This article has been
cited by other articles in ScienceCentral.
Abstract
Spinal subdural hematoma (SDH) is rarely reported, and their simultaneous occurrence with intracranial SDH is even more rare. A 67-year-old male patient with a history of posterolateral fusion to treat an L2 burst fracture came to our outpatient clinic due to an inability to walk by himself over the previous 3 weeks. A neurological examination revealed that the patient was alert with occasional confusion and slight motor weakness in the lower extremities. Brain and lumbar spine magnetic resonance imaging (MRI) was then performed. A brain MRI revealed a large subacute SDH along the right cerebral convexity and falx cerebri with midline shifting, and a spine MRI revealed a right side-predominant subacute SDH extending from L4 to S1. For treatment, burr hole trephination of the intracranial SDH and fluoroscopy-guided lumbar puncture of the spinal SDH were performed and resulted in a favorable outcome. This is a report of a rare case of spontaneous intracranial and lumbar spine SDH. We include a review of the current literature and a discussion of the pathogenesis of this condition in this report.
Go to :

Keywords: Spine, Brain, Subdural hematoma
INTRODUCTION
Spinal subdural hematoma (SDH) is uncommon, and while the precise mechanism for its pathogenesis remains unclear, a variety of hypotheses have been proposed, including trauma, dissection of the subarachnoid hemorrhage into the subdural space, vascular malformation, and anticoagulation.
3) The coexistence of intracranial and spinal SDH is even more rare than spinal SDH alone, and the pathogenesis of this phenomenon has not been well elucidated.
Here, we describe a case of concomitant spinal and intracranial SDH, where the intracranial SDH was treated with burr hole trephination and the spinal SDH was treated with fluoroscopy-guided percutaneous lumbar puncture. We also discuss the pathogenesis of this condition and potential treatment strategies.
Go to :

CASE REPORT
We obtained informed consent from the patient.
A 67-year-old male patient was admitted to our outpatient clinic for gait disturbance without lumbago or radiculopathy. The patient had been experiencing this weakness over the previous 3 weeks. He had a prior history of posterolateral fusion at T11–L1 for a T12 burst fracture at 3 years ago but denied any recent trivial head or spine injury as well as any special intervention procedure. He also had not taken any medications such as anticoagulants and had no history of blood dysplasia or coagulopathy.
The laboratory results from coagulation tests were all within normal limits.
A physical examination revealed mild tenderness of the postoperative lumbar spine with no other abnormalities. A neurological examination showed slight motor weakness in the lower extremities (GVI+/GVI+) and no sensory deficits. Although the patient was alert without evident neurological deficits, he did exhibit disorientation, especially with regard to time and place.
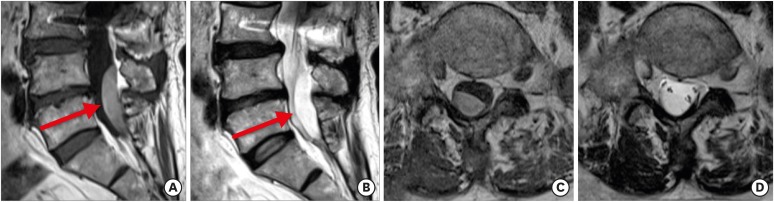
Brain and lumbar spine magnetic resonance imaging (MRI) were also performed. MRI of the lumbar spine also showed a right side-dominant subacute SDH at the L4 to S1 level (
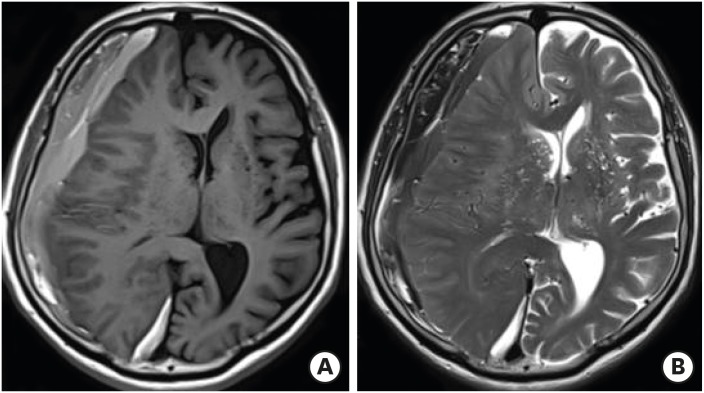
FIGURE 1). Brain MRI revealed a large subacute SDH along the right cerebral convexity and falx cerebri with midline shifting to the left side (
FIGURE 2).
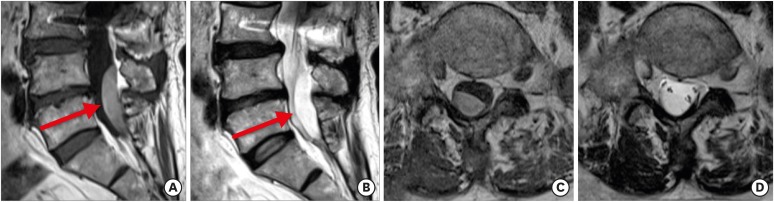 | FIGURE 1
Lumbar spine MRI images of the patient. Sagittal T1-weighted (A) and T2-weighted (B) images reveal a hematoma (arrows) in the dorsal spine at the L4–S1 level. Axial T1-weighted (C) and T2-weighted (D) images at the L5 level reveal a subacute subdural hematoma. The hematoma is right-side dominant.
MRI: magnetic resonance imaging.

