Abstract
Objectives
Materials and Methods
Results
Figures and Tables
Fig. 1
Schematic drawing of short dental implant use in patients with insufficient residual bone volume due to sinus pneumatization (A) or mandible atrophy (B).

Fig. 2
Marginal bone loss (MBL) evaluation used in this study, reference lines were drawn to calculate bone loss on the mesial and distal sides of implant: longitudinal implant axis (“1”), horizontal line at the most coronal level of the implant collar (“2”), horizontal lines at the most coronal level of bone-to-implant contact at the mesial and distal sites (“3” and “4”). MBL measurement in a Stella implant (Shinhung; A) and Luna implant (Shinhung; B).

Fig. 3
Panoramic radiograms of a 76-year-old female who had squamous cell cancer, treated with maxillary mass resection and radiotherapy on the left, radical neck dissection and radiotherapy due to neck metastasis on the right (A). A 4.5 mm×7 mm Stella (Shinhung) was installed in the 47 tooth position (arrow; B). The implant achieved good stability and bone integration, and showed acceptable bone loss at 3 years (arrows; C, D).

Fig. 4
Panoramic radiogram of a 72-year-old male with osteomyelitis and a history of hypertension and diabetes. A. Preoperation radiogram. B. A 4 mm×7 mm Stella (Shinhung) implant was installed in the 37 tooth position (arrow). C, D. The implant achieved good stability and bone integration, and showed acceptable bone loss at 1 year (arrows).

Fig. 5
Panoramic radiogram of a 67-year-old female who had hypertension and osteomyelitis in the posterior right mandible. A. A previous implant installed in the 37 tooth position failed due to bone resorption. B. A 4 mm×7 mm Luna (Shinhung) implant was placed at the 16 tooth position (arrow), and a 4.5 mm×7 mm Stella (Shinhung) implant was placed at the 47 tooth position (arrow) after removal of the failed implant. C, D. The two implants showed good stability and acceptable bone loss on follow-up examination (arrows).

Table 1
Distribution of patients in medical history groups

Table 2
Short dental implant installation locations
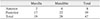
| Maxilla | Mandible | Total | |
|---|---|---|---|
| Anterior | 2 | 6 | 8 |
| Posterior | 17 | 22 | 39 |
| Total | 19 | 28 | 47 |
Table 3
Prosthesis data of 45 success implants

| Types of prosthesis | No. of implants |
|---|---|
| Single crown | 19 |
| Multiple fixed prosthesis | 22 |
| Removable overdenture | 4 |
Table 4
Survival rate of the 47 short dental implants

| Diameter (mm) | Success/fail (total) | Survival rate (%) |
|---|---|---|
| 4.0 | 36/2 (38) | 94.74 |
| 4.5 | 8/0 (8) | 100 |
| 5.0 | 1/0 (1) | 100 |
| Total | 45/2 (47) | 95.74 |
Table 5
Marginal bone loss (MBL) evaluation on the mesial and distal aspects of short dental implants at 3 months, 1 year, and 2 years

Acknowledgements
Notes
Authors' Contributions All authors read and approved the final manuscript. T.T.H.N. read and wrote the manuscript, M.Y.E. prepared retrospective data and wrote the manuscript, Y.J.C. prepared all figures and references, H.M. revised and corrected the manuscript, and S.M.K. designed and wrote the entire article.
Ethics Approval and Consent to Participate This retrospective data analysis was approved by the Institutional Review Board of Seoul National University (S-D20180022).
How to cite this article Nguyen TTH, Eo MY, Cho YJ, Myoung H, Kim SM. 7-mm-long dental implants: retrospective clinical outcomes in medically compromised patients. J Korean Assoc Oral Maxillofac Surg 2019;45:260–266. https://doi.org/10.5125/jkaoms.2019.45.5.260




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download