1. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. International Urogynecological Association. International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010; 29:4–20. PMID:
19941278.

2. Handa VL, Garrett E, Hendrix S, Gold E, Robbins J. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004; 190:27–32. PMID:
14749630.

3. Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014; 123:1201–1206. PMID:
24807341.

4. Swift S, Woodman P, O'Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005; 192:795–806. PMID:
15746674.

5. Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, et al. Pelvic Floor Disorders Network. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009; 114:600–609. PMID:
19701041.

6. Lee U, Raz S. Emerging concepts for pelvic organ prolapse surgery: what is cure? Curr Urol Rep. 2011; 12:62–67. PMID:
21140299.

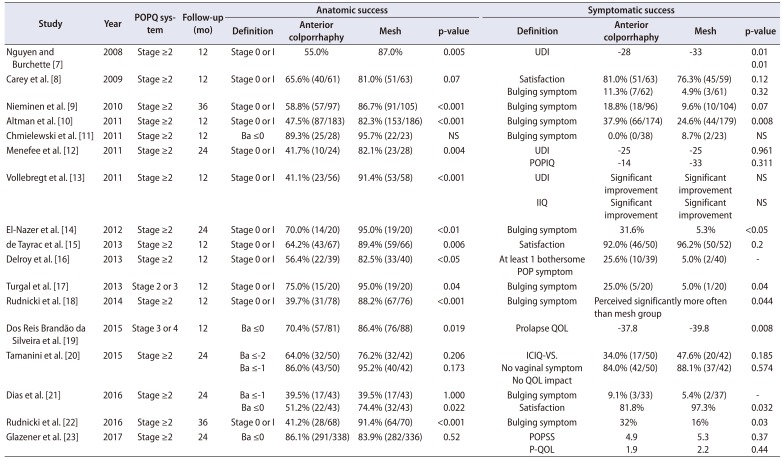
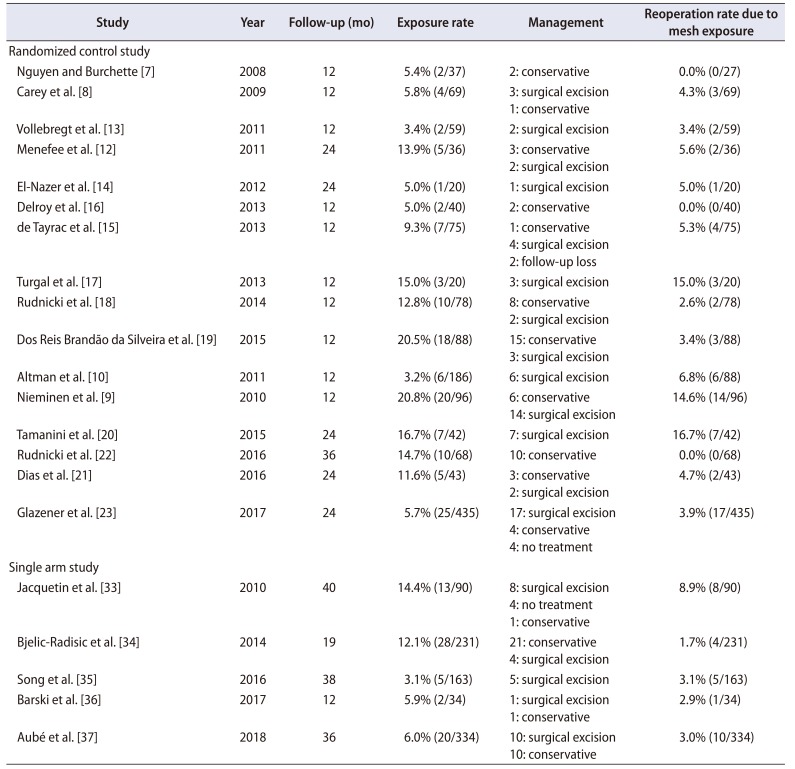
7. Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008; 111:891–898. PMID:
18378748.
8. Carey M, Higgs P, Goh J, Lim J, Leong A, Krause H, et al. Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. BJOG. 2009; 116:1380–1386. PMID:
19583714.

9. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010; 203:235.e1–235.e8. PMID:
20494332.

10. Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C. Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011; 364:1826–1836. PMID:
21561348.

11. Chmielewski L, Walters MD, Weber AM, Barber MD. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol. 2011; 205:69.e1–69.e8. PMID:
21545996.

12. Menefee SA, Dyer KY, Lukacz ES, Simsiman AJ, Luber KM, Nguyen JN. Colporrhaphy compared with mesh or graft-reinforced vaginal paravaginal repair for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol. 2011; 118:1337–1344. PMID:
22067717.
13. Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG. 2011; 118:1518–1527. PMID:
21864325.

14. El-Nazer MA, Gomaa IA, Ismail Madkour WA, Swidan KH, El-Etriby MA. Anterior colporrhaphy versus repair with mesh for anterior vaginal wall prolapse: a comparative clinical study. Arch Gynecol Obstet. 2012; 286:965–972. PMID:
22648445.

15. de Tayrac R, Cornille A, Eglin G, Guilbaud O, Mansoor A, Alonso S, et al. Comparison between trans-obturator transvaginal mesh and traditional anterior colporrhaphy in the treatment of anterior vaginal wall prolapse: results of a French RCT. Int Urogynecol J. 2013; 24:1651–1661. PMID:
23512113.

16. Delroy CA, Castro Rde A, Dias MM, Feldner PC Jr, Bortolini MA, Girão MJ, et al. The use of transvaginal synthetic mesh for anterior vaginal wall prolapse repair: a randomized controlled trial. Int Urogynecol J. 2013; 24:1899–1907. PMID:
23632800.

17. Turgal M, Sivaslioglu A, Yildiz A, Dolen I. Anatomical and functional assessment of anterior colporrhaphy versus polypropylene mesh surgery in cystocele treatment. Eur J Obstet Gynecol Reprod Biol. 2013; 170:555–558. PMID:
23916584.

18. Rudnicki M, Laurikainen E, Pogosean R, Kinne I, Jakobsson U, Teleman P. Anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: a randomised controlled trial. BJOG. 2014; 121:102–110. discussion 110–1.

19. Dos Reis Brandão da Silveira S, Haddad JM, de Jármy-Di Bella ZI, Nastri F, Kawabata MG, da Silva Carramão S, et al. Multicenter, randomized trial comparing native vaginal tissue repair and synthetic mesh repair for genital prolapse surgical treatment. Int Urogynecol J. 2015; 26:335–342. PMID:
25199496.

20. Tamanini JT, de Oliveira Souza Castro RC, Tamanini JM, Castro RA, Sartori MG, Girão MJ. A prospective, randomized, controlled trial of the treatment of anterior vaginal wall prolapse: medium term followup. J Urol. 2015; 193:1298–1304. PMID:
25305357.

21. Dias MM, de A Castro R, Bortolini MA, Delroy CA, Martins PC, Girão MJ, et al. Two-years results of native tissue versus vaginal mesh repair in the treatment of anterior prolapse according to different success criteria: a randomized controlled trial. Neurourol Urodyn. 2016; 35:509–514. PMID:
25820682.

22. Rudnicki M, Laurikainen E, Pogosean R, Kinne I, Jakobsson U, Teleman P. A 3-year follow-up after anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: a randomised controlled trial. BJOG. 2016; 123:136–142. PMID:
26420345.

23. Glazener CM, Breeman S, Elders A, Hemming C, Cooper KG, Freeman RM, et al. PROSPECT study group). Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2017; 389:381–392. PMID:
28010989.

24. Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016; 11:CD004014. PMID:
27901278.

