Abstract
Purpose
Chemically strong-acids (HF and HCl/H2SO4) dual etching implant surfaces have higher strengths of osseointegration than machined implant surfaces. However, the dual acid treatment deteriorates the physical properties of the titanium by weakening the fatigue resistance of the implant and causing microcracks. The removal torque comparison between the dual-acid etched (hydrochloric acid, sulfuric acid, HS) and single-acid etched implants (hydrochloric acid, H) could reveal the efficiency of implant surface acid treatment.
Materials and methods
Nine 3.75 × 4 mm dual-acid etched SLA implants and nine single-acid etched SLA implants were inserted into New Zealand rabbit tibias. After 10 days, removal torque, roughness, and wetting angle were measured.
Results
Mean removal torque values were as follows: Mean removal torque were 9.94 Ncm for HS group and 9.96 Ncm for H group (P=.995). Mean surface roughness value were 0.93 µm for HS group and 0.84 µm for H group (P=.170). Root mean square roughness (RSq) values were 1.21 µm for HS group and 1.08 µm for H group (P=.294), and mean wetting angle values were 99° for HS group and 98° for H group (P=.829). Statistical analysis showed no significant difference between the removal torques, roughness, or wetting angles of the two groups.
The relationship between dental implants and bone was developed based on the concept of osseointegration of titanium, as claimed by Brånemark.1 The high success rate of implants and good long-term prognosis are influenced by patient factors and the condition of the implant.23 Patient factors were not the topic of this study; the study focused instead on the conditions of the implants.
Implant conditions include physical properties, surface treatments, corrosion resistance, abrasion resistance, and others. The condition of the implant surface that directly integrates with the bone is an essential factor.45 This implant condition is actively studied to enlarge the contact area between the bone and the implant and to increase the removal torque using surface treatments.678910111213141516171819202122
Acid treatment methods using hydrochloric, sulfuric, and hydrofluoric acids have been introduced, which produce micropits with a diameter of 0.5 – 2.0 µm on the implant surface.1516 These acid-treated surfaces increase the apposition of bone on the implant surface by enhancing the osteogenic mechanism through the attachment of fibrin and osteoblasts.23 Studies have determined that the implant surface treated with blasting and acid etching (SLA) results in a high BIC, high osseointegration strength, and high clinical success rates.616171819202122
The acid treatment used for Straumann SLA implants is the dual-acid etching method, which mixes high-concentration hydrochloric and sulfuric acids at a temperature above 100℃, and Osseotite is in implants made using hydrofluoric, hydrochloric, and sulfuric acids. Other acid etching methods used depend upon the manufacturer. The treatment coats the implant surface with 20 – 40% titanium hydride (TiH); Straumann SLA implants consist of 37% TiH and 63% TiH.
However, the acid treatment deteriorates the mechanical properties of the titanium by weakening the fatigue resistance of the implant. Titanium hydride needles that were known as hydrogen embrittlement of titanium may be triggered by TiH. Stronger acid treatments increase surface roughness, but also increase the concentration of TiH resulting in weaker mechanical properties and increased possibility of fracture.2425
Surface wettability and roughness are also important physical properties of surface-treated implants that affect implant osseointegration. The adhesion and spread of cells on the bioconjugate material depends on the wettability of the material. Surface roughness affects wettability.262728 At the early stage of implantation, cell attachment is affected by physicochemical properties including wettability. Therefore, the degree of wettability affects the initial stage of osseointegration of implants.
The dual-acid etching method is preferentially used for currently existing products. The treatment increases surface roughness at a microscopic level. It also causes various problems compared to the single-acid method, such as decreased mechanical properties of the implant and environmental pollution.
In this study, we compared the removal torque, roughness and wettability of two groups of integrating implants manufactured using dual-acid etching (hydrochloric acid, sulfuric acid) as the control group and single-acid etching (hydrochloric acid) as the experimental group.
A total of 9 SLA implants (CSM Implant Co., Ltd., Daegu, Korea) manufactured using dual-acid etching with hydrochloric and sulfuric acids (HS group) and 9 SLA implants (CSM Implant Co., Ltd., Korea) manufactured using single-acid etching with hydrochloric acid (H group) were studied. The implants were 3.75 mm in diameter and 4 mm in length.
This experiment was approved by the Animal Care and Use Committee of Kyung-Pook National University. A total of 9 New Zealand rabbits with an average weight of 3.5 kg were included in the study. The rabbits were anesthetized intramuscularly with 0.2 mL/kg of tiletamine/zolazepam (Zolet, Virbac Laboratories, France) and 0.25 mL/kg of xylazine (Rompun, Bayer Korea, Korea).
