This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Total disc replacement (TDR) is frequently performed anterior approaching method for the patients diagnosed with cervical disc herniation. This study aimed to assess the degree of ossification of the posterior longitudinal ligament (OPLL) progression after cervical TDR.
Methods
Twenty-two male soldiers who underwent cervical TDR surgery from 2009 to 2016 and were followed-up for more than 12 months were enrolled. The enrolled patients were classified as; 1) patients with pre-existing OPLL and without; and 2) patient showing progression of OPLL or not.
Results
Twenty-two men were included in the analysis. The mean follow-up period from the surgery was 41.4 months (range, 12–114 months). The mean age of all patients was 40.7 years (range, 31–52 years). TDR-only was used in 7 cases, and the hybrid surgery (TDR+ACDF) was used in 15 cases. The incidence of progression or newly development of OPLL was significantly higher in pre-existing OPLL group (p=0.01). In 11 cases showing the progression of the OPLL, the mean size of OPLL progression was 4.16 mm (range, 0.34–18.87 mm) in the longitudinal height and 1.57 mm (range, 0.54–3.91 mm) in thickness.
Conclusion
The progression of OPLL after cervical TDR was more frequent in patients with pre-existing OPLL than in patients without OPLL. Even though TDR is a major alternative to the treatment of cervical lesions to preserve vertebral segmental motion, careful attention should be paid to whether TDR should be used in patients with OPLL and this should be fully explained to the patient.
Go to :

Keywords: Cervical vertebrae, Total disc replacement, Ossification of posterior longitudinal ligament, Disease Progression
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) or anterior corpectomy and fusion (ACF) were commonly performed anterior approaching techniques in patients with cervical diseases including disc herniation, spondylosis, or ossification of the posterior longitudinal ligament (OPLL). However, these methods limit the range of neck motions postoperatively, and cervical total disc replacement (TDR) could be a good alternative option for treating cervical diseases causing cervical radiculopathy or myelopathy. Recently, TDR surgery with preserving the motion of the cervical spine while removing the lesion is frequently performed in patients with cervical disc herniations, especially when they are young. If the preoperative cervical computed tomography (CT) images showed ossification of cervical spine (i.e. bony spur, osteophytes or OPLL), TDR is relatively contraindicated. However, in clinical settings, surgeons have difficulties to decide the surgical techniques when patients have “small OPLLs or scant bony spurs.” Moreover, no literature has reported on the progression of OPLL in patients diagnosed with cervical disc herniation and OPLL after cervical TDR due to its rare prevalence.
The purpose of this study was to assess the degree of OPLL progression after cervical TDR and to understand the tendency for OPLL progression to be seen under certain conditions. To our knowledge, this study is the first study to investigate the relationship between OPLL and TDR.
Go to :

MATERIALS AND METHODS
Patient enrollment and classification
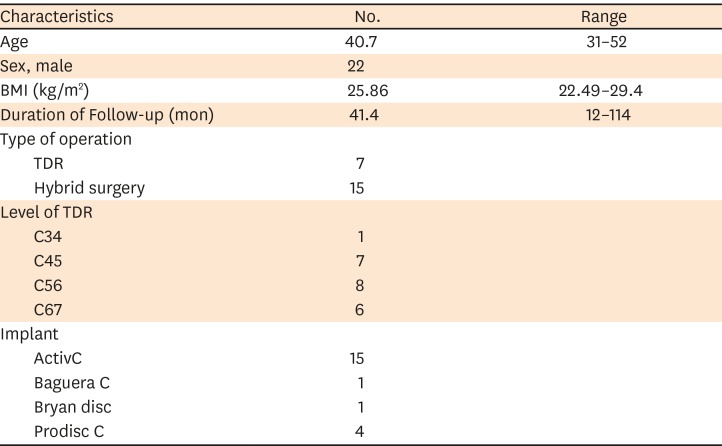
This study was approved by the Institutional Review Board of The Armed Forces Capital Hospital (AFCH-19-IRB-027). This study is retrospective study, IRB approve a waiver to informed consent. We retrospectively reviewed 33 patients who received cervical TDR alone or with anterior cervical fusion surgery from September 2009 through November 2016 at our institution. Among them, 11 patients were excluded because they were followed up for less than 12 months, and totally 22 patients were enrolled. All enrolled patients had the single- or two-level cervical soft disc herniation causing radiculopathy or myelopathy. The indications for TDR in our institution are that 1) the affected segment motion between cervical flexion and extension is well maintained for more than 5° on flexion and extension X-ray scans, 2) the OPLL does not occupy disc space in the manner of the continuous-type of OPLL, and 3) thecal sac compression due to OPLL is minimal. General demographics including age, sex, body mass index (BMI), comorbidities including smoking history and CT features of OPLL were collected. The enrolled patients were classified by 2 methods according to 1) pre-existing OPLL and 2) progression of OPLL (
FIGURE 1).
