Abstract
Intramuscular hematomas on the psoas muscle are rare and usually occur as a result of trauma, iatrogenic etiology during lumbar surgery, rupture of the aortic aneurysm, and hematologic diseases. The incidence of spontaneous psoas muscle hematomas has slowly increased as a result of using anticoagulation and antiplatelet agents. Magnetic resonance (MR) imaging is a more sensitive option compared to computed tomography (CT) when diagnosing a hematoma. Coronal T2-weighted images are more useful. CT imaging is also useful to establish the rapid diagnosis of hematoma. When a prolonged prothrombin time and international normalized ratio and decrease platelet count are noted, psoas muscle hematomas should be considered, if there was no lesion in the spinal canal. Most hematomas resolve spontaneously without clinical complications if the hematoma is not large or it is not compressing the surrounding important structures, irrespective of cause.
Go to : 
Hematomas on the psoas muscle occur secondary to trauma, iatrogenic etiology during lumbar surgery including endoscopic discectomy,56) use of anticoagulants, or coagulation disorders such as disseminated intravascular coagulation and hemophilia. Hematomas of the psoas muscle are rare with an occurrence of 0.1% to 0.6% and being elderly and undergoing hemodialysis are also risk factors.12) Bilateral psoas muscle hematomas may be rarer than unilateral hematomas. Iliopsoas hematomas generally present with groin or thigh pain, muscle dysfunction, numbness or paresthesia of the unilateral lower extremity, and occasionally nerve palsy with the femoral nerve most commonly affected.3) Motor weakness may occur in chronic and large hematomas. Ecchymosis in the periumbilical area (Cullen's sign) or in the flanks (Grey-Turner's sign) may occur. Intramuscular hematomas are diagnosed by computed tomography (CT) and magnetic resonance (MR) imaging. Most hematomas resolve spontaneously without clinical complications, if the hematoma is not large, or it is not compressing the surrounding important structures. Moreover, some hematomas gradually grow for months and years.
Go to : 
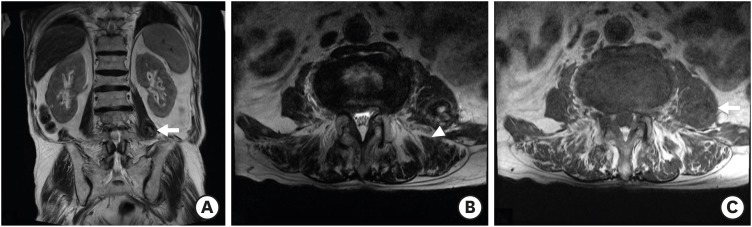
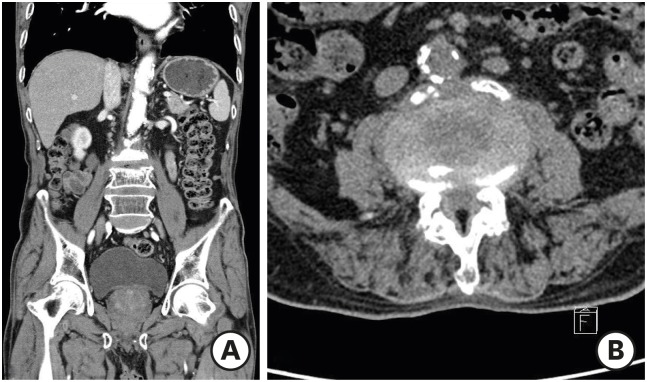
An 81-year-old man was admitted to our emergency room with complaints of back and buttock pain. The symptoms were developed 2 days previously after a heavy weight lifting injury. He had a history of iron deficiency anemia and anticoagulant medication. Motor weakness of the lower extremities was not observed. Urinary and bowel incontinence was also not noted. Platelet count was within normal range and prothrombin time (PT) and international normalized ratio (INR) were prolonged in initial laboratory findings. The platelet count was 220,000/mm3(140,000–400,000/mm3), the PT was 19.6 sec (10.4–12.8 seconds), and the INR was 1.77 (0.93–1.14). An acute compression fracture was not noted on plain radiograph. An approximately 2.8-cm-sized oval-shaped mass with heterogeneous signal intensity was noted in the left psoas muscle (FIGURE 1). The mass had iso to high signal intensity (SI) on T2 weighted image (WI) and isointense SI on T1 WI. We radiologically diagnosed the lesion as a hematoma, and the hematoma was treated conservatively because of the absence of neurologic deficits accompanied with the hematoma. The pain was gradually relieved. Three weeks later, follow-up CT imaging was performed. The hematoma was nearly-totally absorbed (FIGURE 2). Hence, the patient was discharged without any symptoms.
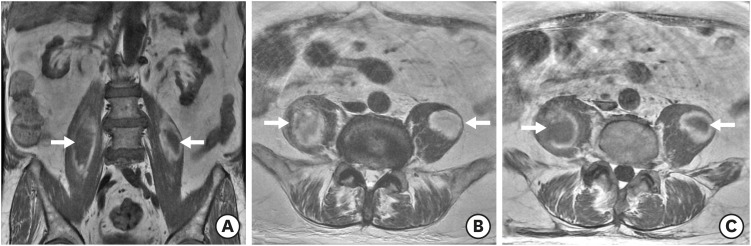
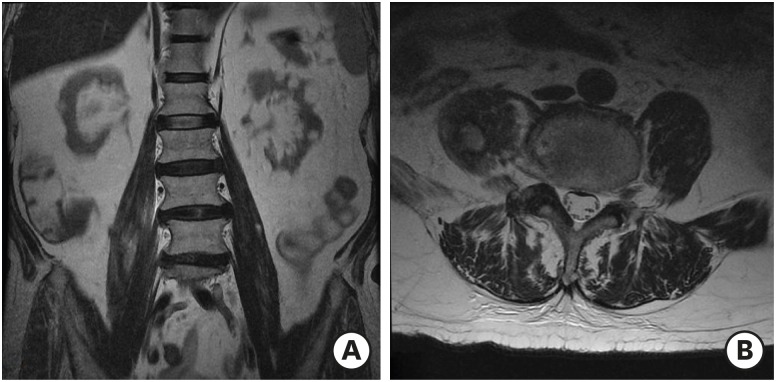
