INTRODUCTION
A Morel-Lavallée lesion, first reported by French surgeon Victor-Auguste-Francois Morel-Lavallée in 1853, is a posttraumatic, closed internal degloving injury.
12) This uncommon lesion is caused by a shearing force abruptly separating the skin and superficial fascia from the deep fascia and creating a potential space. Blood, lymphatic fluid, and debris collect and fill the space.
1718) The most commonly affected sites are the thigh, knee, hip, and pelvic area, but the lesion can also occur in other areas, such as the lower leg, abdomen, periscapular region, and lumbosacral region.
3) The treatment method depends on size, duration, location, associated injuries, and presence of a capsule. A small acute lesion without a capsule can be treated conservatively with tight compression. However, in large chronic cases, more invasive procedures such as percutaneous drainage, sclerotherapy, or surgical resection may be required. We describe an unusual case of a Morel-Lavallée lesion in the sacrococcygeal area, an uncommon location, with an associated coccygeal fracture.
CASE REPORT
A 73-year-old woman with a history of hypertension was transferred to our institute due to a recurrent, fluctuant, soft tissue mass with moderate pain in her sacrococcygeal area. Four months prior, she had undergone L3–4 microscopic discectomy and L4–5 decompressive laminectomy for lumbar disc herniation and spinal stenosis at a local clinic, with no apparent dural tear during the operation or surgical site infection. Outpatient clinic follow-up for 1 month after discharge was unremarkable; however, she slipped and fell on her buttocks 3 months before hospitalization. There was no visible damage to her skin, but coccygeal fracture and dislocation were confirmed on performing a radiologic examination for persistent pain (
