Abstract
Purpose
To describe current cataract surgery practice patterns and changing trends among Korean ophthalmologists.
Methods
A survey of members of the Korean Society of Cataract and Refractive Surgery was performed in July 2018. One hundred and two (12.7%) of 801 questionnaires were returned for analysis. The data were analyzed using descriptive statistics and compared with previous surveys.
Results
Most of the respondents (75%) had been in practice for 6 or more years and performed an average of 31 cataract surgeries per month. The preferred method for cataract surgery was phacoemulsification (95%); 5% used a femtosecond laser. The use of topical anesthesia markedly increased from 69% (2012) to 80% (2018). The use of optical biometry exceeded that of ultrasound A-scan biometry. A multifocal intraocular lens was used by 76% of the respondents compared with 44% of the respondents in 2012. Topical nonsteroidal anti-inflammatory drugs were used by 70% of the respondents postoperatively. Most (59%) of these anti-inflammatory drugs were prescribed for 4 weeks.
Age-related cataracts are the leading cause of visual impairment, and cataract extraction is the most commonly performed eye operation in the world [1]. Preferred surgical techniques, phacoemulsification equipment, and intraocular lenses (IOLs) have changed over the past years with associated improvements in outcomes and safety [2]. Many surveys have been reported regarding current practice and trends in cataract surgery in the USA, Canada, Japan, and New Zealand [345].
Current practices and trends in cataract surgery have been assessed by the Korean Society of Cataract and Refractive Surgery (KSCRS) since 1995, with the latest results based on the 2012 survey of cataract surgical techniques, IOL preferences, and miscellaneous contemporary issues [678]. An understanding of the current practices for cataract surgery is important because of the rapidly changing nature of cataract surgery. These practices are driven by cost, efficiency, and improved patient-centered care [910].
In this study, we analyzed the survey results of KSCRS members in 2018 regarding the types of cataract surgery performed, the types of implanted IOLs, surgical procedures, postoperative management, and the frequency of complications to create a comprehensive picture of current cataract surgical practice in the Republic of Korea.
In July 2018, 32 multiple choice or open-ended questionnaires were sent via e-mail to 801 members of the KSCRS. The questionnaire used in this study was based on a previous KSCRS survey with some modifications to identify the latest and changing surgical trends, such as newly developed types of multifocal IOLs and biometry equipment or femtosecond laser-assisted cataract surgery (FLACS) [7]. The questionnaire consisted of three major categories: surgeon demographics, cataract surgery-general, cataract surgery-skill, and related complications. Return questionnaires were not marked or labeled to maintain the confidentiality of the respondent, and no financial reward was offered. One hundred and two (12.7%) members completed the questionnaire. IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
Most respondents were 30 to 49 years of age (88%), male (78%), and had more than 6 years of surgical experience (75%). Most respondents also worked for university hospitals (48%), followed by private clinics (31.4%), and eye hospitals (15%). The respondent demographics are shown in Table 1.
The average monthly volume of cataract surgeries performed by KSCRS members was 31 cases. Seventy-two percent performed 1 to 5 post refractive surgeries per month, 5% performed 6 to 10 surgeries, 2% performed >10 surgeries, and 21% did not perform post refractive surgery. These surgeons preferred phacoemulsification (95%) and 5% used a femtosecond laser. None of the members performed planned extracapsular cataract extraction. Surgeons were assisted during the procedures by residents (41%), nurses (16%), and nursing assistants (15%). The surgical instruments were managed and sterilized by nurses (83%) and nursing assistants (15%). Ninety-four percent of the respondents selected the IOL power, and 4% of the respondents had the residents perform this task.
