This article has been
cited by other articles in ScienceCentral.
Abstract
Pseudoaneurysm of internal maxillary artery (IMA) after trauma is rare, and most cases reported are caused by maxilla-facial blunt trauma. Pseudoaneurysm is discontinuity in the vascular wall leading to an extravascular hematoma that freely communicates with the intravascular space producing pulsatile hematoma rapidly. A 44-years-old woman presented with a pulsatile swelling and pain in the left parotid region. She underwent the masticatory muscle reduction using needle injection in dentistry 1 month ago. The left facial pulsatile swelling developed after the procedure immediately and uncontrolled bleeding occurred on the day of visit to our institution. We performed emergency angiography and diagnosed pseudoaneurysm of left IMA. We treated by embolization with Histoacryl Glue through left IMA. IMA total occlusion was confirmed and symptoms improved. Pseudoaneurysm following blunt trauma of the face have been reported but are few. Furthermore, there is no report of IMA pseudoaneurysm due to direct injury by needle. Recently, many cosmetic surgery procedures using injection techniques have been performed, and it is necessary to pay attention to the direct vessel injury by the needle. And endovascular therapies can give early recovery with minimal morbidity and avoids injury to the facial nerve and its branches.
Go to :

Keywords: Pseudoaneurysm, Internal maxillary artery, Endovascular treatment
INTRODUCTION
Aneurysm is an irreversible dilatation of an artery. It may contain all layers of the artery wall (true aneurysm) or only a part of the wall and surrounding tissue (false or pseudoaneurysm). Traumatic aneurysm is an example of false aneurysm or pseudoaneurysm caused by injuries which rupture the full thickness of the arterial wall leading to extravasation of blood into surrounding tissues, resulting a pulsatile hematoma.
279) The compressed perivascular connective tissue forms the sac around this false or pseudoaneurysm. Internal maxillary artery (IMA) pseudoaneurysm may be caused as a possible complication of trauma, infection, occurring as a result of maxillofacial surgery, therapeutic or diagnostic arterial wall needle puncture. Rarely, IMA pseudoaneurysm may result from vasculopathy after radiation therapy or tumor invasion. Some cases of pseudoaneurysm following fractures of the facial bones have been reported but few. In recent years, the frequency of cosmetic procedures and operations for the face has been increasing, and the complications are becoming more diverse. This patient is also referred to here as a patient with IMA pseudoaneurysm who developed after masticatory muscle reduction and nerve block.
Go to :

CASE REPORT
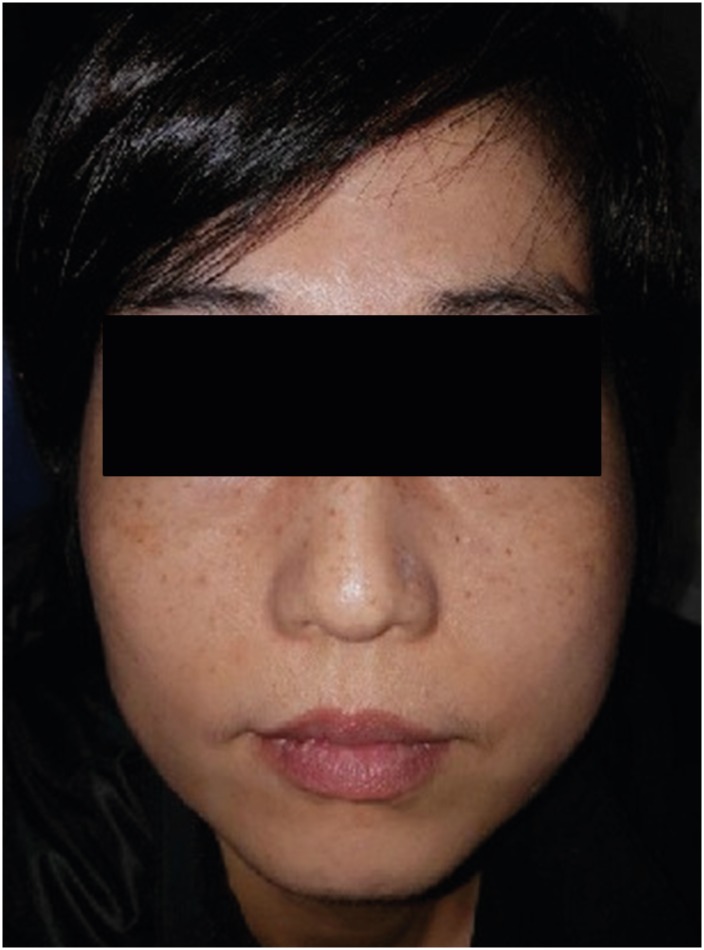
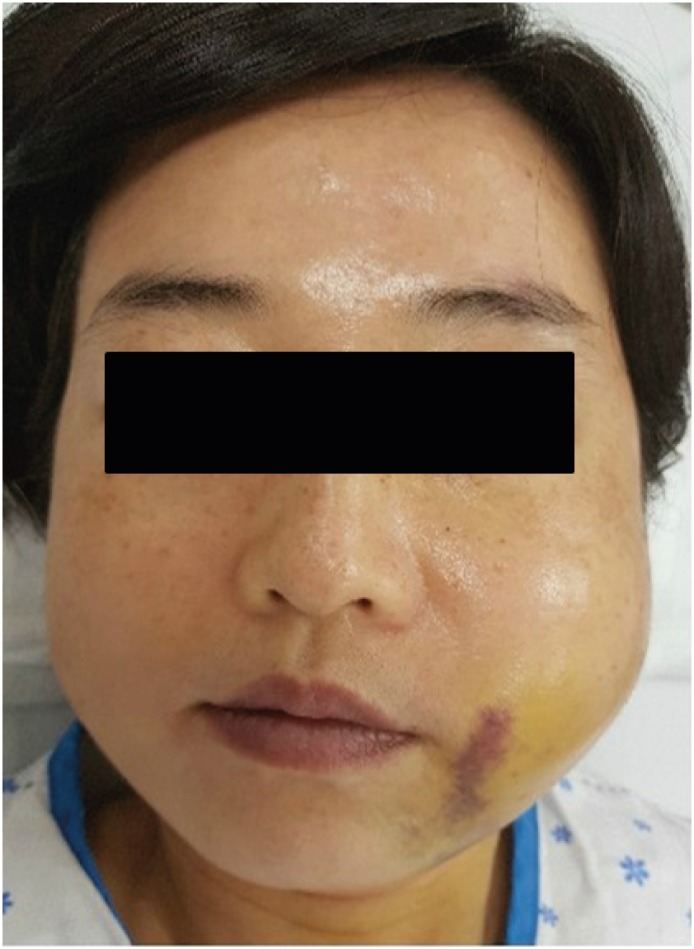