FIGURE 1). Four weeks later, she was admitted to a local clinic complaining of a soft mass with slight pain in her sacrococcygeal area. Approximately 40 mL of serosanguinous fluid was found on needle aspiration. She returned to the clinic 2 weeks later with the same symptoms, and needle aspiration was repeated. However, a large, fluctuant, painful soft mass promptly recurred, and she was transferred to our institute.
FIGURE 1
Lateral radiograph of the sacrococcygeal area shows fracture and dislocation of the coccyx (red arrow).

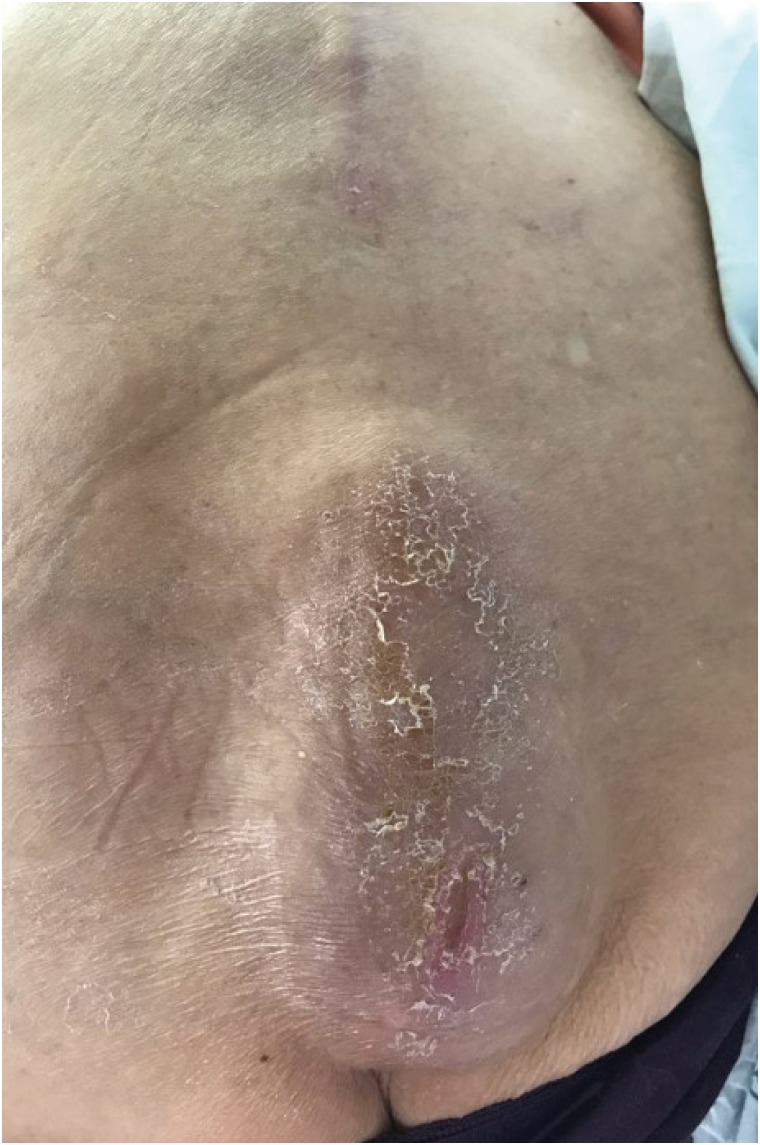
On hospitalization, the pain level was 4/10 on the visual analog scale and was unaffected by movement. A soft fluctuant mass was found in the sacrococcygeal area, but tenderness was not prominent (
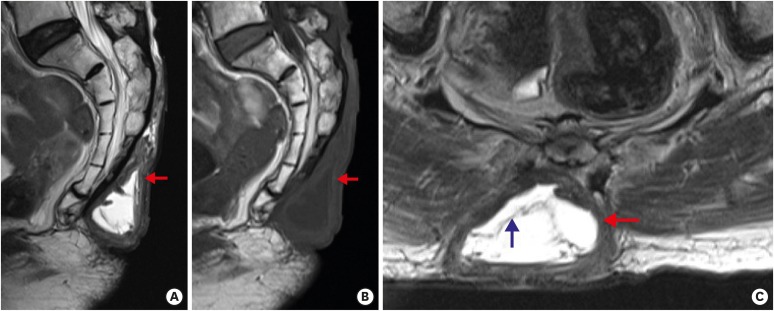
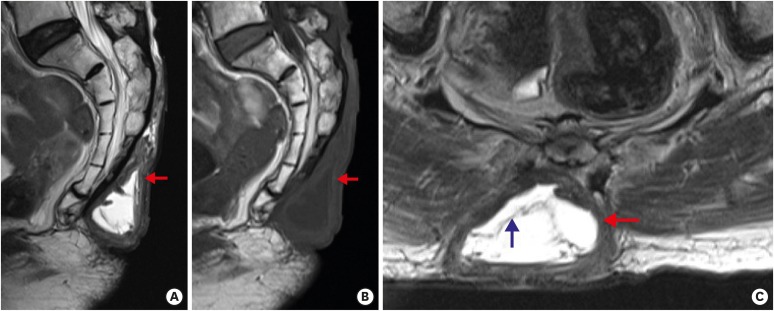
FIGURE 2). Lumbosacral magnetic resonance imaging (MRI) showed a fluid collection between the deep fascia and hypodermis, with homogeneous hypointensity on T1-weighted images (WI), hyperintensity on T2-WI, and internal septations; the lesion was surrounded by a thick peripheral capsule with hypointensity on T1-WI and T2-WI (
FIGURE 3). Needle aspiration and culture were performed, and about 50 cc of serous fluid was collected. The fluid showed a white blood cell (WBC) count of 2 cells/mm
3, red blood cell count of 300 cells/mm
3, glucose level of 60 mg/dL, and protein level of 92 mg/dL; no bacteria were found in the culture. Routine blood tests were normal, including the WBC count, erythrocyte sedimentation rate, and C-reactive protein level.
FIGURE 2
Photograph shows an extensive swelling lesion at the midline of the sacrococcygeal area.
