Abstract
A 57-year-old male had cardiac arrest during an operation of traumatic acute subdural haematoma (ASDH) and intraparenchymal haemorrhage in the infratentorium due to a great amount of bleeding from the pre-injured venous sinus. After effective bleeding control using a gauze, the patient recovered without additional neurological sequelae. The operation of traumatic ASDH in the infratentorium always poses a risk of excessive bleeding from the injured venous sinus that could be life-threatening to the patient. This risk could be avoided with the effective first method that can immediately control the bleeding.
Go to : 
In about 71% cases, acute subdural haematoma (ASDH) occurs mainly due to a trauma.4) Traumatic ASDH in the infratentorium is very rare, and its incidence rate is 0.5–1.6% of all traumatic ASDH.2) The mainstay of management for a significant amount of ASDH is a surgical operation.3) However, the outcome of ASDH in the infratentorium is poor.4) There can be a risk of excessive blood loss from the injured venous sinus and even a disastrous result during an operation for ASDH. In the present report, we operated a patient with traumatic ASDH in the infratentorium accompanied by intraparenchymal cerebellar haemorrhage. There was profuse bleeding from the subdural aspect of the pre-injured venous sinus leading to cardiac arrest during the operation. The patient was resuscitated after bleeding control with a gauze packing and recovered alert mentality without additional neurological sequelae. In the present study, we report this case and discuss the implications.
Go to : 
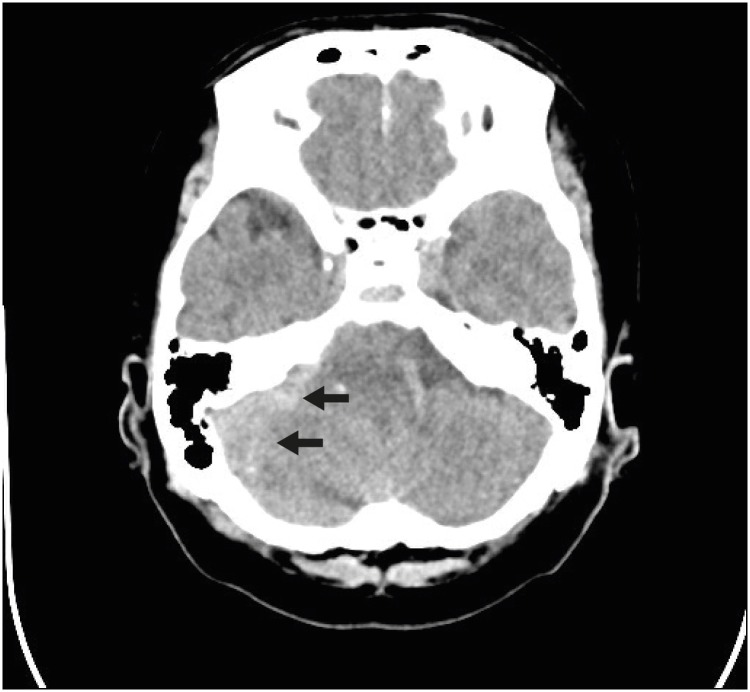
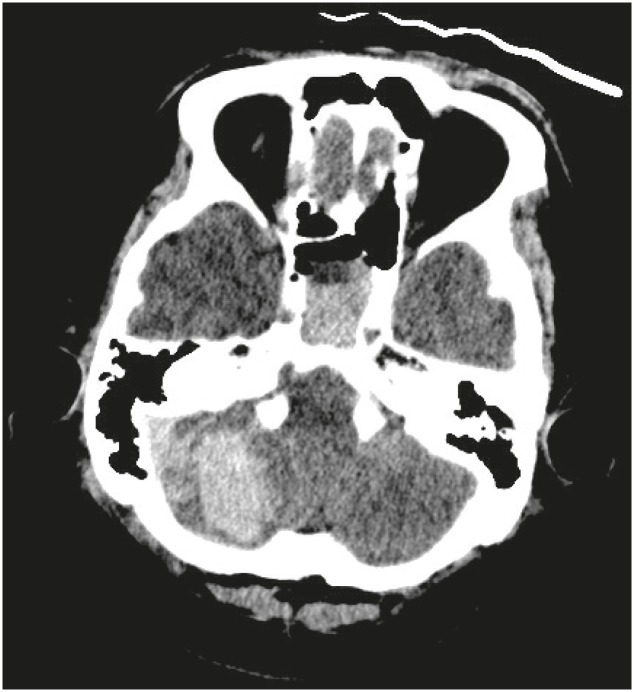
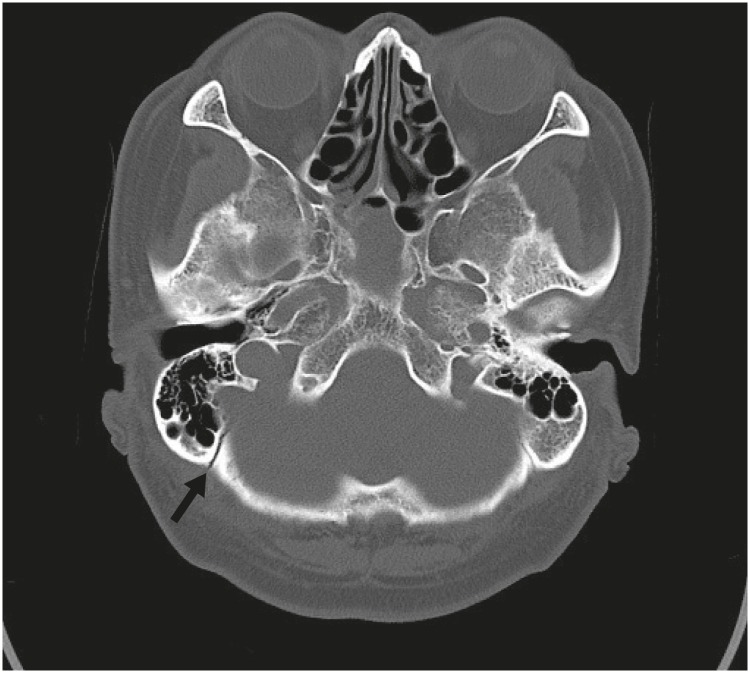
A 59-year-old male was transferred to our hospital presenting with a headache after falling backward. No neurological deficit was observed. The brain computerized tomography (CT) at the first hospital showed a small amount of ASDH in the right side of posterior fossa (FIGURE 1). The patient was admitted to our intensive