INTRODUCTION
Delta-shaped gastroduodenostomy (DSG) [
1] is regarded worldwide as the only acceptable Billroth-I (B-I) anastomotic method in patients undergoing totally laparoscopic distal gastrectomy (TLDG). Although DSG can be performed within a short timeframe and with a wide lumen, it requires additional dissection of the duodenum, which may lead to ischemia. Moreover, the duodenum must be twisted for anastomosis, a procedure that is technically demanding. Many of the developed techniques have sought to overcome these drawbacks of DSG [
234567].
The book binding technique (BBT), first introduced in 2013, utilizes intracorporeal triangular anastomosis [
24], and was developed to overcome the drawbacks of DSG. The anastomosis is triangular in shape and made by the triple stapling technique. The first anastomosis step involves anastomosing the posterior walls of the duodenal stump and the remnant stomach. At this point, the four layers of the gastroduodenal wall are shaped like a bound book, hence the name. After making the anastomosis between the duodenum and the remnant stomach, the anterior wall of the anastomosis are resected. The anterior hole is closed using 2 applications of the linear stapler to form the tip of a triangle.
Although BBT does not require additional dissection or twisting of the duodenum, it has other drawbacks, and a modified book binding technique (MBBT) has recently been developed. The current study describes the method of MBBT, and evaluates its safety, feasibility, and clinical outcomes.
RESULTS
A total of 33 patients underwent TLDG with MBBT, and none experienced any intraoperative complications or required open conversion. The patient characteristics and surgical outcomes are summarized in
Tables 1 and
2, respectively. The mean age of the patients was 63.5 years, and the male to female ratio was 1.39:1. The mean body mass index was 23.6 kg/m
2, and 23 (70%) patients had comorbidities. All patients underwent D2 lymph node dissection, with a mean number of 36.7 lymph nodes retrieved. The mean operation time was 277.6 minutes, and the mean anastomosis time, defined as the time required to create a small hole on the superior edge of the duodenal transection line to complete anastomosis, was 51.9 minutes. The mean estimated blood loss was 100 mL, and the mean number of linear stapler cartridges used was 4.1. The mean postoperative hospital stay was 10.2 days. Seven patients (21.2%) experienced postoperative complications, including 2 with pneumonia, 2 with atelectasis, 1 with gastroparesis, and 2 with anastomosis-related complications. The anastomosis related-complications included one stricture and one leakage. There was one major complication, defined as grade IIIa according to the Clavien-Dindo classification [
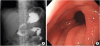
8]. The patient was a 73-year-old male with a history of coronary stenting for angina. The tumor was located in the proximal antrum. The patient underwent TLDG with MBBT, and the entry hole was closed using Endo-stitch (Medtronic Ltd). There were no intraoperative complications, and UGIS was performed on postoperative day 5 with no specific findings. The patient was allowed sips of water and the diet was advanced. On postoperative day 8, he complained of abdominal pain and underwent CT on postoperative day 9. A small defect in the anterior wall of the anastomosis site was detected, and the patient underwent conservative treatment, and EGD was performed on postoperative day 17. No gross perforation was apparent, but severe inflammation was evident around the anastomosis; thus, we decided to maintain a more conservative treatment. On postoperative day 25, EGD was performed again, which revealed slight stenosis but reduced inflammation. Diet was started again but he complained of postprandial abdominal distention and discomfort. EGD was performed again on postoperative day 31, which again revealed stenosis at the anastomosis site, and balloon dilatation was performed. The diet was started again 1 day after balloon dilatation, and the patient was discharged on postoperative day 35.
Table 1
Patient characteristics