|
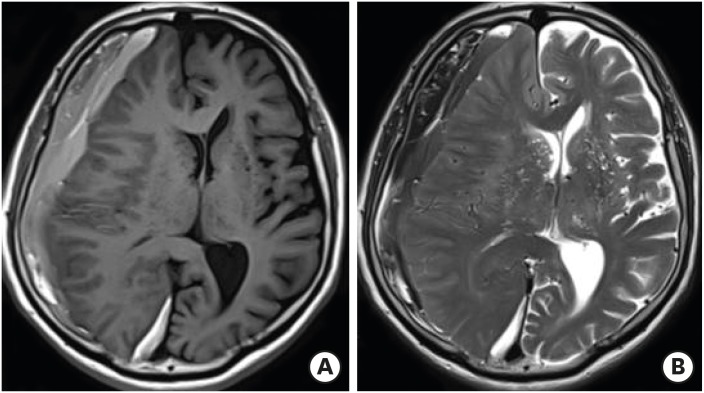 | FIGURE 2
Brain MRI images of the patient. Axial T1-weighted (A) and T2-weighted (B) MRI images demonstrate a large right-side subdural hematoma with slight hyperintensity compared to CSF. This MRI finding is typical of subacute SDH.
MRI: magnetic resonance imaging, CSF: cerebrospinal fluid, SDH: spinal subdural hematoma.

|
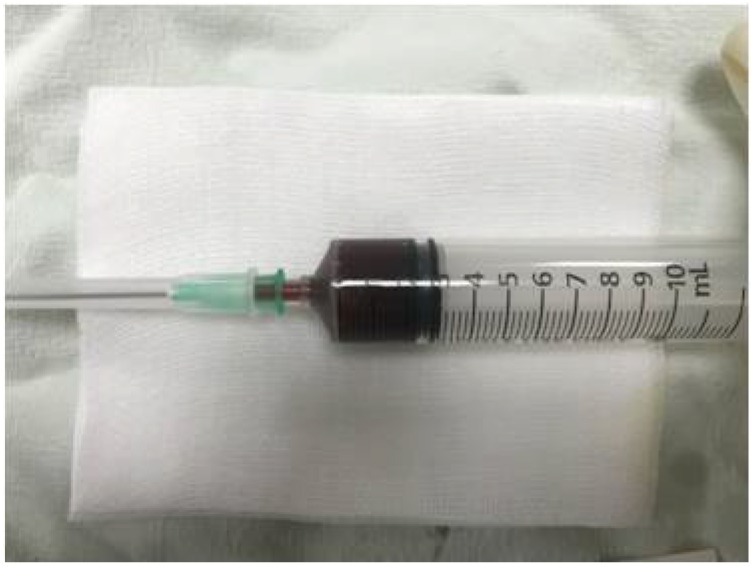
Due to the patient's persistent complaints of subjective weakness and the subacute spinal SDH focused at the L4 to S1 level, a percutaneous lumbar puncture under fluoroscopic guidance was performed. About 3 mL of dark-brownish serous drainage and well-liquefied blood was aspirated (
FIGURE 3). A computed tomography (CT) scan of the brain 3 days after fluoroscopy-guided lumbar puncture and bed rest revealed that the hematoma had resolved to chronic status.
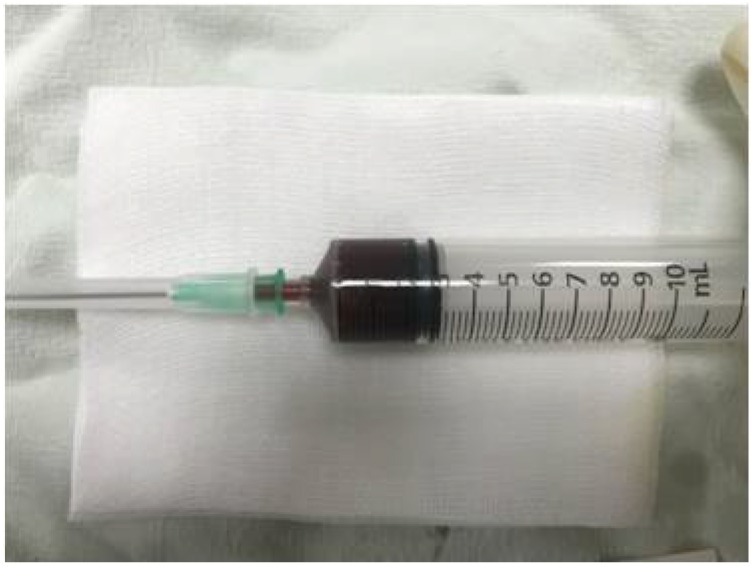 | FIGURE 3 Dark-brownish blood obtained with fluoroscopy-guided lumbar puncture.
|
Burr hole trephination for the right intracranial lesion was performed with a closed drainage system. After surgery, the patient's disorientation improved, and the subjective weakness in both of his lower limbs had completely improved.
Go to :