care unit for careful observation of his neurological status without operation. Several hours after the admission, the patient's condition got worse to drowsy from alert mentality. The follow-up brain CT revealed a newly developed intraparenchymal haemorrhage in the right cerebellar hemisphere and an increased amount of the right subdural haematoma (FIGURE 2). The right intracerebellar parenchymal haemorrhage was considered to be the main cause of the deterioration of mentality.
After informed consent, the patient was transferred to an operation room. A midline incision and right suboccipital craniotomy were performed in a prone position under general anaesthesia. Most of the intraparenchymal hemorrhage was smoothly removed. However, as soon as we removed the haematoma located around the right lower lateral corner covered with unresected bone, a sudden excessive blood poured into the operation field. Due to the huge amount of bleeding and the bone, which had not been resected at the beginning of the operation, concealing the bleeding point, the location of the bleeding point could not be determined. The bleeding seemed to be from a venous sinus at the far lower lateral corner of right posterior fossa. To stop the bleeding, TachoSil (Baxter, Deerfield, IL, USA) was used, but to no avail. The amount of bleeding was increasing and became rampant and uncontrollable. The blood pressure decreased so rapidly that we did not have enough time to use another way of hemostasis. Eventually a cardiac arrest occurred in 2 or 3 minutes. For the immediate cardiopulmonary resuscitation, we promptly packed a 4×8-inch gauze into the bleeding site for the bleeding control and closed the wound by suturing of the skin directly without dura or subcutaneous closure, with one-third of the gauze remaining in the epidural space. During the closure, only a small amount of blood oozing was observed through the packed gauze. The patient's heart rhythm recovered soon after an injection of epinephrine and the gauze packing while closing the skin.