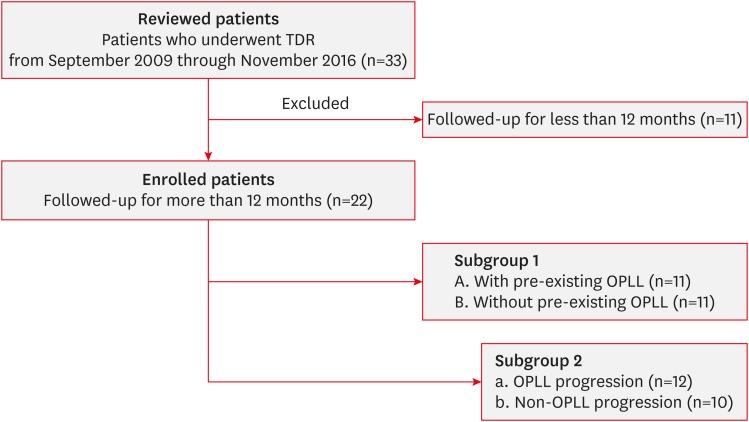 | FIGURE 1
Flow chart for the selection of relevant patients.
TDR: total disc replacement, OPLL: ossification of the posterior longitudinal ligament.

|
Surgical procedures
The surgical indications for TDR in our institution are that 1) the affected segment motion between cervical flexion and extension is well maintained for more than 5° on flexion and extension X-ray scans, 2) the OPLL does not occupy disc space in the manner of the continuous-type of OPLL, and 3) thecal sac compression due to OPLL is minimal (
FIGURE 2). In order to define the correct indication criteria for selecting ACDF or TDR in multilevel herniated disc disease, several factors were considered before surgery as followed; 1) Presence of motion on preoperative dynamic X-rays. In the case of no motion at the target level, 2) Radiographic signs of instability (translational instability of more than 2 mm, angular motion more than 11 degrees greater); 3) Advanced vertebral body spondylosis and/or facet degeneration on preoperative X-ray and CT scan; ACDF was performed.
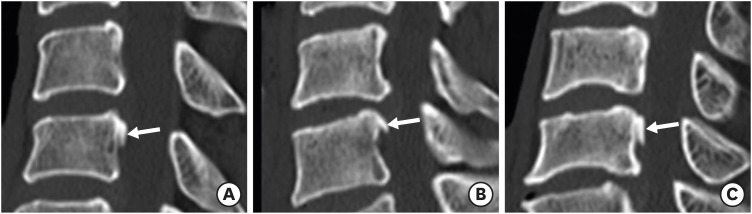
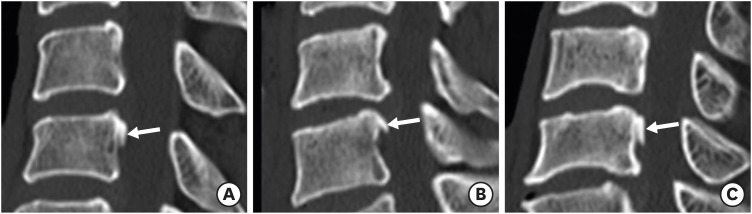 | FIGURE 2
Sagittal plane of preoperative cervical spine CT scan: Three patients had the cervical disc herniation and minimal segmental-type OPLL (arrow) (A-C). They showed the progression of the OPLL at the latest CT scan after TDR surgery.
