Abstract
Involuntary movement of the cervical spine can cause damage to the cervical spinal cord. Cervical myelopathy may occur at an early age in involuntary movement disorders, such as tics. We report the case of a 21-year-old man with Tourette syndrome, who developed progressive quadriparesis, which was more severe in the upper extremities. The patient had abnormal motor tics with hyperflexion and hyperextension of the cervical spine for more than 10 years. High-signal intensity intramedullary lesions were observed at C3-4-5-6 level on T2 weighted magnetic resonance imaging. Examinations were performed for high-signal intensity intramedullary lesions that may occur at a young age, but no other diseases were detected. Botulinum toxin injection to the neck musculature and medication for tic disorders were administered. However, the myelopathy was further aggravated, as the involuntary cervical movement still remained. Therefore, laminoplasty was performed at C3-4-5-6, with posterior fixation at C2-3-4-5-6-7 to alleviate the symptoms. The neurological signs and symptoms improved dramatically. The management of tic disorders should be the first priority during treatment. However, surgical treatment may be necessary, if symptoms worsen after appropriate treatment.
Go to : 
Tourette syndrome (TS) is a childhood-onset neurodevelopmental disorder that is characterized by several motor and phonic tics. Tics usually develop before 10 years of age, exhibit a waxing and waning course and typically improve with increasing age. The prevalence of TS is approximately 1% in children and adolescents.3) If motor tics develop in the cervical spine, repetitive head and neck movements can cause spondylotic changes and myelopathy due to cumulative injury to the cervical spine.8) Patients with myelopathy due to tic disorders are usually between 9 to 27 years old.12468910) and are considerably younger than other patients with cervical myelopathy. Myelopathy is not diagnosed easily at a young age, owing to the possibility of other diseases besides tic disorders, thus, delaying treatment. Moreover, the exact treatment remains known.
We present the case of a 21-year-old man with TS and progressive weakness of all the extremities. Neck bracing and botulinum toxin injection administration were carried to control the severe cervical motion tics. However, the weakness progressed rapidly. Posterior cervical fusion was performed to alleviate the symptoms.
Go to : 
Herein, author asserts that the subject willingly participated in the study after having been verbally informed of all aspects of the study, and this study was approved by Institutional Review Board of Gyeongsang National University Hospital.
A 21-year-old man developed progressive weakness in both arms and legs 3 weeks prior to presentation. He first developed a vocal tic at 11 years of age, while motor tics developed 6 months ago. Motor tic patterns were excessive symptomatic neck motion when the right arm was raised. The neck showed repetitive hyperextension and hyperflexion. He was diagnosed with TS and was prescribed risperidone. His motor tics improved after medication, which worsened and became even more uncontrollable after 3 months. Repetitive neck movements occurred every 1–2 minutes. He developed a more violent form of motor tic, consisting of hyperflexion and hyperextension of neck and the utterance of peculiar meaningless vocal sounds. Three weeks before admission, the pain and temperature sensations decreased in the right upper and lower limbs, with weakness (grade IV) in the left upper and lower limbs. Moreover, the Babinski reflex and ankle clonus were positive and Hoffman sign was also observed. He often fell over due to severe ankle clonus and weakness. He experienced weakness and numbness in both arms, when the tics induced neck movements.
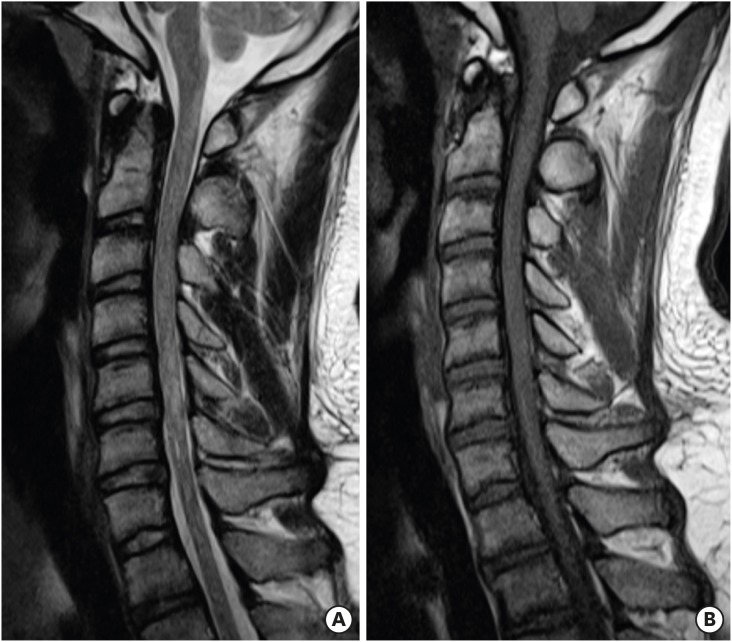
Cervical MRI showed disc bulging at the C5-6-7 level and high-signal intensity intramedullary lesion in the region of C2 to C7 on T2-weighted images (FIGURE 1). The preliminary diagnosis based on imaging findings was transverse myelitis or multiple sclerosis. We opted for a neurology consultation based on the imaging diagnosis. Neck bracing and injection of botulinum toxin into the cervical musculature were performed and medications were prescribed, to reduce neck movements induced by tics.