Optical biometry was used by 92% of the respondents for IOL calculations, and ultrasound biometry was used by 73% of the respondents. Seventy-eight percent of respondents used IOLmaster (Carl Zeiss Meditech, Jena, Germany), 73% used ultrasound A-scan biometry, 14% used Lenstar (Haag-Streit, Koeniz, Switzerland), and 8% used ALscan (Nidek, Gamamori, Japan). Thirty-four percent of the respondents used single equipment, 23% used an IOLmaster, and 8% used an ultrasound A-scan. Sixty-six percent used more than two instruments; the most common combination was ultrasound A-scan biometry and the IOLmaster (44%).
Temporal clear corneal incisions were used by 50% of the respondents, followed by a steep axis incision (15%). The temporal site was the preferred incision meridian (57%), with little variation since 2006 (Fig. 2) [7]. A cataract incision size of 2.8 mm was used by 64% of the respondents (from 61% in 2012), and a size of 2.2 mm was used by 31% (from 24% in 2012) [7]. Among ophthalmic viscoelastic devices, HEALON (Johnson & Johnson, New Brunswick, NJ, USA) was used by 65% of the respondents; HEALON GV (Johnson & Johnson) was used by 10%; Viscoat (Alcon Laboratories, Fort Worth, TX, USA) was used by 7%; and HEALON 5 (Johnson & Johnson) was used by 3%. Forceps were used by 68% of the respondents for continuous curvilinear capsulorhexis, a bent needle was used by 24%, and a femtosecond laser was used by 2%. Capsular polishing was performed by 95% of the respondents during surgery; 5% of the respondents did not use this technique. Forty-eight percent of the respondents used both anterior and posterior capsules, while 44% and 3% of the respondents used only an anterior capsule or posterior capsule, respectively.
In 2001, an acrylic IOL was the preferred optic material, exceeding half of the total number of IOLs used (Fig. 3) [6]. In 2018, acrylic was preferred by 98% of the respondents and silicone by 2%; poly (methyl methacrylate) was not used by any respondent (0%). Among the total number of cataract surgeries, 64% of the respondents used a toric IOL less than 5%, and 84% used multifocal IOLs less than 10% (Fig. 4). Twenty-four percent of the respondents did not use multifocal IOLs; and 66% of the respondents treated less than 10 cases per month, while 8% treated 10–50 cases per month. Eighty-seven percent of the respondents also used multifocal IOLs for patients who were treated with corneal refractive surgery, and it constituted less than 30% of the total cataract surgery cases.
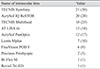
Eighty-two percent of the respondents using multifocal IOLs had been using bifocal IOLs, 48% had been using trifocal IOLs, and 30% had been using both types of IOLs. The types of preferred multifocal IOLs are shown in Table 2.
Forty-seven percent of the respondents did not use oral antibiotics postoperatively, and 31% used oral antibiotics postoperatively for less than 3 days. Forty-one percent of the respondents (from 77% in 2012) prescribed antibiotics for 3 to 7 days. Topical nonsteroidal anti-inflammatory drugs (NSAIDs) were used together with topical steroids by 60% of the respondents, 10% used topical NSAIDs alone, and 30% did not use topical NSAIDs. More than half (53%) of the respondents used topical antibiotics and steroids for 1 month, and 26% of the respondents continued to use topical antibiotics and steroids longer than 1 month. In a similar manner, 52% of the respondents used topical antibiotics and NSAIDs for 1 month postoperatively. Twenty percent of the respondents finished follow-up visits at 1 month postoperatively, 30% finished visits at 3 months, 15% finished visits at 6 months, and 26% continued to visit every year. Most respondents (72%) prescribed reading glasses at 1 month postoperatively.
Ninety-four percent of the respondents (from 80% in 2012) observed posterior capsular rupture during surgery in less than 5% of cases, and 71% observed posterior capsular rupture during surgery in less than 1% of cases. More than half (54%) of the respondents did not observe patients with postoperative endophthalmitis, 23% observed postoperative endophthalmitis once, and 23% observed postoperative endophthalmitis in less than five cases. Fifty-eight percent of those who observed postoperative endophthalmitis estimated that the occurrence was less than 0.1%. More than half (52%) of the respondents observed severe postoperative uveitis, and 63% of these respondents estimated that the occurrence was less than 0.1% of cases.