After removing the hair from the intended surgical site, the site was pre-treated with iodine and a 75% ethanol hybrid solution before incision. After the tibia was exposed, the implants were placed according to the manufacturer's surgical guide. 9 implants surface-treated with hydrochloric acid and sulfuric acid was inserted in the tibia under constant irrigation of physiological saline solution, and 9 implants surface-treated with hydrochloric acid was placed in the tibia. After implantation, the incision was closed with 4-0 Vicryl and 3-0 silk.
After the surgical procedure, antibiotics and medications were administered and appropriate management was performed. After 10 days, this period may be regarded as the early stage of the healing period, presuming that 10 days in a rabbit is equivalent to approximately 25 days in a human.29 anesthesia was performed as described above and the surgical site was re-opened. After the implant was exposed, the removal torque (MGT-12 digital torque gauge, Mark-10 Corp, New York, NY, USA) was measured and the rabbits were sacrificed.
Roughness was measured in average surface roughness (RSa) and mean root square of the surface (RSq) using confocal laser scanning microscopy (Carl Zeiss, LSM 700, Oberkochen, Germany). A total of 3 specimens were measured at 3 middle point of implant.
Plates 10 mm square were made using the same material as the implants and received the same acid treatment. The wetting angle was measured by CA goniometer (SmartDrop, Femtobiomed Inc., Korea) using distilled water.
The two group were compared through t-test in statistical analysis.
The average removal torque was 9.94 Ncm in HS group and 9.96 Ncm in H group (Table 1). The surface roughness of HS group was 0.93 µm in RSa, 1.21 µm in RSq and H group was 0.84 µm in RSa, 1.08 µm in RSq (Table 2). The wetting angle was 99° in HS group and 98° in H group (Table 3). Statistical analysis revealed no difference in removal torque, roughness, or wetting angle between the two groups (Table 4).
The removal torque test is used to measure the extent of osseointegration of the implant. The first use was in 1988 by Carlsson et al., and measured the sheer force of the machined-screw implant required to cause a fracture between un-integrated and integrated bone.30 Removal torque is not obtained by a break between the bone and the implant, but by a rupture between un-integrated and integrated bone. Thus, the measurement of removal torque detects the degree of osseointegration of the implant, and the removal torque varies depending on the surface roughness and the time of measurement. The timing at which the surface roughness of the test material affects osseointegration changes during osseointegration, so the timing of the measurement of the removal torque should be adjusted according to surface roughness.
Rapid bone attachment after implant placement is an important factor in the success of the implant. In clinical practice, the removal torque value (RTV) was approximately 140 Ncm in 4 weeks after insertion of acid-treated implants.31 Based on this, there have been studies of the 99% success rate of implants over 3 years in a clinical trial of prostheses 6 weeks after implantation.2232 The results of these studies suggested that the initial bone attachment after implant placement had a significant impact on the implant success rate.
In a rabbit, the removal torque changes significantly until 1 month after placement of the implant, but there is little or no change after 1 month.16 The removal torque after 1 month of implantation ranges from 20 to 30 Ncm.1630 In addition, a study by Albrektsson et al. compared the healing time of rabbits with that of humans and concluded that 6 weeks of rabbit healing was equivalent to 3 – 4 months of human healing.29 This period may be regarded as the early stage of the healing period, presuming that 10 days in a rabbit is equivalent to approximately 25 days in a human. The average removal torque after 10 days was approximately 10 Ncm in this experiment. In comparison with the removal torque after 1 month, this degree shows a fairly high removal torque during a normal healing process. Therefore, the surface of the implant with a micro-texture due to acid treatments seems to affect osseointegration at the early stage of implantation. As there was no difference between the mean values of the experimental and control groups, the results of the dual-acid etching method using hydrochloric acid and sulfuric acid and the single-acid etching method using only hydrochloric acid were not significantly different.
The surface roughness of implants in this experiment ranged from 0.5 to 2 µm, which generally results from acid surface treatments. Implants with this range of roughness promote early osseointegration.16 Thus, the roughness of an implant affects the relationship between surface energy and cell proliferation.33