Neck movements due to tic disorder did not undergo improvement. After 3 days, weakness in all the extremities gradually worsened. Cervical spondylotic myelopathy due to neck motion can be estimated by the worsening of symptoms during neck movements. Therefore, surgical treatment was performed.
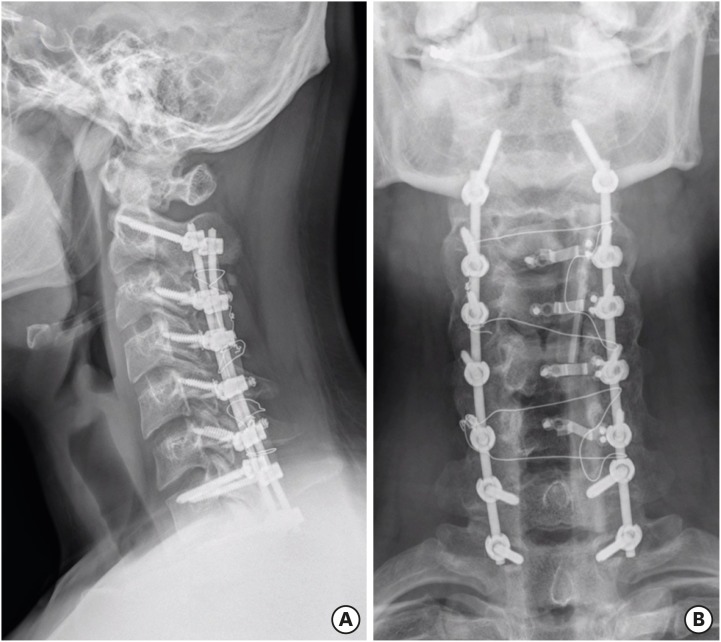
The patient underwent posterior open-door laminoplasty and posterior fixation at C2-3-4-5-6-7-T1 (FIGURE 2). After surgery, a Philadelphia neck brace was worn to prevent construct failure due to tics. The muscle power grade of both arms and legs recovered to grade V and Babinski sign and ankle clonus disappeared, 10 days postoperatively. Moreover, the fine motor function of the fingers was restored.
A recent plain radiograph of the cervical spine shows C3-4-5-6 laminoplasty and posterior fixation at C2-3-4-5-6-7-T1 are well maintained (FIGURE 3).
Go to : 
Tics are defined as sudden, rapid, recurrent, and non-rhythmic motor movements or vocalizations, usually appearing in bouts, and waxing and waning in frequency, intensity, and type. The onset of tic disorders including Gilles de la Tourette or TS is in childhood, typically at the age of 5 to 6 years. TS encompasses the combination of chronic (more than 1 year) motor and vocal tics.3)
Although the pathophysiology of cervical spondylotic myelopathy caused by tic movements is not fully understood, several theories have been suggested. Degenerative change is considered as a possible factor, since this condition is mainly reported in adults with degenerative change, compromising the spinal cord. Second, direct compression following repetitive hyperflexion and hyperextension can also damage the spinal cord. Damage to the anterior spinal artery due to minor injuries can also cause acute myelopathy.
Tics are usually seen in adolescents but the symptoms of myelopathy caused by tics, become apparent in the second decade of life.467) Myelopathy is caused by excessive repetitive hyperflexion and hyperextension in TS. High frequency of tics can cause early onset of symptoms. Cord swelling and high-signal intensity on MRI findings are also seen in cord tumors. Therefore, the diagnosis of cervical spondylotic myelopathy at a young age must be made after careful consideration. 18F-fluorodeoxyglucose positron emission tomography and contrast MRI should be carefully combined to make the final diagnosis.
Previously, cervical spondylotic myelopathy associated with TS was treated with different methods. The non-surgical treatment modality for controlling tics involves medication and botulinum toxin injection.12) However, clinical deterioration may occur if the tics are not effectively controlled and the neck movements are severe.7) In this case, neurological decompression and spinal fusion are performed through surgery. Moreover, deep brain stimulation may be considered for tics with self-injurious behaviors. This treatment was first introduced in 1999 for medically intractable TS. Since then, severe tics have been treated through deep brain stimulation of the thalamus, globus pallidus, and other brain regions.5) In our case, aggressive surgical immobilization effected a good clinical outcome, in addition to neck bracing, botulinum toxin injection, and psychological treatment.
Go to : 
Progressive cervical spondylotic myelopathy due to tic disorders is very rare. Its treatment still remains controversial. However, the control of movements induced by tics is the priority of treatment. Surgical treatment may be necessary if the symptoms worsen after appropriate treatment. Moreover, combined therapy including, neck bracing, botulinum toxin injection, and psychological treatment can be effective.
Go to : 
References
1. Adler CH, Zimmerman RS, Lyons MK, Simeone F, Brin MF. Perioperative use of botulinum toxin for movement disorder-induced cervical spine disease. Mov Disord. 1996; 11:79–81. PMID: 8771071.