The occurrences of other complications such as toxic anterior segment syndrome with severe endothelial cell damage, intraocular pressure spikes requiring medication, clinically significant pseudophakic cystoid macular edema, retinal detachment, dysphotopsia, IOL sulcus fixation, and unplanned aphakia are shown in Fig. 5. More than half (53%) of the respondents did not observe IOL subluxation or dislocation in uncomplicated cases over the past 10 years, 16% observed this complication once, 31% observed this complication in less than five cases, and 1% observed this complication in 10 cases or more. Among secondary IOL implantation techniques, conventional scleral fixation with suture material was used by 76% of the respondents; the Hoffmann technique was used by 10%; the iris-fixated IOL technique was used by 10%; and the glued intrascleral haptic fixation was used by 2%.
This survey provides a summary of current practices of KSCRS members performing cataract surgery and describes the changing trends in clinical practice. Most of the respondents (75%) had been in practice for 6 or more years and had performed an average of 31 cataract surgeries per month. There was a moderate increase in the number of respondents treating 16 to 50 cases per month from 2012 (55%) to 2018 (62%), and over 51 cases from 2012 (7%) to 2018 (11%). There was a decreased number of respondents treating 6–15 cases from 2012 (33%) to 2018 (18%).
This survey involved the latest practice of KSCRS members in cataract surgery; some questions in the survey were modified from their original version used in previous surveys. Some questionnaire items such as FLACS, cataract surgery after refractive surgery, and NSAIDS eye drops were added; and the categories of biometry equipment, incisions, continuous curvilinear capsulorhexis, multifocal IOLs, toric IOLs, and postoperative management were refined [7].
Because no surgeon performed planned extracapsular cataract extraction and the majority (95%) of respondents used phacoemulsification, there was a marked increase in the number of respondents who used topical anesthesia, from 69% (2012) to 80% (2018), and a decreased use of retrobulbar block, from 10% to 5% [7]. These changes also seemed to affect the preferred smaller size of incisions.
The first report of FLACS was included in the current survey. In the 2012 survey, 32% of the respondents expressed an interest in FLACS however, was not used in practice. Only 5% of the respondents in this survey performed FLACS, which showed that FLACS still had a limited role in the Republic of Korea. Possible explanations include the high cost of purchase and operation, as well as the lack of clear advantages of FLACS over traditional phacoemulsification [111213]. According to the 2018 American Society of Cataract and Refractive Surgery clinical survey, only an average of 8% of cataract patients were treated using FLACS. USA respondents performed FLACS more often, with 10% of cataract patients in the USA. Treated with FLACS vs. 6% of non-USA patients [14]. Another survey from the Canadian Ophthalmological Society (COS) reported that the use of FLACS had increased from 2014 (8%) to 2015 (18.9%), then started to decline in 2016 (17.4%) and in 2017 (11.8%) [15]. However, we cannot predict changes in the use FLACS from the results of this survey alone and additional studies are needed.
There was a marked increase in the number of respondents who were using optical biometry. Optical biometry was used by 92% of the respondents and ultrasound biometry by 73% of the respondents. For example, the use of IOLmaster increased from 56% in 2012 to 78% in 2018. As new optical biometry equipment has been introduced with a newer generation of IOL calculation formulas, optical biometry has partially replaced conventional ultrasound A-scan biometry. Optical biometry is convenient to use, reproducible, and has an installed calculation formula. Several favorable results in cases implanted with multifocal or toric IOLs seem to be related to its increasing popularity.
There was a marked increase in the number of respondents who were using multifocal IOLs, from 44% (2012) to 76% (2018). This was higher than the COS report of approximately 50% in 2017; two-thirds was the proportion reported by the American Society of Cataract and Refractive Surgery clinical survey in 2018 [1415].