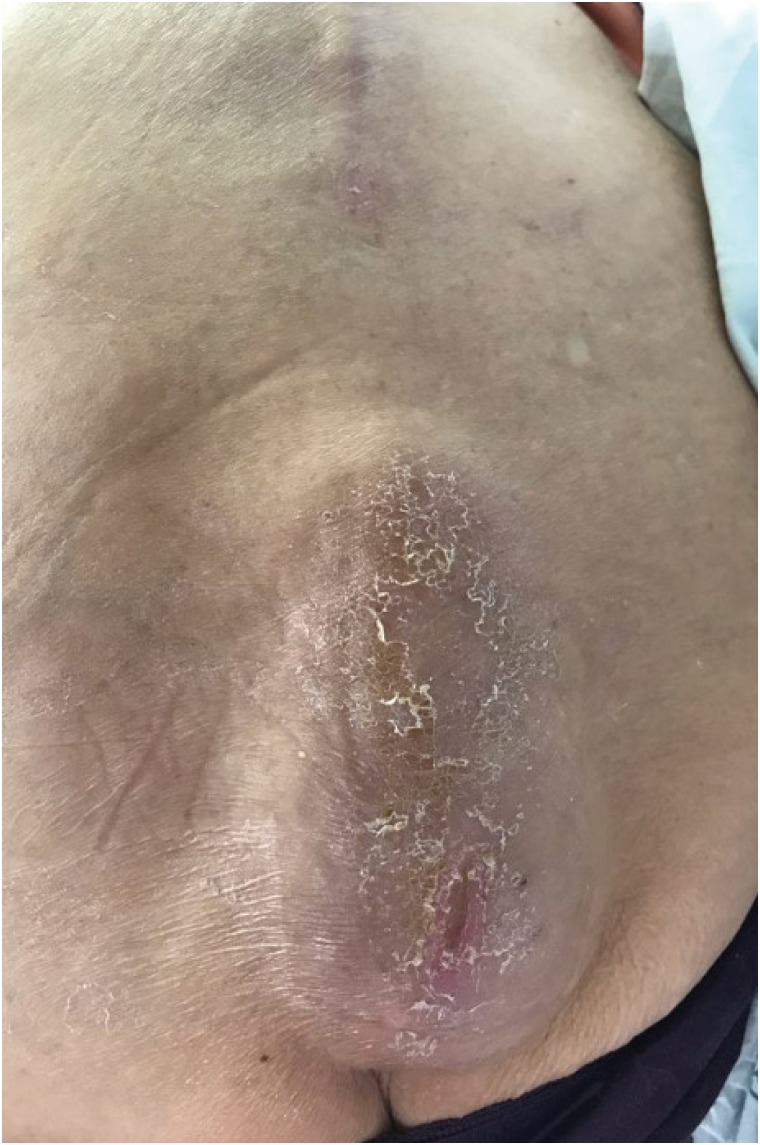
FIGURE 3
Magnetic resonance imaging of the lesion. Sagittal T2-weighted (A), sagittal T1-weighted (B), and axial T2-weighted (C) images demonstrate a fluid collection above the deep fascia, with high signal intensity on T2-weighted images and low signal intensity on T1-weighted images in the sacrococcygeal area. There is a hypointense thick peripheral capsule (red arrow) with internal septations (blue arrow).
Although the location was uncommon, we considered a Morel-Lavallée lesion. However, we could not rule out an association with previous lumbar surgery, such as cerebrospinal fluid (CSF) leakage caused by dural injury, and performed elective surgery, collaborated with the department of plastic and reconstructive surgery. The skin was incised under general anesthesia, and serous fluid flowed out. A wide and thick fibrous capsule was found above the deep fascia and was completely removed after confirmation that it was not connected to the previous lumbar surgical site. After irrigation, a drainage tube was inserted and the wound was closed tightly (
FIGURE 4). The patient was discharged without any surgery-related complications or recurrent fluid collection. We obtained informed consent from the patient.
FIGURE 4
Postoperative photograph immediately after removal of the fluctuant mass and closure of wound with a flap. A suction drainage tube is seen in the left gluteal area.

DISCUSSION
A Morel-Lavallée lesion is an uncommon closed, posttraumatic degloving injury. The lesion is caused by shearing force generated during trauma, which separates the skin and superficial fascia from the deep fascia, creating a potential space without surface penetration. Blood, lymphatic fluid, and debris collect and fill the space.
1718)
A Morel-Lavallée lesion most commonly occurs in the trochanteric region and proximal lateral thigh, but can be found anywhere in the body.
19) Our patient had sacrococcygeal involvement, which has rarely been reported. Moreover, the history of lumbar spine surgery and the possible association with CSF leakage required consideration.
A Morel-Lavallée lesion most commonly presents with pain and swelling and a palpable, fluctuant soft tissue mass. Ecchymosis, skin hypermobility, and hypesthesia or anesthesia may also occur. Symptoms usually appear within a few days following the onset of injury. However, diagnosis may be difficult and is often delayed, because the lesion is easily overlooked in the presence of underlying fractures and the skin surface is intact.