An 81-year-old man was referred to our department from the department of nephrology with a complaint of gradually developing pain in both lower extremities (right side dominant) several days ago. The patient was admitted to our hospital with poor oral feeding, azotemia, and acute renal failure 3 weeks ago. He had no recent trauma history. He had no previous history of antiplatelet and/or anticoagulant medication, but he had chronic kidney disease. According to the initial laboratory findings, the platelet count was decreased (126.000/mm3), but, the INR (1.08) and PT (12.3 seconds) were not increased. INR and PT prolongation was not noted during his hospital stay. Motor weakness was not observed. A well-demarcated mass lesion was noted on both psoas muscles during MR imaging (FIGURE 3). Heterogeneous intermediate to low SI and peripheral high SI rim on T1 and T2 WI was observed. We treated the mass conservatively, and the pain was slowly relieved. Four weeks later, the hematoma size decreased on MR imaging (FIGURE 4).
Go to : 
Intramuscular hematomas on the psoas muscle usually occur as a result of trauma and underlying hematologic diseases. Coagulation disorders result in acute bleeding influenced by fibrinolysis.2) Iatrogenically occurring hematomas may occur as a result of the compression of the nerve roots after lumbar surgery.1113) The minor trauma on the psoas muscle during screw insertion may be related to the occurrence of hematoma.
However, lesions of the psoas muscle may also present with non-specific or slowly progressing symptoms because of its retrofascial location.4) The iliopsoas forms part of the posterior abdominal wall lying posteriorly in the retroperitoneum. The differentiations of the psoas lesions are difficult to assess radiologically. It is significantly more difficult to distinguish other lesions in chronic hematomas compared to acute hematomas. The hematomas on the psoas muscle will gradually develop into large hematomas because of the presence of thin psoas fascia.11)
Performing MR imaging is more sensitive compared to CT imaging when diagnosing a hematoma. Coronal T2-weighted images are more useful.10) Moreover, it is more difficult to distinguish a neoplasm and an abscess compared to hematoma when performing CT imaging. The hematoma diffusely involves the muscle compared to the neoplasm and abscess.9) A mosaic of various signal intensities, named the “mosaic sign,” is useful in diagnosing hematoma on MR T2-weighted imaging.1) The mosaic sign reflects repeated hemorrhage and absorption, and it tends to appear in chronic expanding hematomas.1)
However, sonography and CT imaging are also useful to establish the rapid diagnosis of hematoma. CT images of hematomas show diffuse involvement of the muscles, and a hyperdense lesion in the muscle may be the early sign of hematoma.9) CT imaging is helpful in evaluating the extent of hematoma in relation to its adjacent structures and in identifying the regression of hematoma.4) If air bubbles with calcification are noted within the hematoma, CT imaging is also preferred.7)
Definitive treatment of iliopsoas hematoma is not well-established. It may be reasonable to consider the following in choosing the method of treatment for hematoma: speed of onset, timing of diagnosis, hematoma volume, cause of hematoma, and degree of neurological impairment.310)
Most hematomas resolve spontaneously without clinical complications. However, large hematomas or those hematomas involving the iliacus muscle may compress the femoral nerve. Sometimes, surgical resection of the hematoma is required.8) Drainage of the hematoma during CT-guided imaging is also useful.13) The surgical resection of the hematoma is also required to rule out intratumoral hematoma.14)
Go to : 
When the prolonged PT and INR and decreases in platelet count were noted, psoas muscle hematomas should be considered if there is no lesion in the spinal canal. MR imaging is the diagnostic method of choice when distinguishing other lesions on the psoas muscle. However, MR imaging can provide difficulties, including high costs, and if there are medical devices or metallic foreign materials in the body, CT is also useful diagnostic tool as a screening test.
Hematomas resolve spontaneously without clinical complications, if the hematoma is not large, or it is not compressing the surrounding important structures, whether a traumatic or spontaneous occurrence.
Go to : 
References
1. Akata S, Ohkubo Y, Jinho P, Saito K, Yamagishi T, Yoshimura M, et al. MR features of a case of chronic expanding hematoma. Clin Imaging. 2000; 24:44–46. PMID: 11120417.

