This article has been
cited by other articles in ScienceCentral.
Abstract
We report 3 cases of arachnoid cysts (ACs) that completely disappeared after burr hole drainage, without cyst fenestration into the subarachnoid space or cystoperitoneal shunt. The first patient was a 21-year-old female with an AC of the right cerebral convexity, found incidentally. After endoscopic AC fenestration was performed, the patient complained of persistent headache. Two-month postoperative brain imaging revealed reaccumulated AC and associated multi-stage subdural hematoma. Burr hole drainage was performed to resolve the chronic subdural hematoma (CSDH). Three months later, brain computed tomography showed that the CSDH and the AC had disappeared. The second patient was an 11-year-old male who had a history of trauma 1 month prior to presentation at the clinic. Brain magnetic resonance imaging revealed an AC in the left sylvian fissure with CSDH. We performed burr hole drainage to treat the CSDH first. Subsequently, the AC as well as the CSDH disappeared. The third case was an AC of the right parietal convexity, found incidentally. Only burr hole drainage was performed, following which, the AC disappeared. This case series shows that an AC can disappear naturally after rupture into the subdural space by trauma or the burr hole procedure.
Keywords: Arachnoid cysts, Trephination, Chronic subdural hematoma
INTRODUCTION
Arachnoid cysts (ACs) are congenital fluid filled cavities within arachnoid or between arachnoid and pia mater containing cerebrospinal fluid-like fluid. They most commonly occur in the middle fossa. The pathogenesis is still not clear, and little is known about its natural course. One of the common complications of ACs is the development of chronic subdural hematoma (CSDH) or hygroma. Several cases of spontaneous disappearance of ACs have been reported after occurrence of subdural hematoma or hygroma. The mechanism is not clear, but consecutive absorption of the cyst fluid after a tear in the cyst caused by trauma is one hypothesis for the spontaneous disappearance.
We report 3 cases of ACs that completely disappeared after burrhole drainage into subdural space, with or without cyst fenestration into subarachnoid space or cystoperitoneal shunt. All 3 of our cases were ACs located in supratentorium. In 2 of the 3 cases, CSDH was accompanied by an AC.
CASE REPORT
Informed consent was obtained from all individual participants included in this study. Our Institutional Review Board approved this study (IRB No, 2019-02-002).
Case 1
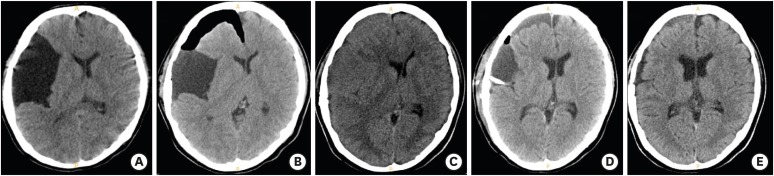
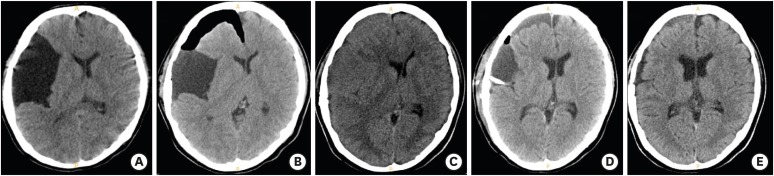
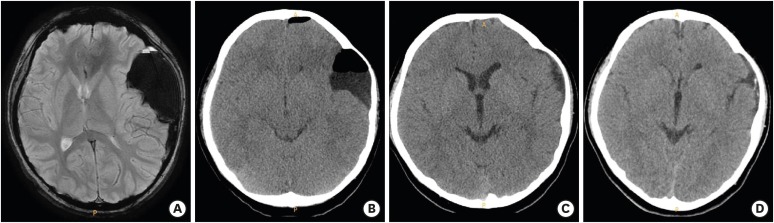
A 21-year-old female without any medical history visited the emergency clinic because of headache. A computed tomography (CT) scan showed an AC in the right middle cranial fossa (
FIGURE 1A). There was no evidence of recent hemorrhage. Because of persistent headache, endoscopic fenestration of the cyst wall was performed. An immediate postoperative CT scan showed that the size of AC was reduced. (
FIGURE 1B). However, the patient still complained of persistent headache, and postoperative 2-months brain CT scan revealed the multi-stage subdural hematoma in the right fronto-temporo-parietal convexity with midline shifting to the left side (
FIGURE 1C). Burrhole drainage was performed to resolve the subdural hematoma. We confirmed the neonembrane of the subdural hematoma and performed catheter drainage from the subdural space. No identification or treatment of the wall of the AC was performed at al. In brain CT scan after the burrhole drainage, CSDH disappeared, but a reaccumulation of AC was newly notified (
FIGURE 1D). The patient's headache was relieved without any neurologic deficit. Brain CT scan performed 3 months later showed an absence of CSDH as well as a significant regression of AC (
FIGURE 1E).
FIGURE 1
Illustration of case 1. (A) Preoperative CT scan showed an AC in the right middle cranial fossa, (B) Immediate postoperative CT scan showed that the size of AC was reduced. (C) Postoperative 2-months CT scan revealed the multi-stage subdural hematoma in the right fronto-temporo-parietal convexity with midline shifting to the left side, (D) After burrhole drainage, CSDH disappeared, but reaccumulation of AC was newly notified, and (E) Follow-up CT scan performed 3 months after burrhole drainage showed an absence of CSDH as well as a significant regression of the AC.