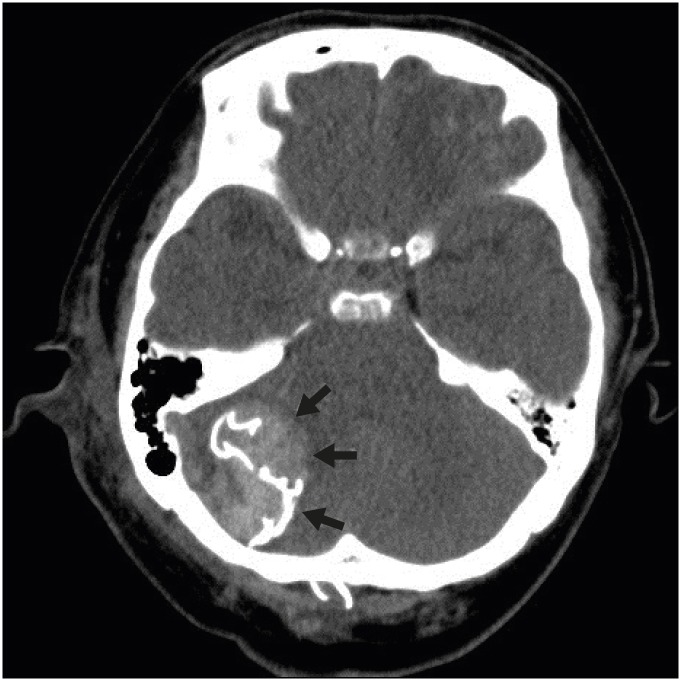
We quit the operation at that point and transferred the patient to the intensive care unit. He was relatively stable; the blood pressure was around 100 mmHg, the pupils were isocoric and showed a prompt light reflex. On day 2 after the operation, the brain CT showed no significant intraparenchymal hemorrhage around the gauze, ischemic lesion, and brain stem compression except the hyperdense shadow of the gauze (FIGURE 3). In the next several days, the patient gradually recovered to drowsy mentality without significant motor weakness. The patient became febrile over 38°C from the second post-operation day.
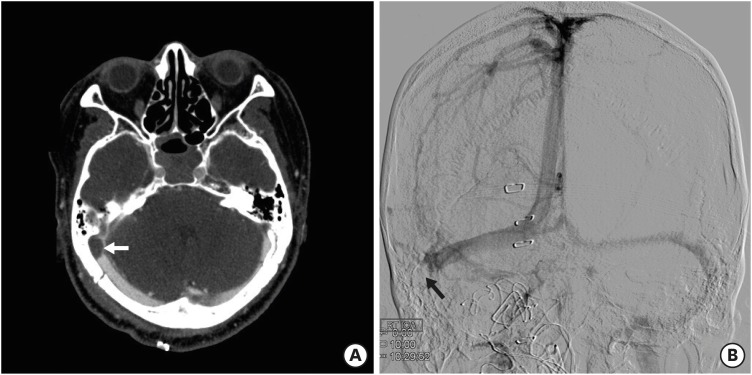
On day 10 after the operation, the patient got the second operation to remove the previously packed gauze. The enhanced preoperative brain CT showed occlusion of the right transverse sinus at the distal end, and we confirmed that again with transfemoral cerebral angiography for a safe surgery (FIGURE 4). While reviewing the images before the second surgery, we found that there was a diastatic fracture of right occipitomastoid suture around the subdural hematoma (FIGURE 5). The fracture might have caused the sigmoid sinus injury and the development of the subdural haematoma. During the removal of the gauze, no recurrent haemorrhage from the sinus, which had been expected through the enhanced preoperative CT and the cerebral angiography, was observed. There was no intraparenchymal hemorrhage inside and around the gauze. The patient improved to the light drowsy status on day 2 after the operation and became afebrile immediately after the second operation. He was getting better over time and became alert. On day 26 after the second operation, he was transferred to the rehabilitation department for the management of gait difficulty.