DISCUSSION
Concurrent intracranial and SDH is extremely rare, with only a few cases reported in the literature. Even less frequent are spontaneous SDHs associated with intraspinal hemorrhage.
47811) Spinal SDH is usually attributed to trauma, coagulopathy, vascular malformation, spinal puncture, recent lumbar instrumentation, and other invasive procedures. It can also occur spontaneously.
1013)
An asymptomatic spinal SDH may coexist in patients with intracranial SDH, but lumbar MRI is not routinely performed after burr hole surgery, especially in patients without clinical symptoms of spinal disorders. Spinal subdural space does not contain any major blood vessels or bridging veins that act as a source for a spinal SDH, which differs from circumstances that lead to intracranial SDH. The etiology of the simultaneous occurrence of intracranial and spinal SDH has not yet been elucidated; however, 2 main underlying mechanisms have been suggested: a traumatic spinal SDH, and migration from the cranial compartment to the spinal compartment.
The first of the potential mechanisms that may lead to concomitant intracranial and spinal SDH is a trauma-induced effect or accidental coincidence. In a prospective study, Kokubo et al.
5) reported the incidence of spinal SDH in patients with intracranial SDH. Among 168 patients, only 2 showed a concomitant lumbar SDH, and both patients had a history of trauma to both the brain and the spine. The authors thus postulated that the major pathogenic effect underlying their concomitant SDHs was double trauma and low cerebrospinal fluid (CSF) pressure. Others have also speculated that lumbar SDH is the result of direct trauma to the lumbar or hip area.
1)
The second potential mechanism that may lead to concomitant intracranial and spinal SDH is intracranial migration of an acute SDH. Yamaguchi et al.
14) reported that intracranial SDH may distribute to the spinal subdural space, particularly in the lumbar region due to the influence of gravity. The migration theory is supported by the fact that MRI revealed SDHs with the same intensity. The authors suggested that the growing hematoma may have torn the membrane, thus allowing it to move freely in the subdural space. In our case, a CT scan of the brain revealed a subacute SDH on the falx cerebri, which indicated that migrating hematoma leakage was leading to redistribution of the hematoma to the spine, most likely as a result of gravity. Moreover, MRI revealed continuity of the SDH from the cranium to the spine and both hematomas were of the same intensity.
In our case, we were unable to confirm a traumatic origin of the spinal SDH and believe that this case might be caused by the migration of the intracranial SDH to the spinal subdural space. The patient denied any trivial injuries to the brain, hip, or spine.
Most cases of concomitant intracranial and spinal SDH showed a good clinical outcome following conservative treatment. Prompt decompression should be considered, however, when the neurological deficits are rapidly progressive.
26912) In our case, we performed a fluoroscopy-guided lumbar puncture and achieved a good clinical outcome. The hematoma was able to be drained using a spinal needle because it had a clear border and was well-focused. This technique can provide an anatomically precise puncture site and eliminate the need for general anesthesia or laminectomy. We believe that a simple lumbar puncture under fluoroscopic guidance can be an appropriate treatment to improve clinical symptoms of patients with concomitant intracranial and spinal SDH.
Go to :

CONCLUSION
We reported a rare case of concomitant intracranial and spinal SDH without any traumatic events. We recommend a minimally invasive approach, such as burr hole trephination and fluoroscopy-guided lumbar puncture as a strategy for this rare condition.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download