A 44-years-old woman presented with a pulsatile swelling and pain in the left parotid region. She underwent the masticatory muscle reduction using needle injection in dentistry 1 month ago. The left facial pulsatile swelling developed after the procedure immediately (
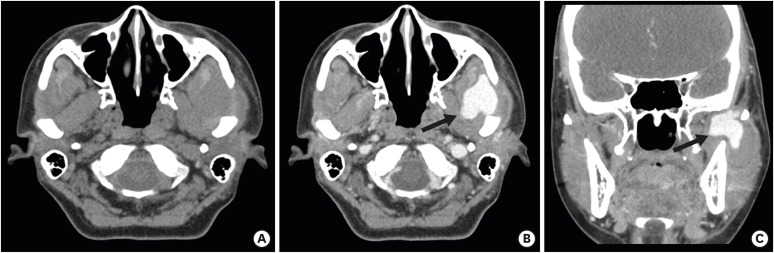
FIGURE 1). In this case, we observed extravasation of contrast in the buccal fat space when a low-density lesion of 32×30×40 mm size was observed in the left masticator space on neck contrast computed tomography (CT) performed on our patient's emergency room (
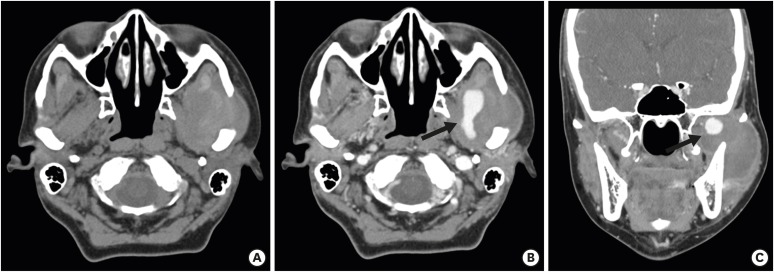
FIGURE 2). After incision & drainage under suspicion of cellulitis with hematoma, dental outpatient follow-up was decided. During follow-up, bleeding and swelling were continuously observed on drainage, and after paranasal-sinus CT (
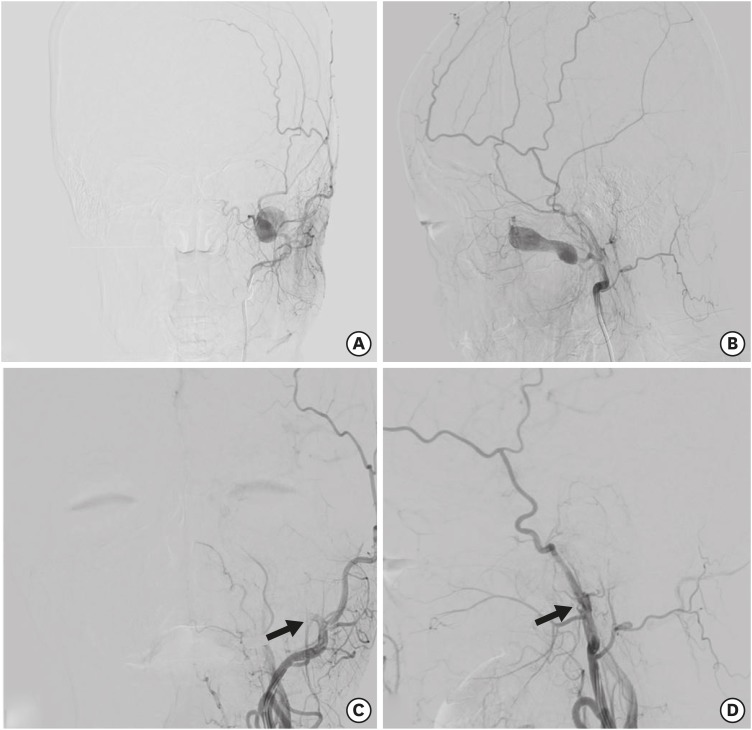
FIGURE 3), trans-femoral cerebral angiography was performed to our department to identify the vessel lesion. Left in external carotid artery selection, a sac-contrast filling was observed at the distal portion of the IMA (
FIGURE 4). This was diagnosed as pseudoaneurysm due to needling injury in the previous procedure. The microcatheter was placed at the base of the IMA, embolization was performed using Histoacryl glue, and pseudoaneurysm occlusion was confirmed (
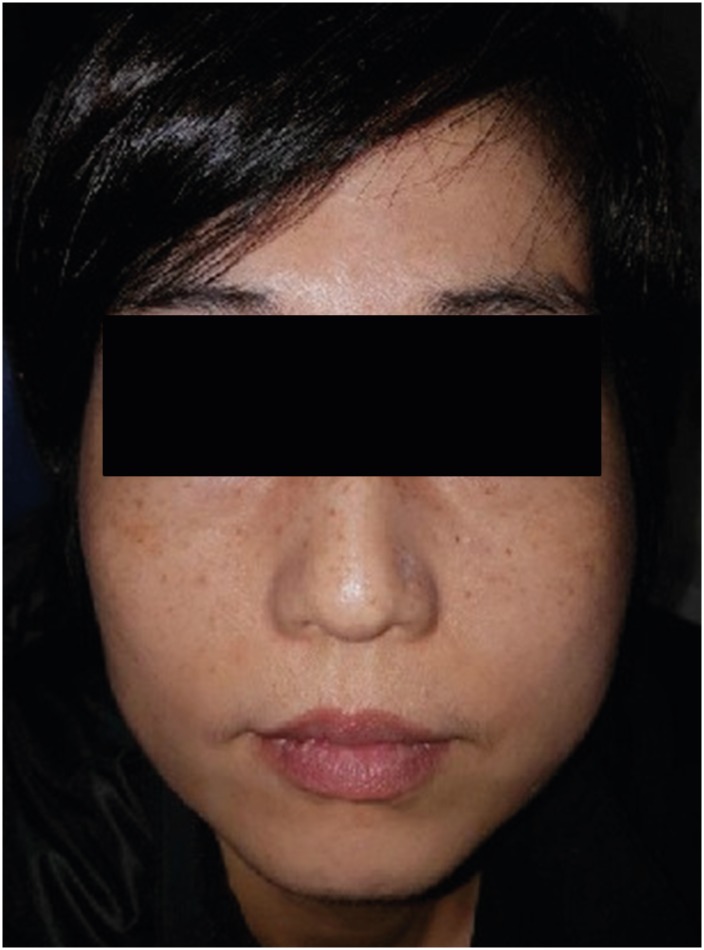
FIGURE 4). In follow-up, swelling and pain were improved (
FIGURE 5). She had not any other complication after procedure.