25. Sung VW, Rogers RG, Schaffer JI, Balk EM, Uhlig K, Lau J, et al. Society of Gynecologic Surgeons Systematic Review Group. Graft use in transvaginal pelvic organ prolapse repair: a systematic review. Obstet Gynecol. 2008; 112:1131–1142. PMID:
18978116.

26. Feiner B, Jelovsek JE, Maher C. Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG. 2009; 116:15–24.

27. Bako A, Dhar R. Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:103–111. PMID:
18779916.

28. Food and Drug Administration. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. Food and Drug Administration;2011.
29. Skoczylas LC, Turner LC, Wang L, Winger DG, Shepherd JP. Changes in prolapse surgery trends relative to FDA notifications regarding vaginal mesh. Int Urogynecol J. 2014; 25:471–477. PMID:
24081497.

30. NICE Guidance - Urinary incontinence and pelvic organ prolapse in women:management: © NICE (2019) Urinary incontinence and pelvic organ prolapse in women: management. BJU Int. 2019; 123:777–803. PMID:
31008559.
31. Petri E, Ashok K. Comparison of late complications of retropubic and transobturator slings in stress urinary incontinence. Int Urogynecol J. 2012; 23:321–325. PMID:
21845508.

32. MacDonald S, Terlecki R, Costantini E, Badlani G. Complications of transvaginal mesh for pelvic organ prolapse and stress urinary incontinence: tips for prevention, recognition, and management. Eur Urol Focus. 2016; 2:260–267. PMID:
28723371.

33. Jacquetin B, Fatton B, Rosenthal C, Clavé H, Debodinance P, Hinoul P, et al. Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 3-year prospective follow-up study. Int Urogynecol J. 2010; 21:1455–1462. PMID:
20683579.

34. Bjelic-Radisic V, Aigmueller T, Preyer O, Ralph G, Geiss I, Müller G, et al. Austrian Urogynecology Working Group. Vaginal prolapse surgery with transvaginal mesh: results of the Austrian registry. Int Urogynecol J. 2014; 25:1047–1052. PMID:
24519644.

35. Song W, Kim TH, Chung JW, Cho WJ, Lee HN, Lee YS, et al. Anatomical and functional outcomes of prolift transvaginal mesh for treatment of pelvic organ prolapse. Low Urin Tract Symptoms. 2016; 8:159–164. PMID:
27619780.

36. Barski D, Arndt C, Gerullis H, Yang J, Boros M, Otto T, et al. Transvaginal PVDF-mesh for cystocele repair: a cohort study. Int J Surg. 2017; 39:249–254. PMID:
28192248.

37. Aubé M, Guérin M, Rheaume C, Tu LM. Efficacy and patient satisfaction of pelvic organ prolapse reduction using transvaginal mesh: a Canadian perspective. Can Urol Assoc J. 2018; 12:E432–E437. PMID:
29989915.

38. Whiteside JL, Weber AM, Meyn LA, Walters MD. Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol. 2004; 191:1533–1538. PMID:
15547521.

39. Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006; 195:1837–1840. PMID:
17132485.

40. Elliott CS, Yeh J, Comiter CV, Chen B, Sokol ER. The predictive value of a cystocele for concomitant vaginal apical prolapse. J Urol. 2013; 189:200–203. PMID:
23174246.

41. Eilber KS, Alperin M, Khan A, Wu N, Pashos CL, Clemens JQ, et al. Outcomes of vaginal prolapse surgery among female Medicare beneficiaries: the role of apical support. Obstet Gynecol. 2013; 122:981–987. PMID:
24104778.
42. Liu JS, Nettey O, Vo AX, Hofer MD, Flury SC, Kielb SJ. Prolapse repair with and without apical resuspension-Practice patterns among certifying American urologists. Neurourol Urodyn. 2017; 36:344–348. PMID:
26547063.

43. Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016; 10:CD012376. PMID:
27696355.

44. Lee RK, Mottrie A, Payne CK, Waltregny D. A review of the current status of laparoscopic and robot-assisted sacrocolpopexy for pelvic organ prolapse. Eur Urol. 2014; 65:1128–1137. PMID:
24433811.

45. Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Pelvic Floor Disorders Network. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004; 104:805–823. PMID:
15458906.

46. Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014; 123:5–12. PMID:
24463657.
47. Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of posthysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013; 24:377–384. PMID:
22864764.

48. Geller EJ, Siddiqui NY, Wu JM, Visco AG. Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol. 2008; 112:1201–1206. PMID:
19037026.

49. Nosti PA, Umoh Andy U, Kane S, White DE, Harvie HS, Lowenstein L, et al. Outcomes of abdominal and minimally invasive sacrocolpopexy: a retrospective cohort study. Female Pelvic Med Reconstr Surg. 2014; 20:33–37. PMID:
24368486.
50. Paraiso MF, Jelovsek JE, Frick A, Chen CC, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011; 118:1005–1013. PMID:
21979458.
51. Siddiqui NY, Geller EJ, Visco AG. Symptomatic and anatomic 1-year outcomes after robotic and abdominal sacrocolpopexy. Am J Obstet Gynecol. 2012; 206:435.e1–435.e5. PMID:
22397900.

52. Costantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, di Biase M, et al. Laparoscopic versus abdominal sacrocolpopexy: a randomized, controlled trial. J Urol. 2016; 196:159–165. PMID:
26780167.

53. Salamon CG, Lewis C, Priestley J, Gurshumov E, Culligan PJ. Prospective study of an ultra-lightweight polypropylene Y mesh for robotic sacrocolpopexy. Int Urogynecol J. 2013; 24:1371–1375. PMID:
23296684.

54. Pan K, Zhang Y, Wang Y, Wang Y, Xu H. A systematic review and meta-analysis of conventional laparoscopic sacrocolpopexy versus robot-assisted laparoscopic sacrocolpopexy. Int J Gynaecol Obstet. 2016; 132:284–291. PMID:
26797199.

55. Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013; 24:1481–1487. PMID:
23361855.

56. Pan K, Cao L, Ryan NA, Wang Y, Xu H. Laparoscopic sacral hysteropexy versus laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. 2016; 27:93–101. PMID:
26179552.

57. Warner WB, Vora S, Hurtado EA, Welgoss JA, Horbach NS, von Pechmann WS. Effect of operative technique on mesh exposure in laparoscopic sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2012; 18:113–117. PMID:
22453322.

58. Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES. Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J. 2011; 22:205–212. PMID:
20842494.

59. Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic-assisted vaginal hysterectomy: experience of 402 patients. J Minim Invasive Gynecol. 2008; 15:188–196. PMID:
18312989.

60. Meyer I, McGwin G, Swain TA, Alvarez MD, Ellington DR, Richter HE. Synthetic graft augmentation in vaginal prolapse surgery: long-term objective and subjective outcomes. J Minim Invasive Gynecol. 2016; 23:614–621. PMID:
26922879.

61. Myers EM, Siff L, Osmundsen B, Geller E, Matthews CA. Differences in recurrent prolapse at 1 year after total vs supracervical hysterectomy and robotic sacrocolpopexy. Int Urogynecol J. 2015; 26:585–589. PMID:
25366305.
62. Gracia M, Perelló M, Bataller E, Espuña M, Parellada M, Genís D, et al. Comparison between laparoscopic sacral hysteropexy and subtotal hysterectomy plus cervicopexy in pelvic organ prolapse: a pilot study. Neurourol Urodyn. 2015; 34:654–658. PMID:
24975722.

63. Lee W, Tam J, Kobashi K. Surgery for apical vaginal prolapse after hysterectomy: abdominal sacrocolpopexy. Urol Clin North Am. 2019; 46:113–121. PMID:
30466696.
64. Oliver JL, Kim JH. Robotic sacrocolpopexy-is it the treatment of choice for advanced apical pelvic organ prolapse? Curr Urol Rep. 2017; 18:66. PMID:
28718162.