|
Variables |
Value |
|
Age (yr) |
63.5±12.8 |
|
Sex |
|
|
Male |
19 (57.6) |
|
Female |
14 (42.4) |
|
Body mass index (kg/m2) |
23.6±2.7 |
|
No. of comorbidities |
|
|
0 |
10 (30.3) |
|
1 |
4 (12.1) |
|
≥2 |
19 (57.6) |
|
Tumor location*
|
|
|
Middle |
13 (39.4) |
|
Lower |
20 (60.6) |
|
Tumor size (cm) |
2.8±1.6 |
|
T†
|
|
|
T1a |
15 (45.5) |
|
T1b |
13 (39.4) |
|
T2 |
1 (3.0) |
|
T3 |
2 (6.1) |
|
T4a |
2 (6.1) |
|
N†
|
|
|
N0 |
28 (84.8) |
|
N1 |
4 (12.1) |
|
N2 |
1 (3.0) |
|
Stage†
|
|
|
IA |
26 (78.8) |
|
IB |
2 (6.1) |
|
IIA |
1 (3.0) |
|
IIB |
3 (9.1) |
|
IIIA |
1 (3.0) |

Table 2
Surgical outcomes

|
Variables |
Value |
|
Conversion to open surgery |
0 (0) |
|
Combined resection†
|
2 (6.1) |
|
Extent of lymph node dissection*
|
|
|
D1+ |
0 (0) |
|
D2 |
33 (100.0) |
|
No. of retrieved lymph nodes |
36.7±13.8 |
|
Operation time (min) |
277.6±37.1 |
|
Anastomosis time (min) |
51.9±15.7 |
|
Estimated blood loss (mL) |
100±55.6 |
|
Linear stapler cartridges used (No.) |
4.1±0.3 |
|
Time to first flatus (day) |
3.8±0.8 |
|
Postoperative hospital stays (day) |
10.2±5.1 |
|
Postoperative complications |
|
|
Leakage |
1 (3) |
|
Stenosis |
1 (3) |
|
Gastric stasis |
1 (3) |
|
Pulmonary |
4 (12.1) |

All patients underwent follow-up EGD 6 months after gastrectomy. The endoscopic findings were evaluated based on gastric residue, the degree of gastritis, and bile reflux (RGB) classification (
Table 3) [
9].
Table 3
Gastric residue, the degree of gastritis, and bile reflux classification
|
Variables |
Value |
|
Residue |
|
|
0 |
19 (59.4) |
|
1 |
7 (21.9) |
|
2 |
4 (12.5) |
|
3 |
2 (6.3) |
|
Gastritis |
|
|
0 |
10 (31.3) |
|
1 |
16 (50.0) |
|
2 |
5 (15.6) |
|
3 |
1 (3.1) |
|
Bile reflux |
|
|
0 |
13 (40.6) |
|
1 |
19 (59.4) |

