with rheumatoid arthritis and patients with post-traumatic arthritis. Arch Orthop Trauma Surg. 2009; 129(11):1505–1510. PMID:
19373479.

56. Giannicola G, Scacchi M, Polimanti D, Cinotti G. Discovery elbow system: 2- to 5-year results in distal humerus fractures and posttraumatic conditions: a prospective study on 24 patients. J Hand Surg Am. 2014; 39(9):1746–1756. PMID:
25063393.

57. Lenich A, Imhoff AB, Siebenlist S. Post-traumatic osteoarthritis of the elbow joint: endoprosthetic options in young patients. Orthopade. 2016; 45(10):844–852. PMID:
27647165.
58. Celli A, Morrey BF. Total elbow arthroplasty in patients forty years of age or less. J Bone Joint Surg Am. 2009; 91(6):1414–1418. PMID:
19487519.

59. Park JG, Cho NS, Song JH, Lee DS, Rhee YG. Clinical outcomes of semiconstrained total elbow arthroplasty in patients who were forty years of age or younger. J Bone Joint Surg Am. 2015; 97(21):1781–1791. PMID:
26537166.

60. Kwak JM, Kholinne E, Sun Y, Lim S, Koh KH, Jeon IH. Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: comparison of arthroscopic and open procedure. Arthroscopy. 2019; 35(4):1083–1089. PMID:
30871900.

61. Kwak JM, Kholinne E, Sun Y, Kim MS, Koh KH, Jeon IH. Clinical results of revision total elbow arthroplasty: comparison of infected and non-infected total elbow arthroplasty. Int Orthop. 2019; 43(6):1421–1427. PMID:
30617613.
62. Farnsworth CW, Schott EM, Benvie AM, et al. Obesity/type 2 diabetes increases inflammation, periosteal reactive bone formation, and osteolysis during Staphylococcus aureus implant-associated bone infection. J Orthop Res. 2018; 36(6):1614–1623. PMID:
29227579.
63. Perretta D, van Leeuwen WF, Dyer G, Ring D, Chen N. Risk factors for reoperation after total elbow arthroplasty. J Shoulder Elbow Surg. 2017; 26(5):824–829. PMID:
28159475.

64. Griffin JW, Werner BC, Gwathmey FW, Chhabra AB. Obesity is associated with increased postoperative complications after total elbow arthroplasty. J Shoulder Elbow Surg. 2015; 24(10):1594–1601. PMID:
26385389.

65. Geurts EJ, Viveen J, van Riet RP, Kodde IF, Eygendaal D. Outcomes after revision total elbow arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019; 28(2):381–386. PMID:
30658776.

66. Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017; 99(4 Supple B):3–10.
67. Ting NT, Della Valle CJ. Diagnosis of periprosthetic joint infection-an algorithm-based approach. J Arthroplasty. 2017; 32(7):2047–2050. PMID:
28343826.

68. Somerson JS, Morrey ME, Sanchez-Sotelo J, Morrey BF. Diagnosis and management of periprosthetic elbow infection. J Bone Joint Surg Am. 2015; 97(23):1962–1971. PMID:
26631998.

69. Drago L, De Vecchi E, Bortolin M, Zagra L, Romano CL, Cappelletti L. Epidemiology and antibiotic resistance of late prosthetic knee and hip infections. J Arthroplasty. 2017; 32(8):2496–2500. PMID:
28390886.

70. Henderson RA, Austin MS. Management of periprosthetic joint infection: the more we learn, the less we know. J Arthroplasty. 2017; 32(7):2056–2059. PMID:
28318868.

71. Pruzansky JS, Bronson MJ, Grelsamer RP, Strauss E, Moucha CS. Prevalence of modifiable surgical site infection risk factors in hip and knee joint arthroplasty patients at an urban academic hospital. J Arthroplasty. 2014; 29(2):272–276. PMID:
23890832.

72. Streubel PN, Simone JP, Morrey BF, Sanchez-Sotelo J, Morrey ME. Infection in total elbow arthroplasty with stable components: outcomes of a staged surgical protocol with retention of the components. Bone Joint J. 2016; 98(7):976–983. PMID:
27365477.
73. Kok TW, Agrawal N, Sathappan SS, Chen WK. Risk factors for early implant-related surgical site infection. J Orthop Surg (Hong Kong). 2016; 24(1):72–76. PMID:
27122517.

74. Spormann C, Achermann Y, Simmen BR, et al. Treatment strategies for periprosthetic infections after primary elbow arthroplasty. J Shoulder Elbow Surg. 2012; 21(8):992–1000. PMID:
22221886.

75. Pope D, Scaife SL, Tzeng TH, Vasdev S, Saleh KJ. Impact of diabetes on early postoperative outcomes after total elbow arthroplasty. J Shoulder Elbow Surg. 2015; 24(3):348–352. PMID:
25499723.

76. Toor AS, Jiang JJ, Shi LL, Koh JL. Comparison of perioperative complications after total elbow arthroplasty in patients with and without diabetes. J Shoulder Elbow Surg. 2014; 23(11):1599–1606. PMID:
25213826.