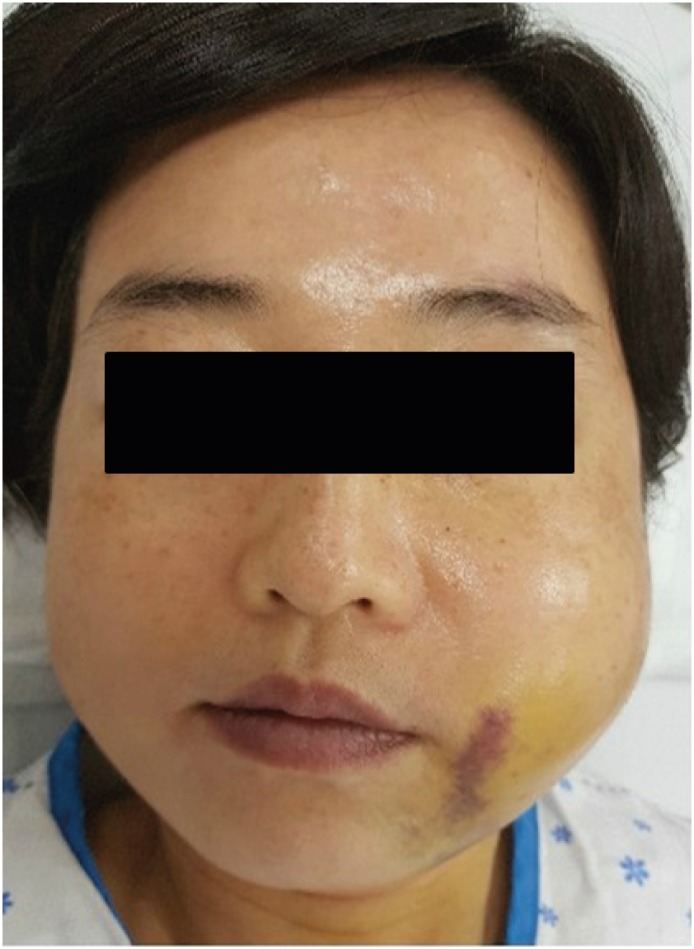 | FIGURE 1 Patient's appearance at the emergency room. Left facial swelling and ecchymosis was seen.
|
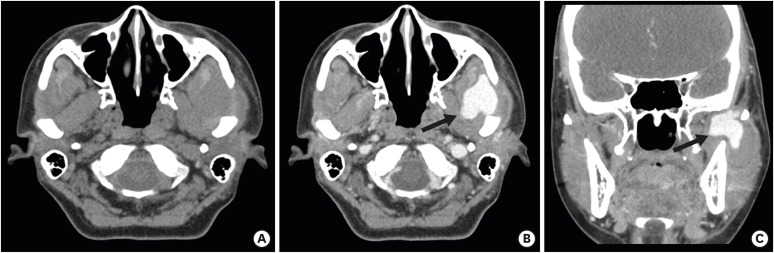 | FIGURE 2
Neck contrast CT images. (A) Pre-contrast axial, (B) Post-contrast axial, and (C) Post-contrast coronal. CT shows a low-density mass-like lesion at left masticator space with contrast extravasation (arrow).
CT: computed tomography.

|
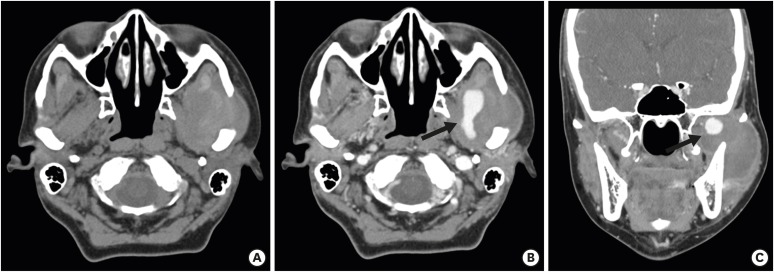 | FIGURE 3
Para-nasal sinus CT images. (A) Pre-contrast axial, (B) Post-contrast axial, and (C) Post-contrast coronal. CT shows that Further increased status of previous noted low-density mass-like lesion or loculated fluid at left masticator space but decreased contrast extravasation (arrow).
CT: computed tomography.