CT: computed tomography, AC: arachnoid cyst, CSDH: chronid subdural hematoma.
Case 2
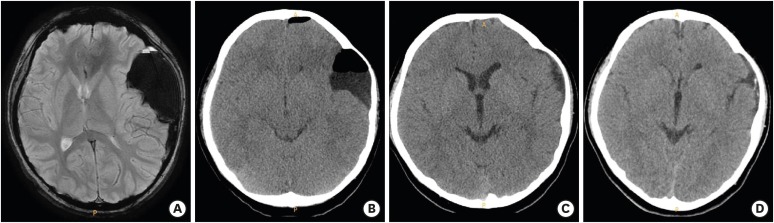
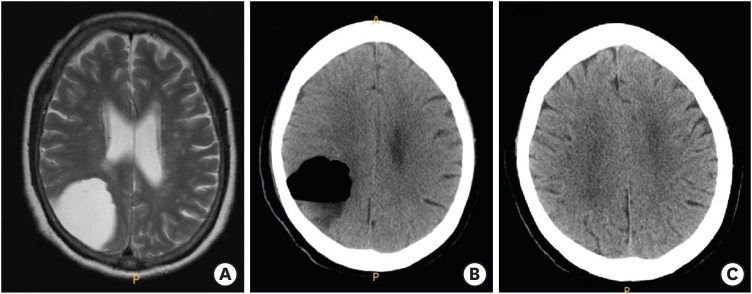
The second patient was an 11-year-old male patient, who had trauma history 1 month ago. He underwent brain magnetic resonance imaging (MRI) because of sudden headache and vomiting started from 2 days ago, and AC in left sylvian fissure and CSDH with subfalcian herniation were revealed (
FIGURE 2A). We planned to treat CSDH first by burrhole drainage and then consider managing AC afterward. We performed burrhole trephination and natural drainage for 1 night after confirming the presence of chronic subdural membrane. Postoperative CT scan showed disappearance of CSDH and remaining AC with air density (
FIGURE 2B). The clinical symptoms including headache and vomiting were completely improved. During the outpatient follow-up period of 18 months, the brain expanded and AC disappeared without any further management (
FIGURE 2C). The AC as well as CSDH did not recur for 18 months since the burrhole drainage for CSDH. Brain CT at postoperative 18 months showed dural calcification in temporal area (
FIGURE 2D).
FIGURE 2
Illustration of case 2. (A) Brain CT showed an AC in left sylvian fissure and accompanied CSDH with subfalcian herniation, (B) Postoperative CT scan revealed disappearance of CSDH and remaining AC with air density, (C) In the follow-up CT scan 18 months after burrhole drainage, the brain expanded and AC disappeared without further management, and (D) The AC as well as CSDH did not recur until 18 months after burrhole drainage for CSDH.
CT: computed tomography, AC: arachnoid cyst, CSDH: chronid subdural hematoma.
Case 3
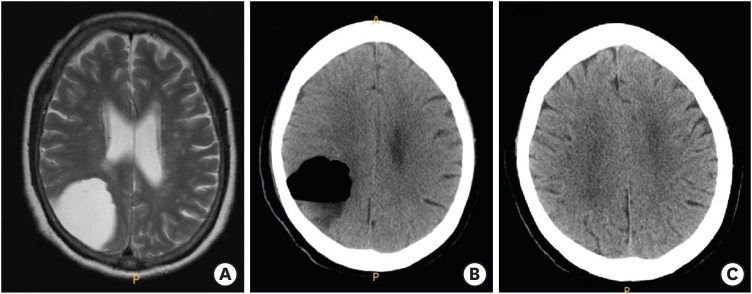
A 65-year-old woman with a history of hypertension visited department of neurology because of facial palsy. Facial palsy improved after medical treatment, but brain MRI performed to evaluate facial palsy revealed an AC in the right parietal convexity (
FIGURE 3A). The burrhole trephination and catheter drainage within the cyst were performed after a dura incision (
FIGURE 3B). There was no new neurologic symptom after the surgery. Postoperative 3 months CT scan showed a complete disappearance of AC (
FIGURE 3C).
FIGURE 3
Illustration of case 3. (A) Brain MRI revealed an AC of the right parietal convexity found incidentally, (B) Post-burrhole trephination CT scan. Catheter drainage was performed after dura incision (C) Postoperative 3 months CT scan showed complete disappearance of AC.
MRI: magnetic resonance imaging, CT: computed tomography, AC, arachnoid cyst.
DISCUSSION
This case series shows that the ACs disappeared after burrhole drainage. In first 2 cases, CSDH was accompanied, and burrhole drainage was performed within the subdural space. In the third case, burrhole drainage was performed within the AC. The etiology of AC is still controversial and unknown.
4) There are several theories that attempt to explain the formation of ACs; agenesis in certain part of the brain, a minor aberration in the development of the arachnoid, and developmental defect from condensation of the mesenchyme or abnormalities of CSF flow.
316) Some of suggested mechanisms that explain the growth of the cyst are the ball valve hypothesis that an one-way flow from the subarachnoid space into the cyst increases the cyst, osmotic gradient theory that the osmotic gradient in the cystic fluid caused by microhemorrhage within the cystic cavity diffuses the liquid into the cyst, and fluid production theory that borderline cells lining the walls of the cyst produce cystic fluid.
3710)
One of the main complications of the AC is CSDH or subdural hygroma, and 2 of our cases were accompanied by CSDH.
261319) The pathogenesis of AC-related CSDH is not clear, but it can occur even when the trauma is negligible or minor. A few authors suggest that CSDH may occur from either the vessels surround the cyst wall or floating vessels in the cyst.
1319) Although some authors have emphasized the structure between the dura and the arachnoid membrane, it is almost impossible to identify the bleeding point during AC-related CSDH surgery due to the distortion of original anatomical structure by hematoma.