77. Mraovic B, Suh D, Jacovides C, Parvizi J. Perioperative hyperglycemia and postoperative infection after lower limb arthroplasty. J Diabetes Sci Technol. 2011; 5(2):412–418. PMID:
21527113.

78. Yoon HK, Cho SH, Lee DY, et al. A review of the literature on culture-negative periprosthetic joint infection: epidemiology, diagnosis and treatment. Knee Surg Relat Res. 2017; 29(3):155–164. PMID:
28854760.

79. Peach CA, Nicoletti S, Lawrence TM, Stanley D. Two-stage revision for the treatment of the infected total elbow arthroplasty. Bone Joint J. 2013; 95(12):1681–1686. PMID:
24293600.

80. Rudge WB, Eseonu K, Brown M, et al. The management of infected elbow arthroplasty by two-stage revision. J Shoulder Elbow Surg. 2018; 27(5):879–886. PMID:
29503100.

81. Wagner ER, Ransom JE, Kremers HM, Morrey M, Sanchez-Sotelo J. Comparison of the hospital costs for two-stage reimplantation for deep infection, single-stage revision and primary total elbow arthroplasty. Shoulder Elbow. 2017; 9(4):279–284. PMID:
28932285.

82. Zmistowski B, Pourjafari A, Padegimas EM, et al. Treatment of periprosthetic joint infection of the elbow: 15-year experience at a single institution. J Shoulder Elbow Surg. 2018; 27(9):1636–1641. PMID:
30045830.

83. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013; 56(1):e1–e25. PMID:
23223583.
84. Choi HR, Kwon YM, Freiberg AA, Nelson SB, Malchau H. Periprosthetic joint infection with negative culture results: clinical characteristics and treatment outcome. J Arthroplasty. 2013; 28(6):899–903. PMID:
23523496.

85. Parvizi J, Adeli B, Zmistowski B, Restrepo C, Greenwald AS. Management of periprosthetic joint infection: the current knowledge: AAOS exhibit selection. J Bone Joint Surg Am. 2012; 94(14):e104. PMID:
22810411.
86. Morrey BF, Bryan RS. Infection after total elbow arthroplasty. J Bone Joint Surg Am. 1983; 65(3):330–338. PMID:
6826595.

87. Zhou H, Orvets ND, Merlin G, et al. Total elbow arthroplasty in the United States: evaluation of cost, patient demographics, and complication rates. Orthop Rev (Pavia). 2016; 8(1):6113. PMID:
27114806.

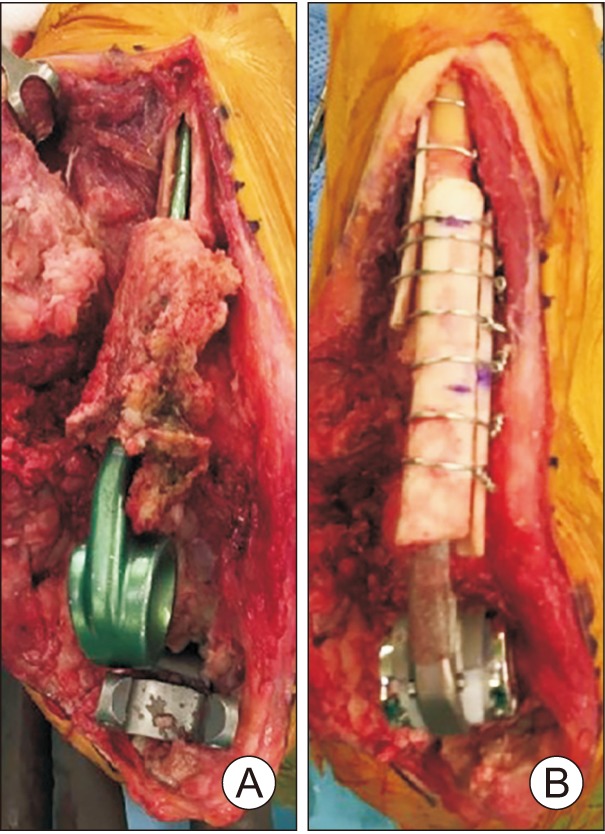
88. Rhee YG, Cho NS, Parke CS. Impaction grafting in revision total elbow arthroplasty due to aseptic loosening and bone loss. J Bone Joint Surg Am. 2013; 95(11):e741–e747. PMID:
23780544.

89. Goldberg SH, Urban RM, Jacobs JJ, King GJ, O'Driscoll SW, Cohen MS. Modes of wear after semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2008; 90(3):609–619. PMID:
18310712.