Go to : 
During an operation for ASDH in the posterior fossa, bleeding from an injured venous sinus can be profuse, thereby even resulting in fatal consequences. In some cases, it is not easy to control the abundant amount of subdural sinus bleeding from the unexposed area covered with bone in the infratentorium. Spending too much time with ineffective methods trying stop the pouring subdural blood from the venous sinus could result in instant cardiac arrest. Therefore, in the event of an excessive amount of subdural sinus bleeding in spite of using all measures to stop the bleeding, and if there is no enough time to prevent hypovolemic shock, we have to use the most reliable and easily applicable method first to prevent cardiac arrest. In our first operation, the bleeding was very rapidly and effectively controlled using the gauze packing into the bleeding site. Only some blood oozing through the packed gauze was observed during the suturing of the skin. This method was not only prompt, but also safe, as there was no significant intraparenchymal haemorrhage around the gauze, ischemic lesion or mass effect against the brain stem on the brain CT after the first operation. This method has been used for a long time; a recent report has documented a successful application of this method to control a severe venous sinus bleeding in a patient with acute epidural hematoma.1)
We performed the second operation for the removal of the gauze 10 days after the first operation. As expected from the enhanced brain CT checked before the second operation where there was an occlusion of transverse sinus at the distal end, no bleeding from the inside of the operation field while removing the packed gauze was observed. In the second surgery, there was an abscess under the skin at the lower side of the first operation wound. Therefore, to avoid abscess formation, as long as the sinus occlusion could be confirmed, it would be better to do reoperation as early as possible before 10 postoperative day.
If the sinus is not occluded after the gauze packing, it can be occluded using the coil embolization technique before the second operation to prevent the dangerous rebleeding after the consideration of the benefit to risk ratio for the sinus embolization.1) The acute venous sinus occlusion can cause several complications, such as venous infarction, intracranial hemorrhage, edema, subarachnoid hemorrhage, as well as rapidly progressive illness and coma.1) According to a recent report, the venous sinus remained patent three days after the operation of acute epidural hematoma removal and gauze packing.1) To prevent a dangerous rebleeding, the operators successfully occluded the injured sinus using the coil embolization technique. There was no sign of contrast leakage and venous hypertension in the post-embolization angiograms. Considering the high-risk of rebreeding, this technique can be a good option to ensure safety of the second operation.
In a trauma patient with an operable amount of intraparenchymal haemorrhage accompanying a small amount of ASDH near the dural sinus in the posterior fossa, it is necessary to try not to overlook the small amount of subdural haematoma and not to focus only on intraparenchymal haemorrhage. An effort should be made to find a fracture line, including diastatic fracture crossing the dural sinus over the subdural haematoma. This will help the operator to prepare and avoid an unexpected catastrophic bleeding from the injured venous sinus.
Go to : 
During the operation of traumatic ASDH in the posterior fossa, the operator should keep in mind that there can be a sudden unexpected profuse subdural bleeding from the pre-injured venous sinus which can cause cardiac arrest and a gauze packing can be the most simple and efficient method to choose first for bleeding control. And the fact that venous sinus can be occluded spontaneously several days after gauze packing gives us another option on future planning after the sinus bleeding control with gauze packing.
Go to : 
References
1. Kim JH, Yu SH, Kim BC, Lee JH, Lee JI, Choi HJ. Endovascular treatment following gauze packing for the control of massive bleeding from traumatic transverse sinus lesion. Korean J Neurotrauma. 2018; 14:150–154. PMID: 30402436.

2. Motohashi O, Kameyama M, Shimosegawa Y, Fujimori K, Sugai K, Onuma T. Single burr hole evacuation for traumatic acute subdural hematoma of the posterior fossa in the emergency room. J Neurotrauma. 2002; 19:993–998. PMID: 12225659.

3. Phan K, Moore JM, Griessenauer C, Dmytriw AA, Scherman DB, Sheik-Ali S, et al. Craniotomy versus decompressive craniectomy for acute subdural hematoma: systematic review and meta-analysis. World Neurosurg. 2017; 101:677–685.e2. PMID: 28315797.

4. Vega RA, Valadka AB. Natural history of acute subdural hematoma. Neurosurg Clin N Am. 2017; 28:247–255. PMID: 28325459.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download