89) Page et al.
13) proposed 2 hypotheses to explain the cause of CSDH accompanied with AC. The first is that the bridging vein of the cyst wall easily ruptures from receiving pressure through the cyst. The second hypothesis is that AC is more easily ruptured than normal brain, thus the cyst cavity provides the fluctuating movement of the cystic fluid and the shearing force being transmitted to the outer membrane. Therefore, the small vessels tearing between the outer arachnoid membrane and the dura results in a symptomatic chronic stage. This would explain that most AC-related CSDH patients have an absent or minor trauma history.
Treatment of AC includes craniotomy and fenestration, endoscopic fenestration, and cystoperitoneal shunt. However, the optimal treatment of AC with subdural fluid collection is controversial.
17) In few cases, spontaneous non-surgical resolution of AC after head trauma has been reported. Most of these cases happened in young men, and the most common site was middle cranial fossa. In 1986, Yamanouchi et al.
20) reported that the cyst of the middle cranial fossa was spontaneously decreased after a head trauma. They assumed that the cystic fluid would have been drained into the subdural space and reabsorbed there. Mori et al.
12) reported 2 similar cases, consistent with those of Yamanouchi et al.
20) in the reduction and spontaneous disappearance of AC. Cullis and Gilroy
5) described that they confirmed a connection between the cyst and the subdural space during operation. Spontaneous reduction of AC has also been reported in cases of posterior fossa. Arunkumar et al.
1) reported a spontaneous reduction of cyst located along the midline, which required surgical treatment due to symptom recurrence and re-expansion of cyst. In another case reported by Takagi et al.,
18) cyst was located at the cerebello-pontine angle. A complete resolution of the posterior fossa cyst was reported in a 7-month-old child.
14) Three other cases were reported by Moon et al.
13) and Poirrier et al.
15)
Most of these reported literature shows that the spontaneous reduction of AC can occur after a mild trauma. In the former 2 of our 3 cases, trauma led to CSDH and burrhole drainage was performed within subdural space. In the third case, burrhole drainage was performed within the cyst itself, and it served as an artificial trauma causing the pressure inside the cyst to be directed outwards, resulting in cyst reduction. Communication between cyst and subdural space occurred due to trauma in the 2 cases with CSDH, and an artificial communication was caused by burrhole drainage in the third case. The pressure inside the cyst resulted by the traumatic connection from the tearing of the cyst wall caused the fluid to drain out and the disappearance of AC. In all 3 cases, the interval from the burrhole drainage to the complete disappearance of the cyst was at least 3 months. Along with the reduction of AC, the patients' symptoms including headache also improved.
We believe that some ACs can be treated with burrhole drainage, especially in cases accompanied with CSDH after rupture into subdural space. If a traumatic connection is maintained between the cyst and the subdural space, regression and disappearance of AC after drainage might be expected.
CONCLUSION
In all 3 cases, the AC remained completely disappeared after the burrhole trephination. This case series shows that the AC can disappear naturally after being ruptured into the subdural space by the trauma or burrhole procedure. The natural course of ACs is dynamic, and intracystic and intraparenchymal pressure is likely to be involved in the process. Further prospective study will be needed to clarify the mechanism.
ACKNOWLEDGMENT
This work was funded by Soonchunhyang University Research Fund.
References
1. Arunkumar MJ, Haran RP, Chandy MJ. Spontaneous fluctuation in the size of a midline posterior fossa arachnoid cyst. Br J Neurosurg. 1999; 13:326–328. PMID:
10562848.
2. Bilginer B, Onal MB, Oguz KK, Akalan N. Arachnoid cyst associated with subdural hematoma: report of three cases and review of the literature. Childs Nerv Syst. 2009; 25:119–124. PMID:
18839182.