2. Aguirregomozcorta M, Pagonabarraga J, Diaz-Manera J, Pascual-Sedano B, Gironell A, Kulisevsky J. Efficacy of botulinum toxin in severe Tourette syndrome with dystonic tics involving the neck. Parkinsonism Relat Disord. 2008; 14:443–445. PMID: 18337152.

3. Bloch MH, Leckman JF. Clinical course of Tourette syndrome. J Psychosom Res. 2009; 67:497–501. PMID: 19913654.

4. Dobbs M, Berger JR. Cervical myelopathy secondary to violent tics of Tourette's syndrome. Neurology. 2003; 60:1862–1863. PMID: 12796554.

5. Eddy CM, Rickards HE, Cavanna AE. Treatment strategies for tics in Tourette syndrome. Ther Adv Neurol Disorder. 2011; 4:25–45.

6. Isaacs JD, Adams M, Lees AJ. Noncompressive myelopathy associated with violent axial tics of Tourette syndrome. Neurology. 2010; 74:697–698. PMID: 20177125.

7. Ko DY, Kim SK, Chae JH, Wang KC, Phi JH. Cervical spondylotic myelopathy caused by violent motor tics in a child with Tourette syndrome. Childs Nerv Syst. 2013; 29:317–321. PMID: 23053364.

8. Krauss JK, Jankovic J. Severe motor tics causing cervical myelopathy in Tourette's syndrome. Mov Disord. 1996; 11:563–566. PMID: 8866498.

9. Lin JJ, Wang HS, Wong MC, Wu CT, Lin KL. Tourette's syndrome with cervical disc herniation. Brain Dev. 2007; 29:61–63. PMID: 17188440.

10. Muroi A, Matsumura A, Asakawa H, Enomoto T, Iwasaki N, Nose T. Myelopathy caused by tics in an adolescent, associated with T2 signal intensity changes of the spinal cord. Childs Nerv Syst. 2002; 18:191–194. PMID: 11981634.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download