CT: computed tomography, OPLL: ossification of the posterior longitudinal ligament, TDR: total disc replacement.

|
TDR was performed with usual Smith-Robinson approach. The symptomatic disc was removed, and then osteophyte or the posterior longitudinal ligament was removed sufficiently. After discectomy, a cervical disc prosthesis was implanted into intervertebral space. Bryan Disc (Medtronic Sofamor Danek USA Inc., Memphis, TN, USA), ActivC intervertebral disc prosthesis (B. Braun Melsungen AG, Melsungen, Germany), Baguera C cervical prosthesis (Spineart SA, Geneva, Switzerland) and the prodisc C (Centinel Spine Inc., West Chester, PA, USA) were used. In 15 patients with adjacent segment fusion, a polyetheretherketone cage filled with an allograft cancellous bone chip for fusion, was inserted into the disc space, and fixed with a plate and screws (Skyline Anterior Cervical Plate System, DePuy Synthes, Raynham, MA, USA).
Radiologic evaluations
The CT scan data for all the patients were analyzed by two neurosurgeons including the level of the involved segments, radiologic feature of OPLL, and its progression. OPLL was defined as the presence of a thin radio-opaque structure between the vertebral body and the ossified posterior ligament in the CT imaging, and also defined as the central position within the spinal canal in the axial image and distinguished from the bony prominence. Based on the classification of the Investigation Committee on OPLL of the Japanese Ministry of Public Health and Welfare, the OPLL types were classified as segmental, continuous, or mixed.
15)
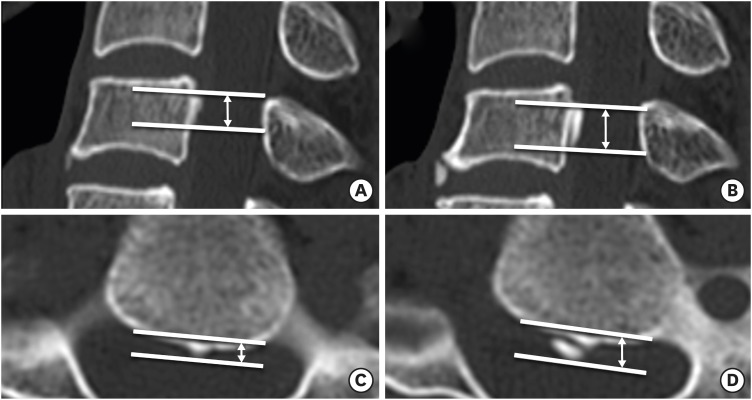
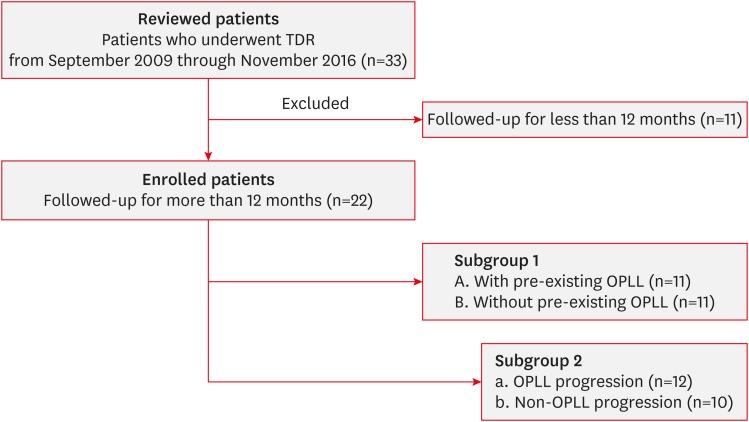
The progression of the OPLL mass on the CT scans was compared between the immediate postoperative CT scan and the latest CT scan. We evaluated “height” and “thickness” of OPLL by measuring the mass size horizontally in the thickest area from the vertebral body to the OPLL mass on the axial plane, and longitudinally based on the longest distance between the proximal and distal margins of the OPLL mass on the sagittal plane, respectively
36) (
FIGURE 3). The OPLL mass was distinguished from osteophyte that forms along the margin of the intervertebral space. The “progression of the OPLL” was defined when the ossification newly occurred in OPLL-free spines or the size of OPLL mass was increased. When progression of the OPLL mass was noted, the authors additionally evaluated the direction of the progression; toward the TDR level, fusion level, and the adjacent segment level without the TDR or ACDF. All radiologic measurements were conducted using the institution's picture archiving and communication system (PACS; M-view; INFINITT Healthcare Co. Ltd., Seoul, Korea).