2) Hudson
6) reported that the diagnosis was delayed in about one-third of patients, and Rha et al.
14) reported that in up to one-third of all patients, symptoms may develop several months or years after the initial injury.
The passing of months to years after trauma defines a chronic Morel-Lavallée lesion. With time, the lesion may grow and become painful, indicating that a fibrous capsule has formed due to an inflammatory reaction, and may be misdiagnosed as some other soft tissue lesion or even a tumor. Overlying secondary skin changes such as discoloration, dryness, cracking, and even necrosis can occur.
5)
Various imaging modalities including ultrasonography, computed tomography (CT), and MRI are helpful in diagnosing a Morel-Lavallée lesion. Noninvasive approaches are usually used in the first, but invasive methods such as injection of a contrast agent into the cavity are infrequently performed.
8) Ultrasonography is a rapid, inexpensive, easy-to-perform imaging modality that can identify size, volume, and depth and allows real time evaluation, but the diagnosis can be nonspecific.
4) CT is readily available and the initial modality of choice to confirm fracture in acute trauma, but it has a risk of radiation and lacks precision for visualization of soft tissue detail. CT may show a fluid-fluid level caused by sedimentation of cellular blood components and a peripheral capsule surrounding the mass, especially in chronic lesions.
2) Some lesions may contain internal septations and fat globules.
3)
Although MRI is time-consuming and expensive, it does not involve exposure to radiation and demonstrates superior soft tissue detail over other imaging modalities, making it the preferred imaging modality for a Morel-Lavallée lesion. MRI signal characteristics are affected by the internal contents and chronicity of the lesion, mainly appearing as a fluid collection between the deep fascia and hypodermis and a peripheral capsule. Internal septations and fat globules can also be seen. Generally, a chronic lesion shows homogeneous hypointensity on T1-WI, hyperintensity on T2-WI, and a water-like MRI signal with a hypointense thick peripheral ring or capsule.
2711) As the lesion evolves and matures, a peripheral ring or capsule develops and appears hypointense on T1-WI and T2-WI due to the presence of hemosiderin and fibrous tissue.
715) In our case, MRI showed a fluid collection between the deep fascia and hypodermis, with homogeneous hypointensity on T1-WI, hyperintensity on T2-WI with internal septations, and a surrounding hypointense, thick peripheral capsule. Considering the trauma history, elapsed time after trauma, presence of a fluctuant soft tissue mass, aspirated serous fluid, MRI signal characteristics, and location between the deep fascia and hypodermis, was considered chronic.
There are no standard treatments for a Morel-Lavallée lesion. Treatment strategies are based on chronicity, size, severity, accompanying injuries including fractures, and presence of a peripheral capsule, among others.
Acute, small lesions without underlying fracture are usually treated conservatively with compression banding, medication, and absolute bed rest.
2416) Acute lesions that do not respond to conservative treatment and chronic lesions can be treated with ultrasonography-guided percutaneous drainage and sclerotherapy. Multiple clinical series reported good results using sclerotherapy with talc, doxycycline, or alcohol.
191013)
Surgical debridement has been attempted in lesions refractory to the above-mentioned treatments, acute lesions with an underlying open fracture, and chronic lesions with infection or skin necrosis.
4) Surgery is also indicated in patients with a chronic Morel-Lavallée lesion with a peripheral capsule because of resistance to conservative treatment and percutaneous drainage, and likelihood of recurrence.
4) Despite the fact that aspiration was performed twice at a local clinic and once in our institute, our patient showed rapid recurrence in spite of repeated drainage. As MRI showed a chronic lesion with a thick peripheral capsule, we performed surgical resection of the lesion and capsule removal.
CONCLUSION
A Morel-Lavallée lesion is an uncommon, closed internal degloving injury and can occur anywhere in the body. When the location is uncommon, the lesion can be diagnosed based on trauma history, elapsed time after trauma, presence of a fluctuant soft tissue mass, appearance of aspirated fluid, MRI signal characteristics, and location between the deep fascia and hypodermis. If there is no response to aspiration or repeated drainage, surgical resection should be considered.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download