DISCUSSION
Anastomosis is important for safety and good functional outcomes in patients undergoing totally laparoscopic gastrectomy. Although DSG is both safe and effective, it has several drawbacks, making it unacceptable to some surgeons; this has led to the development of the BBT.
Although the BBT is effective for intracorporeal gastroduodenostomy, we have found that this method has some drawbacks, suggesting the need for modifications that improve the technique. The first step of the modifications was to cut the lesser curvature side of the duodenal stump. All the linear staplers have some dead space at their tips, preventing the anastomosis of the entire posterior wall of the duodenum. In addition, the superior edge of the duodenal stump could be punctured by the sharp tip of the anvil during anastomosis. This is not a major problem since this part is removed; however, if problems were experienced during surgery, the lesser curvature side of the duodenum was opened prior to the anastomosis. This extra procedure enabled the entire posterior wall of the duodenal stump to be used for anastomosis and prevented unexpected perforations.
In the second step, the remnant stomach and the duodenal stump were attached by interrupted sutures prior to anastomosis. It is difficult to insert the staplers during intracorporeal gastroduodenostomy, and aligning both ends for anastomosis after stapler insertion is complicated. To overcome this problem, the two ends were attached prior to inserting the stapler, making insertion of the staplers easier. The sutures were also useful for aligning the two ends of the anastomosis.
In the third step, a 5 mm rather than a 12 mm sized trocar was inserted into the left lower quadrant. The linear stapler was inserted through the umbilical trocar and the camera was moved to the right lower 12 mm sized trocar. Relative to larger trocars, a 5 mm sized trocar is associated with reduced pain, better cosmetic results, and a reduction in other trocar-related complications [
10]. Unlike DSG, the MBBT does not require twisting. In addition, inserting the linear stapler through the umbilical trocar increases the comfort of the operator because the stapler and the site of anastomosis are aligned. Therefore, there was no need for a 12 mm sized trocar in the left lower abdomen. Moreover, operators familiar with reduced port surgery can complete the operation using three trocars; three such patients were included in this study.
In the fourth step, the anterior hole was closed by hand sewing rather than by using a linear stapler. Initial attempts to close with a linear stapler placed the superior edge of the anastomosis at risk of incomplete closure. Moreover, both DSG and the BBT are more costly due to the need for many linear stapler cartridges. Closing using a hand sewing technique enabled identification of the correct edge and complete closure of the entire layer. In this study, the mean number of linear stapler cartridges used was 4.1±0.3. By contrast, DSG requires at least five cartridges and the original BBT requires at least six. Moreover, other intracorporeal gastroduodenostomy procedures require at least five to six cartridges [
2567]. Thus, use of the MBBT allows successful anastomosis with fewer linear stapler cartridges.
In this study, the mean postoperative hospital stay was 10.2 days; the advantage of minimally invasive surgery is that the patient recovers fast, resulting in a short postoperative hospital stay. The mean postoperative hospital stay of 10.2 days is somewhat longer than the average, but similar to that reported for the initial experience with new procedures in other studies [
56]. Given that this was an initial experience, we checked the UGIS on postoperative day 5 and started the diet if there were no abnormal findings. After this initial experience, we no longer routinely checked the UGIS and the postoperative hospital stay was shortened.
In this study, all patients underwent D2 lymph node dissection, which is not recommended for T1 cancers in the Japanese Gastric Cancer Treatment Guideline [
11], and weakly recommended in the Korean Gastric Cancer Treatment Guideline [
12]. D2 lymph node dissection is the recommended procedure at our institute, because lymph node metastasis cannot be completely excluded even if it is clinically N0. Thus, all patients included in this study underwent D2 lymph node dissection despite being diagnosed with a T1 cancer. Recently, D1+ lymph node dissection has been performed more frequently for T1 cancer.
There were five complications other than anastomosis related complications: Four cases of lung related complications, two cases of atelectasis, and two cases of pneumonia. The mean age of patients with lung related complications was 77 years. In elderly patients, lung related complications can occur more often than in young patients [
13]. All patients recovered well with appropriate medication and physical therapy.
Two patients in this study experienced anastomosis-related complications. One patient showed leakage in UGIS, and after conservative treatment, the leakage was resolved. However, stenosis later developed; because the stenosis did not improve, even with careful treatment, the patient was eventually treated with endoscopic balloon dilation. A second patient developed symptoms including vomiting, especially after eating. EGD showed severe edema and ulceration of the anastomosis site. This patient was also managed with conservative treatment, and the stenosis was resolved. No patient required a re-operation, and the rate of anastomosis-related complications was similar to those of other studies reporting early experience with new techniques [
1415].
DSG is the most popular B-I anastomotic method in patients undergoing TLDG. Although the BBT method overcomes the drawbacks of DSG [
16], it has its own weaknesses. We report results obtained using a MBBT method. Although this new method has the drawbacks of taking a long time to complete and being difficult to perform if the operator is not familiar with laparoscopic suturing, it compensates for the weak points of DSG and BBT. MBBT does not require additional dissection or twisting of the duodenum. In addition, MBBT may remove the potential risk of free perforation of the duodenum during anastomosis, and can reduce the size of the trocar. It also reduces the number of linear stapler cartridges used for surgery, which is economical.
In conclusion, the MBBT is both safe and feasible, with acceptable surgical outcomes, and may be a good alternative option for intracorporeal anastomosis in patients with TLDG. However, this study was not a comparative study and included only short-term follow-up data. Therefore, long term comparative studies are needed to fully assess the utility of this technique.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download