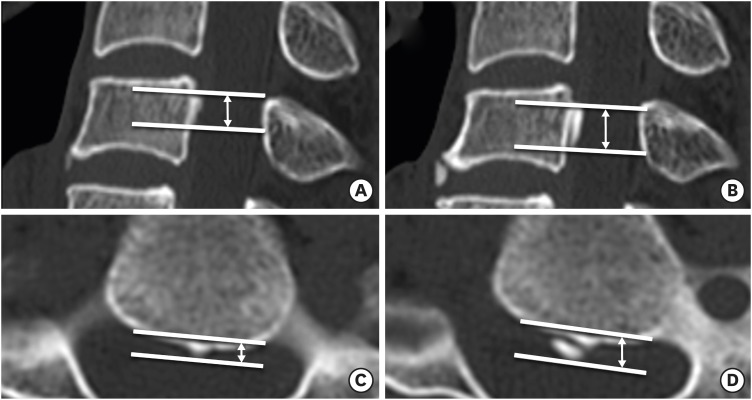 | FIGURE 3
Immediate postoperative sagittal and axial computed tomography images of a 39-year-old male underwent a total disc replacement at C5-C6 illustrating the method of measuring the size of OPLL mass longitudinally (A) and horizontally (B). After 61 months postoperatively, the OPLL masses progressed (C and D).
OPLL: ossification of the posterior longitudinal ligament.

|
Statistical analysis
Statistical analysis was performed with SPSS software (version 21.0; IBM Corp., Armonk, NY, USA). Continuous variables were expressed with mean and standard deviations and categorical variables were expressed with numbers and percentages. The independent t-tests were run on continuous variables and χ2 on categorical variables to compare the groups. When more than 20% of the cells in the χ2 had an expected frequency less than 5, the likelihood ratio was used. The statistical significance was defined as p<0.05.
Go to :

RESULTS
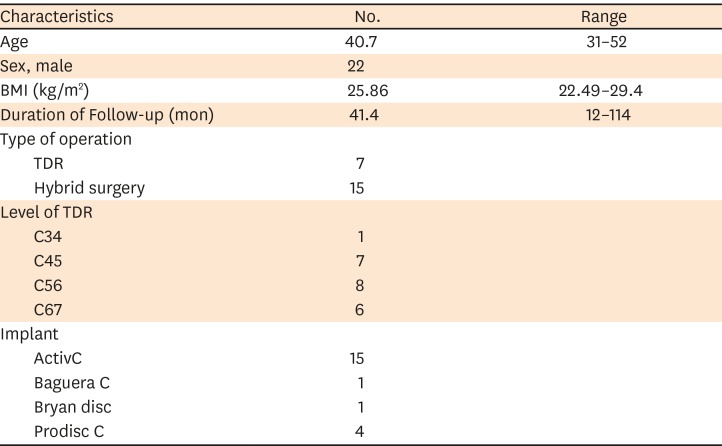
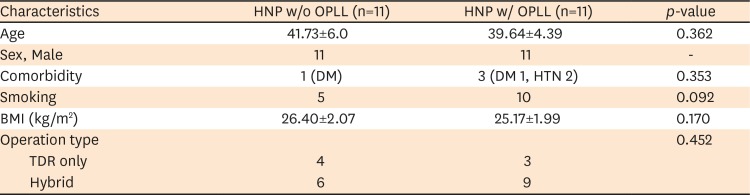
Twenty-two men were included in the analysis. The mean follow-up period from the surgery was 41.4 months (range, 12–114 months). All patients were male and military soldiers. The mean age of all patients was 40.7 years (range, 31–52 years), and the mean BMI was 25.86 kg/m
2 (range, 22.49–29.40 kg/m
2). TDR-only was used in 7 cases, and the hybrid surgery (TDR+ACDF) was used in 15 cases. According to the level of TDR insertion, C3-C4 in one case, C4-C5 in 7 cases, C5-C6 in 8 cases, and C6-C7 in 6 cases were performed. The cervical disc prosthetics used in the TDR surgery were as follows: a single case using Bryan Disc, a single case using Baguera C, 5 cases of prodisc C and 15 cases of Activ C (
TABLE 1).