2. Almushayti Z. Hematoma of the psoas muscle, in prostatic cancer patient: a case report. Pan Afr Med J. 2015; 20:138. PMID: 27386016.

3. Basheer A, Jain R, Anton T, Rock J. Bilateral iliopsoas hematoma: case report and literature review. Surg Neurol Int. 2013; 4:121. PMID: 24232386.

4. Cronin CG, Lohan DG, Meehan CP, Delappe E, McLoughlin R, O'Sullivan GJ, et al. Anatomy, pathology, imaging and intervention of the iliopsoas muscle revisited. Emerg Radiol. 2008; 15:295–310. PMID: 18548299.

5. Kim HS, Ju CI, Kim SW, Kim JG. Huge psoas muscle hematoma due to lumbar segmental vessel injury following percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2009; 45:192–195. PMID: 19352485.

6. Lakkol S, Sarda P, Karpe P, Krishna M. Conservative management of psoas haematoma following complex lumbar surgery. Indian J Orthop. 2014; 48:107–110. PMID: 24600073.

7. Lee JK, Glazer HS. Psoas muscle disorders: MR imaging. Radiology. 1986; 160:683–687. PMID: 3737906.

8. Lefevre N, Bohu Y, Klouche S, Chemla N, Herman S. Complete paralysis of the quadriceps secondary to post-traumatic iliopsoas hematoma: a systematic review. Eur J Orthop Surg Traumatol. 2015; 25:39–43. PMID: 23996110.

9. Lenchik L, Dovgan DJ, Kier R. CT of the iliopsoas compartment: value in differentiating tumor, abscess, and hematoma. AJR Am J Roentgenol. 1994; 162:83–86. PMID: 8273696.

10. Marquardt G, Barduzal Angles S, Leheta F, Seifert V. Spontaneous haematoma of the iliac psoas muscle: a case report and review of the literature. Arch Orthop Trauma Surg. 2002; 122:109–111. PMID: 11880914.
11. Robinson DE, Ball KE, Webb PJ. Iliopsoas hematoma with femoral neuropathy presenting a diagnostic dilemma after spinal decompression. Spine. 2001; 26:E135–E138. PMID: 11246396.

12. Saad Z, Ahmed B, Mostafa R, Hicham B, Lahcen B. Conservative treatment of a psoas hematoma revealed by a lower limb palsy. Pan Afr Med J. 2017; 28:138. PMID: 29541288.

13. Sarwat AM, Sutcliffe JC. Haematoma of the psoas muscle after posterior spinal instrumentation and enoxaparin prophylaxis. Grand Rounds. 2003; 3:35–37.
14. Yamasaki T, Shirahase T, Hashimura T. Chronic expanding hematoma in the psoas muscle. Int J Urol. 2005; 12:1063–1065. PMID: 16409613.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download