This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Desmoplastic melanoma (DM) is a rare variant of malignant melanoma and constitutes less than 1% of all cutaneous melanomas
1. Like all melanomas, especially melanomas of the skin, DM is easily diagnosed in the majority of cases, but some cases can mimic other tumors and cause misdiagnoses. Furthermore, because of the aggressive local behavior and high local recurrence rate of DM, proper diagnosis is essential
23. Recently, there has been much speculation on the relationship between Parkinson's disease (PD) and melanoma, and according to recent retrospective, case-controlled studies, patients with PD are at 4-fold greater risk of having a history of melanoma, and conversely, patients with melanoma are at similar risk of developing PD. In a recent prospective study conducted in North America patients with PD were found to be at 7-fold greater risk of developing melanoma
4.
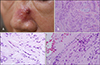
A 81-year-old female presented with an erosive, crusted nodule on a violaceous indurated plaque on her nose (
Fig. 1A). We received the patient's consent form about publishing all photographic materials. She had been diagnosed with PD 5 years previously and had been treated with levodopa. The clinical differential diagnoses included basal cell carcinoma, squamous cell carcinoma, Merkel cell carcinoma, cutaneous lymphoma, and dermal scar tissue. Histopathologic examination revealed hyperchromatic spindle-shaped cells in dermis mixed with dense collagen bundles (
Fig. 1B, C). Neurotropic features and a tendency for malignant, spindle-shaped cells to invade nerves in the dermis were also presented (
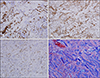
Fig. 1D). Immunohistochemical staining for S-100 protein, CD 68, cyclin D1, Trichrome, produced positive results for infiltrating spindle-shaped cells but HMB45 was negative (
Fig. 2). Based on these findings, a final diagnosis of DM was made (cT4aN0M0, stage IIB). The patient was transferred to another hospital for surgical excision and local skin flap. DM frequently poses diagnostic challenges for dermatologists. Biopsy is necessary for precise diagnosis and proper treatment, because DM is a distinct form of cutaneous melanoma with unique histopathologic and immunohistochemical staining features. Physicians should consider counseling melanoma patients about the risk of PD and undertaking cutaneous melanoma surveillance in PD patients. A family history of melanoma and lighter hair and skin color confer higher risks of developing PD, and having a first-degree relative with either disease conveys an increased risk of developing the other. Possible connections between the two diseases explored, include pigmentation genes in neural-derived cells, pesticides, melanocortin 1 receptor polymorphisms, and abnormal cellular autophagy
5.
A retrospective review was performed in patient with malignant melanoma to find the association with PD from 2007 to 2017 in our center. Interestingly, 3 out of 43 patients (7%) with malignant melanoma had PD. Among melanoma patients over 65 years old, comorbid PD patients were 18 patients (16.7%). Future research on this topic will undoubtedly provide further insight into the cause of this relationship as well as necessary screening or patient counseling measures that should be implemented.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download