3. Catala M, Poirier J. Arachnoid cysts: histologic, embryologic and physiopathologic review. Rev Neurol (Paris). 1998; 154:489–501. PMID:
9773082.
4. Cincu R, Agrawal A, Eiras J. Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg. 2007; 109:837–843. PMID:
17764831.

5. Cullis PA, Gilroy J. Arachnoid cyst with rupture into the subdural space. J Neurol Neurosurg Psychiatry. 1983; 46:454–456. PMID:
6101185.

6. Domenicucci M, Russo N, Giugni E, Pierallini A. Relationship between supratentorial arachnoid cyst and chronic subdural hematoma: neuroradiological evidence and surgical treatment. J Neurosurg. 2009; 110:1250–1255. PMID:
18976058.

7. Gosalakkal JA. Intracranial arachnoid cysts in children: a review of pathogenesis, clinical features, and management. Pediatr Neurol. 2002; 26:93–98. PMID:
11897472.

8. Haines DE, Harkey HL, al-Mefty O. The “subdural” space: a new look at an outdated concept. Neurosurgery. 1993; 32:111–120. PMID:
8421539.
9. Kushida Y, Terao H, Shibata I, Shishido M, Seiki Y, Tsutsumi S. Chronic subdural hematoma associated with arachnoid cyst--study of the mechanism of its development. No Shinkei Geka. 1983; 11:1211–1217. PMID:
6664448.
10. Martínez-Lage JF, Poza M, Sola J, Puche A. Congenital arachnoid cyst of the lateral ventricles in children. Childs Nerv Syst. 1992; 8:203–206. PMID:
1394251.
11. Moon KS, Lee JK, Kim JH, Kim SH. Spontaneous disappearance of a suprasellar arachnoid cyst: case report and review of the literature. Childs Nerv Syst. 2007; 23:99–104. PMID:
16944178.

12. Mori T, Fujimoto M, Sakae K, Sakakibara T, Shin H, Yamaki T, et al. Disappearance of arachnoid cysts after head injury. Neurosurgery. 1995; 36:938–941. PMID:
7791985.

13. Page A, Paxton RM, Mohan D. A reappraisal of the relationship between arachnoid cysts of the middle fossa and chronic subdural haematoma. J Neurol Neurosurg Psychiatry. 1987; 50:1001–1007. PMID:
3655804.

14. Pandey P, Tripathi M, Chandra PS, Singh VP, Mehta VS. Spontaneous decompression of a posterior fossa arachnoid cyst: a case report. Pediatr Neurosurg. 2001; 35:162–163. PMID:
11641628.

15. Poirrier AL, Ngosso-Tetanye I, Mouchamps M, Misson JP. Spontaneous arachnoid cyst rupture in a previously asymptomatic child: a case report. Eur J Paediatr Neurol. 2004; 8:247–251. PMID:
15341907.

16. Robinson RG. The temporal lobe agenesis syndrome. Brain. 1964; 87:87–106. PMID:
14152215.

17. Sprung C, Armbruster B, Koeppen D, Cabraja M. Arachnoid cysts of the middle cranial fossa accompanied by subdural effusions--experience with 60 consecutive cases. Acta Neurochir (Wien). 2011; 153:75–84. PMID:
20931240.

18. Takagi K, Sasaki T, Basugi N. Spontaneous disappearance of cerebellopontine angle arachnoid cyst: report of a case. No Shinkei Geka. 1987; 15:295–299. PMID:
3496551.
19. Wester K, Helland CA. How often do chronic extra-cerebral haematomas occur in patients with intracranial arachnoid cysts? J Neurol Neurosurg Psychiatry. 2008; 79:72–75. PMID:
17488784.

20. Yamanouchi Y, Someda K, Oka N. Spontaneous disappearance of middle fossa arachnoid cyst after head injury. Childs Nerv Syst. 1986; 2:40–43. PMID:
3731162.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download