65. Majercik S, Tsikitis V, Iannitti DA. Strength of tissue attachment to mesh after ventral hernia repair with synthetic composite mesh in a porcine model. Surg Endosc. 2006; 20:1671–1674. PMID:
17001442.

66. Greenberg JA, Clark RM. Advances in suture material for obstetric and gynecologic surgery. Rev Obstet Gynecol. 2009; 2:146–158. PMID:
19826572.
67. Linder BJ, Anand M, Klingele CJ, Trabuco EC, Gebhart JB, Occhino JA. Outcomes of robotic sacrocolpopexy using only absorbable suture for mesh fixation. Female Pelvic Med Reconstr Surg. 2017; 23:13–16. PMID:
27636221.

68. Callewaert G, Bosteels J, Housmans S, Verguts J, Van Cleynenbreugel B, Van der Aa F, et al. Laparoscopic versus robotic-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review. Gynecol Surg. 2016; 13:115–123. PMID:
27226787.

69. Claerhout F, Verguts J, Werbrouck E, Veldman J, Lewi P, Deprest J. Analysis of the learning process for laparoscopic sacrocolpopexy: identification of challenging steps. Int Urogynecol J. 2014; 25:1185–1191. PMID:
24846153.

70. Mowat A, Maher C, Pelecanos A. Can the learning curve of laparoscopic sacrocolpopexy be reduced by a structured training program? Female Pelvic Med Reconstr Surg. 2018; 24:272–276. PMID:
28657989.

71. Tan-Kim J, Nager CW, Grimes CL, Luber KM, Lukacz ES, Brown HW, et al. A randomized trial of vaginal mesh attachment techniques for minimally invasive sacrocolpopexy. Int Urogynecol J. 2015; 26:649–656. PMID:
25421934.

72. Borahay MA, Oge T, Walsh TM, Patel PR, Rodriguez AM, Kilic GS. Outcomes of robotic sacrocolpopexy using barbed delayed absorbable sutures. J Minim Invasive Gynecol. 2014; 21:412–416. PMID:
24263027.

73. Kallidonis P, Al-Aown A, Vasilas M, Kyriazis I, Panagopoulos V, Fligou F, et al. Laparoscopic sacrocolpopexy using barbed sutures for mesh fixation and peritoneal closure: a safe option to reduce operational times. Urol Ann. 2017; 9:159–165. PMID:
28479768.

74. Guan X, Ma Y, Gisseman J, Kleithermes C, Liu J. Robotic single-site sacrocolpopexy using barbed suture anchoring and peritoneal tunneling technique: tips and tricks. J Minim Invasive Gynecol. 2017; 24:12–13. PMID:
27344033.

75. Liu J, Bardawil E, Zurawin RK, Wu J, Fu H, Orejuela F, et al. Robotic single-site sacrocolpopexy with retroperitoneal tunneling. JSLS. 2018; 22:e2018.00009.

76. Matanes E, Lauterbach R, Mustafa-Mikhail S, Amit A, Wiener Z, Lowenstein L. Single port robotic assisted sacrocolpopexy: our experience with the first 25 cases. Female Pelvic Med Reconstr Surg. 2017; 23:e14–e18. PMID:
28134702.

77. Lowenstein L, Matanes E, Burke YZ. Surgical technique for robot-assisted sacrocolpopexy performed via a single port. Urology. 2017; 103:272. PMID:
28982620.

78. Kim S, Pollock GR, Twiss CO, Funk JT. Surgery for posterior compartment vaginal prolapse: graft augmented repair. Urol Clin North Am. 2019; 46:87–95. PMID:
30466706.

79. Paraiso MF, Barber MD, Muir TW, Walters MD. Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol. 2006; 195:1762–1771. PMID:
17132479.

80. Mowat A, Maher D, Baessler K, Christmann-Schmid C, Haya N, Maher C. Surgery for women with posterior compartment prolapse. Cochrane Database Syst Rev. 2018; 3:CD012975. PMID:
29502352.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download