|
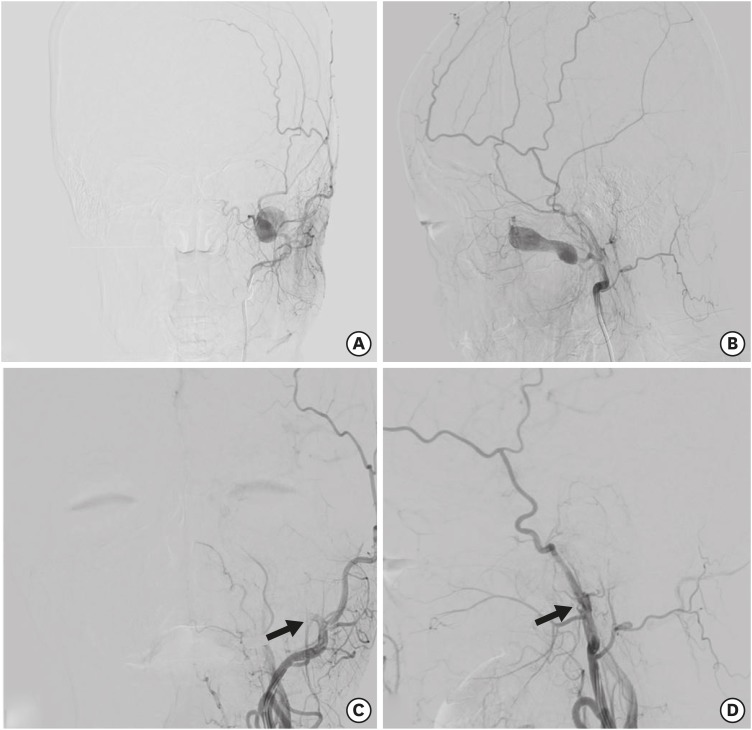 | FIGURE 4
Trans-femoral cerebral angiography images. Pre-operative; (A) Antero-posterior view, (B) Lateral view. Contrast filling mass-like pseudoaneurysm was seen in the left IMA proximal area. Post-operative; (C) Antero-posterior view, (D) Lateral view. Left proximal IMA was totally occluded by Histoacryl Glue (arrow).
IMA: internal maxillary artery.

|
 | FIGURE 5 Post-operative patient's appearance at the emergency room. There was seen that decreased left mandibular swelling.
|
Go to :

DISCUSSION
A pseudoaneurysm is a rare disease that causes life - threatening bleeding if diagnosis and treatment are delayed.
1)
In patients with a history of trauma to the face, the presence of cysts accompanied by systolic bruit should increase the suspicion of traumatic pseudoaneurysm and facilitate further evaluation through various investigations.
5) Diagnostics for this include CT scans and magnetic resonance imaging (MRI), ultrasonography and color Doppler. However, angiography remains the definitive and most important diagnostic procedure that provides valuable additional benefits in the treatment plan. Angiography can be combined with CT scan or MRI.
After confirmation, there are 2 treatment options that can be determined. There are 2 treatment options that you can choose between endovascular and surgical treatment.
6)
Endovascular treatment is currently being used as a major treatment method in many centers. The use of such interventions has improved access to surgically inaccessible microvascular vessels and reduced morbidity and mortality, such as complications such as general anesthesia and blood loss by surgery.
Embolization uses a variety of materials to block blood vessels. Commonly used materials include Gelfoam, Isobutyl-cyano-acrylate, Coils (Made from Dacron or Nylon Fiber). The criteria for selecting among these materials are selected in consideration of the properties of the embolic material and the like based on the position of the catheter and the catheter, the size and location of the catheter.
5)
Thus, endovascular treatment is a very attractive and minimally invasive approach, but without certain disadvantages. However, some skilled and experienced interventional therapists are needed to perform endovascular treatment.
3)
Minor complications include craniofacial pain, facial edema and paresthesia, nasopharyngeal ulcers and osmosis. The main complications are rare, but they include intraoperative rupture of the pseudoaneurysm wall, stroke and stroke and other cranial neuropathy due to embolism from aneurysm joint thrombus or embolic material to the brain, maxillary ischemic necrosis, tooth loss, and careless proximal branch obstruction.
411)
Surgical management remains the gold standard of treatment, especially in the case of large aneurysms and noninvasive approaches fail. In addition, lack of infrastructure and skilled expertise may be beneficial to the choice of surgical management.
810)
Go to :

CONCLUSION
Endovascular treatment with traumatic pseudoaneurysm of the IMA may be a better option, compared to surgical treatment. Moreover, consultation with not only the surgeon but also the interventional therapist may be helpful in establishing the treatment plan.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download