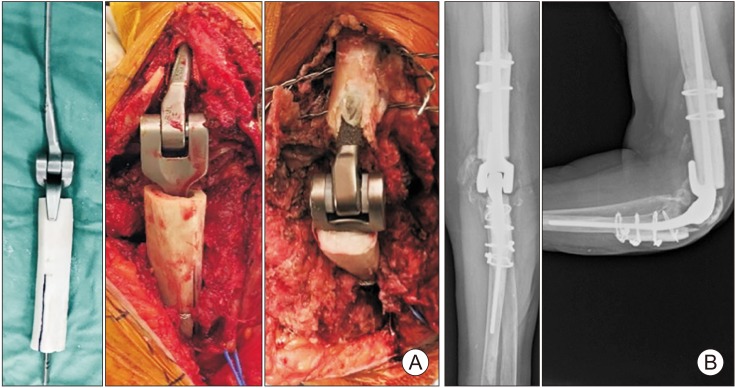
90. Morrey ME, Sanchez-Sotelo J, Abdel MP, Morrey BF. Allograft-prosthetic composite reconstruction for massive bone loss including catastrophic failure in total elbow arthroplasty. J Bone Joint Surg Am. 2013; 95(12):1117–1124. PMID:
23783209.

91. King GJ, Adams RA, Morrey BF. Total elbow arthroplasty: revision with use of a non-custom semiconstrained prosthesis. J Bone Joint Surg Am. 1997; 79(3):394–400. PMID:
9070529.
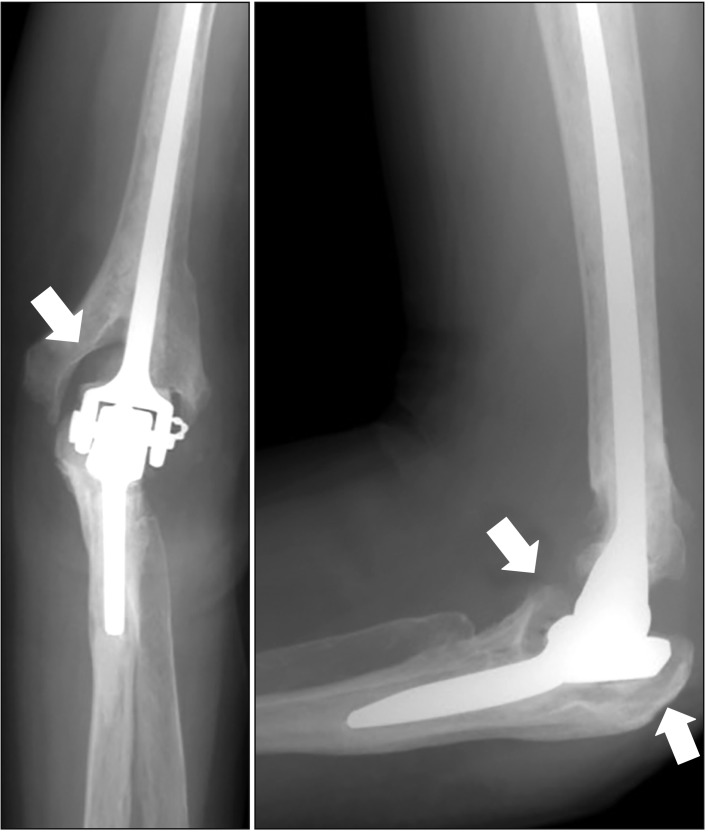
92. Sanchez-Sotelo J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after total elbow arthroplasty: treatment with implant revision and strut allograft augmentation. J Bone Joint Surg Am. 2002; 84(9):1642–1650. PMID:
12208923.
93. Celli A, Arash A, Adams RA, Morrey BF. Triceps insufficiency following total elbow arthroplasty. J Bone Joint Surg Am. 2005; 87(9):1957–1964. PMID:
16140809.

94. Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg. 2011; 20(1):158–168. PMID:
21134667.

95. Dachs RP, Fleming MA, Chivers DA, et al. Total elbow arthroplasty: outcomes after triceps-detaching and triceps-sparing approaches. J Shoulder Elbow Surg. 2015; 24(3):339–347. PMID:
25591460.

96. Solarz MK, Patel MK, Struk AM, et al. A clinical comparison of triceps-sparing and triceps-detaching approaches for revision total elbow arthroplasty. J Hand Surg Am. 2019; 6. 18. [Epub]. DOI:
10.1016/j.jhsa.2019.05.002.

97. Lee H, Vaichinger AM, O'Driscoll SW. Component fracture after total elbow arthroplasty. J Shoulder Elbow Surg. 2019; 28(8):1449–1456. PMID:
31076278.

98. Dachs RP, Vrettos BC, Chivers DA, Du Plessis JP, Roche SJ. Outcomes after ulnar nerve in situ release during total elbow arthroplasty. J Hand Surg Am. 2015; 40(9):1832–1837. PMID:
26254945.

99. Morrey BF, Bryan RS. Revision total elbow arthroplasty. J Bone Joint Surg Am. 1987; 69(4):523–532. PMID:
3571311.

100. Cheung EV, O'Driscoll SW. Total elbow prosthesis loosening caused by ulnar component pistoning. J Bone Joint Surg Am. 2007; 89(6):1269–1274. PMID:
17545430.

101. Renfree KJ, Dell PC, Kozin SH, Wright TW. Total elbow arthroplasty with massive composite allografts. J Shoulder Elbow Surg. 2004; 13(3):313–321. PMID:
15111902.

102. O'Driscoll SW, King GJ. Treatment of instability after total elbow arthroplasty. Orthop Clin North Am. 2001; 32(4):679–695. PMID:
11689380.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download