According to Wennerberg et al.,34 a histological experiment using 5 µm, 75 µm, and 250 µm particle blasted implants showed that 250 µm implants have the highest BIC. Another study reported that plasma spray methods or coating methods lead to increased roughness but decreased BIC, removal torque, and osseointegration strength compared to implants treated with blasting or acid.6
Webb et al.35 demonstrated that cell differentiation is affected by surface roughness. Cells grown on rough surfaces produce more osteocalcin and alkaline phosphatase, suggesting that these mechanisms are the result of the differentiation and proliferation of osteoblasts.
During the healing process after implantation, cells migrate toward and adhere to the surface of the implant to formulate bone, which results in osseointegration of the implant into the bone. Cells require a certain roughness to move rapidly and adhere to the implant surface. Thus, not just high but suitable roughness is important. The acid treatment is an essential factor for the preparation of implants with rough surfaces, but there was no difference in roughness between the control and the experimental groups in this experiment. Thus, the dual-acid and single-acid etching methods were not different. Dualacid etching cannot be considered superior to single-acid etching, as there was no difference between the experimental and control groups and the ideal roughness has not yet been determined.
Physical properties of the surface and surface energy can be measured using the wettability and contact angle between the surface and the liquid. These values indicate whether a surface is hydrophilic or hydrophobic. Surfaces with contact angle close to 0° are hydrophilic, while those with contact angle close to 140° are hydrophobic.
The average contact angles of the experimental and control groups were 98° and 99°, respectively, suggesting no difference. Therefore, the contact angle, or wettability, did not appear to differ according to single-acid or dual-acid etching. These results suggest that both experimental and control implants are more hydrophobic than hydrophilic.
The higher hydrophilicity encourages cell and tissue interaction.36 Proteins on the surface of implants are highly influenced by surface properties in their absorption and adhesion. Therefore, the degree of hydrophilicity of the implant surface affects initial osseointegration.
Surface properties such as roughness, wettability, and surface energy affect the cells involved in early osseointegration. Studies by Boyan et al.37 have shown that higher wettability increases cell differentiation, and that more fibroblasts attach to a hydrophilic surface than to a hydrophobic surface. These hydrophilic implant surfaces enhance adhesion of fibrin to the surface, and the attached fibrin induces the attachment of osteoblasts. The attachment mechanism of cells to the implant surface affects the differentiation of cells and the formation of surrounding tissues.
Chemical acid treatments weaken the physical properties of titanium. These treatments produce microcracks that weaken the fatigue resistance of the implant. The effect is due to hydrogen ions (H+) generated during the acid treatment of the implant surface that rapidly penetrate the surface and accumulate underneath. These ions produce the titanium hydride layer.3839 Titanium hydride can be up to 40% of the implant. This high concentration of titanium hydrides triggers a hydride needle, which weakens fatigue resistance. This is known as hydrogen embrittlement of titanium.2540 SLAactive is manufactured with dual-acid etching and includes 37% titanium hydride.24 This titanium hydride weakens the implant, which decreases the prognosis of the implant over time.
However, according to a study of sandblasted and acid-etched implants by Zhang et al.,41 the experimental group containing TiH showed increased alkaline phosphatase and osteocalcin. The study determined that TiH is eliminated by heat treatment. In addition, cell differentiation and cell adhesion were significantly higher in the TiH group, suggesting that TiH improves osseointegration by affecting cells and surrounding tissues during the early stage of osseointegration.
As there are a number of methods that do not use blasting or acid-etching surface treatments, and implants treated with those methods also show good osseointegration,7911 the use of blasting and strong, dual, triple etching should be reconsidered.
TiH, which is produced at high concentrations by these acid treatments, ultimately weakens the implant. In addition, more acid treatments increase the industrial pollution generated by the treatments, and damage the environment. In this experiment using implants treated by the dual-acid and single-acid etching methods in rabbits, we found that there is no significant difference in the removal torques, roughness, or contact angles between the two types of treated implants. So we expect that implant surface treatment should be not by stronger acid etching and more surface roughness, but by making ideal surface roughness through study and researches.
Figures and Tables
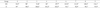
Table 1
Removal torque of HS group and H group. The average removal torque was 9.94 Ncm in HS group and 9.96 Ncm in H group (Unit: Ncm)