The most current survey included the first use of NSAIDS eye drops. These were used by 70% of the respondents postoperatively, and the majority prescribed eye drops for 4 weeks (59%). This was similar to the COS report, which showed that 75.9% of the respondents prescribed NSAIDS and 52.4% prescribed these drops for 4 weeks [15].
This survey has several limitations. Response bias could have affected the results although there were few open-ended questions. The questionnaire primarily involved multiple choice questions without the option of responses that were not listed. Because the response represented only 12.7% of the KSCRS members (20.6% in 2012), the results may not represent the opinions and practices of the majority of ophthalmologists in the Republic of Korea.
In summary, this study provides a comprehensive update of the present cataract surgery practices of KSCRS members. The results emphasize the growing role of premium IOLs, optical biometry, and the use of topical anesthesia. A follow-up survey concerning the use of FLACS, post refractive cataract surgery, the use of premium IOLs, and changes in postoperative medications is required.
Figures and Tables
 | Fig. 4Percentages of (A) toric intraocual lens and (B) multifocal intraocual lens implanted after phacoemulsification among the total number of cataract surgeries. |
 | Fig. 5The complication rate of toxic anterior segment syndrome (TASS) with severe endothelial cell damage, intraocular pressure (IOP) spikes requiring medication, clinically significant pseudophakic cystoid macular edema (CME), retinal detachment, intraocular lens (IOL) subluxation/dislocation, dysphotopsia, IOL sulcus fixation, and unplanned aphakia. |
References
1. Day AC, Gore DM, Bunce C, Evans JR. Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery. Cochrane Database Syst Rev. 2016; 7:CD010735.

2. Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser-assisted lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refract Surg. 2013; 39:1297–1306.
3. Leaming DV. Practice styles and preferences of ASCRS members: 2003 survey. J Cataract Refract Surg. 2004; 30:892–900.
4. Pick ZS, Leaming DV, Elder MJ. The fourth New Zealand cataract and refractive surgery survey: 2007. Clin Exp Ophthalmol. 2008; 36:604–619.
5. Oshika T, Amano S, Araie M, et al. Current trends in cataract and refractive surgery in Japan: 1999 survey. Jpn J Ophthalmol. 2001; 45:383–387.

6. Yoon SC, Jung JW, Sohn HJ, Shyn KH. Cataract and refractive surgery in: a survey of KSCRS members from 1995-2006. Korean J Ophthalmol. 2009; 23:142–147.
7. Wi JM, Moon HS, Kim KH, Shyn KH. 2012 survey of KSCRS and KOS member: current trends in cataract surgery in Korea. J Korean Ophthalmol Soc. 2015; 56:1181–1187.

8. Shyn KH, Baek NH, Lee JH, et al. 95 survey of Korean Society of Cataract and Refractive Surgery members. J Korean Ophthalmol Soc. 1998; 39:892–899.
9. Ianchulev T, Litoff D, Ellinger D, et al. Office-based cataract surgery: population health outcomes study of more than 21,000 cases in the United States. Ophthalmology. 2016; 123:723–728.
10. Chen CL, Lin GA, Bardach NS, et al. Preoperative medical testing in Medicare patients undergoing cataract surgery. N Engl J Med. 2015; 372:1530–1538.
11. Havnaer AG, Greenberg PB, Cockerham GC, et al. Cataract surgery practices in the United States Veterans Health Administration. J Cataract Refract Surg. 2017; 43:543–551.

12. Popovic M, Campos-Moller X, Schlenker MB, Ahmed II. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 eyes. Ophthalmology. 2016; 123:2113–2126.
13. Chen X, Xiao W, Ye S, et al. Efficacy and safety of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract: a meta-analysis of randomized controlled trials. Sci Rep. 2015; 5:13123.

14. Braga-Mele R. ASCRS clinical survey 2018 [Internet]. [place unknown]: Eyeworld News Service;2018. cited 2019 Jul 1. Available from: http://supplements.eyeworld.org/eyeworld-supplements/december-2018-clinical-survey.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download