Table 2
Surface roughness of HS group and H group. The surface roughness of HS group was 0.93 µm in RSa, 1.21 µm in RSq and H group was 0.84 µm in RSa, 1.08 µm in RSq (Unit: µm)

References
1. Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969; 3:81–100.
2. van Steenberghe D, Jacobs R, Desnyder M, Maffei G, Quirynen M. The relative impact of local and endogenous patientrelated factors on implant failure up to the abutment stage. Clin Oral Implants Res. 2002; 13:617–622.

3. Wennerberg A, Hallgren C, Johansson C, Danelli S. A histomorphometric evaluation of screw-shaped implants each prepared with two surface roughnesses. Clin Oral Implants Res. 1998; 9:11–19.

4. Vervaeke S, Collaert B, De Bruyn H. The effect of implant surface modifications on survival and bone loss of immediately loaded implants in the edentulous mandible. Int J Oral Maxillofac Implants. 2013; 28:1352–1357.

5. Souza FA, Queiroz TP, Guastaldi AC, Garcia-Júnior IR, Magro-Filho O, Nishioka RS, Sisti KE, Sonoda CK. Comparative in vivo study of commercially pure Ti implants with surfaces modified by laser with and without silicate deposition: biomechanical and scanning electron microscopy analysis. J Biomed Mater Res B Appl Biomater. 2013; 101:76–84.
6. Buser D, Schenk RK, Steinemann S, Fiorellini JP, Fox CH, Stich H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J Biomed Mater Res. 1991; 25:889–902.

7. Daculsi G, Laboux O, Malard O, Weiss P. Current state of the art of biphasic calcium phosphate bioceramics. J Mater Sci Mater Med. 2003; 14:195–200.
8. Geurs NC, Jeffcoat RL, McGlumphy EA, Reddy MS, Jeffcoat MK. Influence of implant geometry and surface characteristics on progressive osseointegration. Int J Oral Maxillofac Implants. 2002; 17:811–815.
9. Chang YL, Lew D, Park JB, Keller JC. Biomechanical and morphometric analysis of hydroxyapatite-coated implants with varying crystallinity. J Oral Maxillofac Surg. 1999; 57:1096–1108.

10. Hallgren C, Reimers H, Chakarov D, Gold J, Wennerberg A. An in vivo study of bone response to implants topographically modified by laser micromachining. Biomaterials. 2003; 24:701–710.

11. Cho SA, Jung SK. A removal torque of the laser-treated titanium implants in rabbit tibia. Biomaterials. 2003; 24:4859–4863.

12. Gaggl A, Schultes G, Müller WD, Kärcher H. Scanning electron microscopical analysis of laser-treated titanium implant surfaces-a comparative study. Biomaterials. 2000; 21:1067–1073.

13. Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995; 6:24–30.

14. Ivanoff CJ, Hallgren C, Widmark G, Sennerby L, Wennerberg A. Histologic evaluation of the bone integration of TiO(2) blasted and turned titanium microimplants in humans. Clin Oral Implants Res. 2001; 12:128–134.

15. Massaro C, Rotolo P, De Riccardis F, Milella E, Napoli A, Wieland M, Textor M, Spencer ND, Brunette DM. Comparative investigation of the surface properties of commercial titanium dental implants. Part I: chemical composition. J Mater Sci Mater Med. 2002; 13:535–548.
16. Klokkevold PR, Johnson P, Dadgostari S, Caputo A, Davies JE, Nishimura RD. Early endosseous integration enhanced by dual acid etching of titanium: a torque removal study in the rabbit. Clin Oral Implants Res. 2001; 12:350–357.

17. Cho SA, Park KT. The removal torque of titanium screw inserted in rabbit tibia treated by dual acid etching. Biomaterials. 2003; 24:3611–3617.

18. Trisi P, Marcato C, Todisco M. Bone-to-implant apposition with machined and MTX microtextured implant surfaces in human sinus grafts. Int J Periodontics Restorative Dent. 2003; 23:427–437.
19. He FM, Yang GL, Zhao SF, Cheng ZP. Mechanical and histomorphometric evaluations of rough titanium implants treated with hydrofluoric acid/nitric acid solution in rabbit tibia. Int J Oral Maxillofac Implants. 2011; 26:115–122.
20. Zareidoost A, Yousefpour M, Ghaseme B, Amanzadeh A. The relationship of surface roughness and cell response of chemical surface modification of titanium. J Mater Sci Mater Med. 2012; 23:1479–1488.

21. Roccuzzo M, Bunino M, Prioglio F, Bianchi SD. Early loading of sandblasted and acid-etched (SLA) implants: a prospective split-mouth comparative study. Clin Oral Implants Res. 2001; 12:572–578.

22. Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, Peters F, Simpson JP. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002; 13:144–153.

23. Park JY, Davies JE. Red blood cell and platelet interactions with titanium implant surfaces. Clin Oral Implants Res. 2000; 11:530–539.

24. Szmukler-Moncler S, Bischof M, Nedir R, Ermrich M. Titanium hydride and hydrogen concentration in acid-etched commercially pure titanium and titanium alloy implants: a comparative analysis of five implant systems. Clin Oral Implants Res. 2010; 21:944–950.

25. Yokoyama K, Ichikawa T, Murakami H, Miyamoto Y, Asaoka K. Fracture mechanisms of retrieved titanium screw thread in dental implant. Biomaterials. 2002; 23:2459–2465.

26. van Kooten TG, Schakenraad JM, van der Mei HC, Busscher HJ. Influence of substratum wettability on the strength of adhesion of human fibroblasts. Biomaterials. 1992; 13:897–904.

27. Yanagisawa I, Sakuma H, Shimura M, Wakamatsu Y, Yanagisawa S, Sairenji E. Effects of “wettability” of biomaterials on culture cells. J Oral Implantol. 1989; 15:168–177.
28. Kilpadi DV, Lemons JE. Surface energy characterization of unalloyed titanium implants. J Biomed Mater Res. 1994; 28:1419–1425.

29. Albrektsson T, Brånemark PI, Eriksson A, Lindström J. The preformed autologous bone graft. An experimental study in the rabbit. Scand J Plast Reconstr Surg. 1978; 12:215–223.

30. Carlsson L, Röstlund T, Albrektsson B, Albrektsson T. Removal torques for polished and rough titanium implants. Int J Oral Maxillofac Implants. 1988; 3:21–24.
31. Buser D, Nydegger T, Oxland T, Cochran DL, Schenk RK, Hirt HP, Snétivy D, Nolte LP. Interface shear strength of titanium implants with a sandblasted and acid-etched surface: a biomechanical study in the maxilla of miniature pigs. J Biomed Mater Res. 1999; 45:75–83.

32. Roccuzzo M, Wilson T. A prospective study evaluating a protocol for 6 weeks’ loading of SLA implants in the posterior maxilla: one year results. Clin Oral Implants Res. 2002; 13:502–507.

33. Ponsonnet L, Reybier K, Jaffrezic N, Comte V, Lagneau C, Lissac M, Martelet C. Relationship between surface properties (roughness, wettability) of titanium and titanium alloys and cell behaviour. Mater Sci Eng C. 2003; 23:551–560.

34. Wennerberg A, Albrektsson T, Andersson B. Bone tissue response to commercially pure titanium implants blasted with fine and coarse particles of aluminum oxide. Int J Oral Maxillofac Implants. 1996; 11:38–45.
35. Webb K, Hlady V, Tresco PA. Relative importance of surface wettability and charged functional groups on NIH 3T3 fibroblast attachment, spreading, and cytoskeletal organization. J Biomed Mater Res. 1998; 41:422–430.

36. Zhao G, Schwartz Z, Wieland M, Rupp F, Geis-Gerstorfer J, Cochran DL, Boyan BD. High surface energy enhances cell response to titanium substrate microstructure. J Biomed Mater Res A. 2005; 74:49–58.

37. Boyan BD, Dean DD, Lohmann CH, Cochran DL, Sylvia VL, Schwartz Z. The titanium-bone cell interface in vitro: The role of the surface in promoting osteointegration. In : Donald MB, Pentti T, Marcus T, editors. Titanium in medicine. Berlin, Heidelberg: Springer;2001. p. 561–585.
38. Szmukler-Moncler S, Reingewirtz Y, Weber H-P. Bone response to early loading: The effect of surface state. In : Davidovitch Z, Norton LA, editors. Biological mechanisms of tooth movement and craniofacial adaptation. Boston: Harvard Society for the Advancement of Orthodontics;1996. p. 611–616.
39. Taborelli M, Jobin M, François P, Vaudaux P, Tonetti M, Szmukler-Moncler S, Simpson JP, Descouts P. Influence of surface treatments developed for oral implants on the physical and biological properties of titanium. (I) Surface characterization. Clin Oral Implants Res. 1997; 8:208–216.

40. Donachie Junior MJ. Titanium: A technical guide. 2nd ed. Materials Park: ASM International;2000. p. 85–94.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download