TABLE 1
Demographic characteristics of the patients
|
Characteristics |
No. |
Range |
|
Age |
40.7 |
31–52 |
|
Sex, male |
22 |
|
|
BMI (kg/m2) |
25.86 |
22.49–29.4 |
|
Duration of Follow-up (mon) |
41.4 |
12–114 |
|
Type of operation |
|
|
|
TDR |
7 |
|
|
Hybrid surgery |
15 |
|
|
Level of TDR |
|
|
|
C34 |
1 |
|
|
C45 |
7 |
|
|
C56 |
8 |
|
|
C67 |
6 |
|
|
Implant |
|
|
|
ActivC |
15 |
|
|
Baguera C |
1 |
|
|
Bryan disc |
1 |
|
|
Prodisc C |
4 |
|

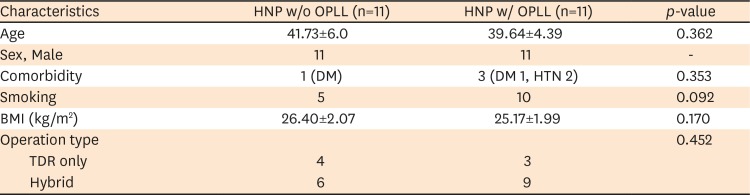
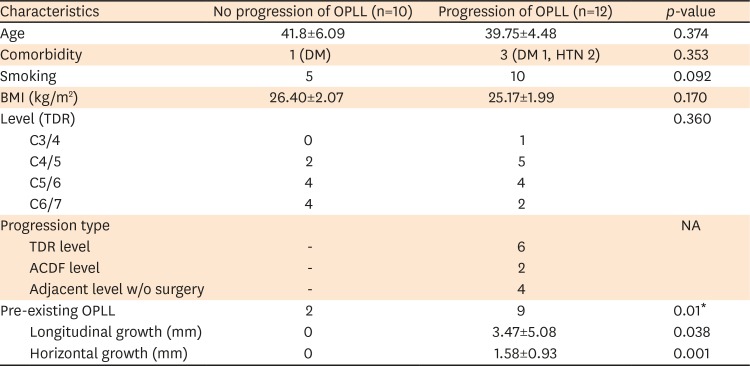
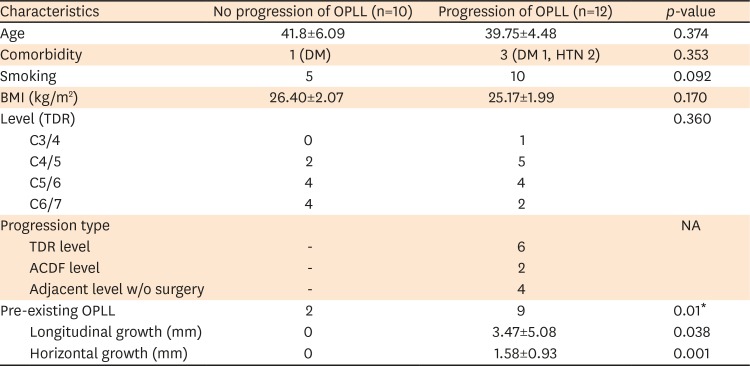
Among them, 11 patients have pre-existing small OPLLs, all the segmental type, on the preoperative CT scan. The detailed features of pre-existing OPLL were shown in
TABLE 2. The results of the statistical analysis comparing the patients with pre-existing OPLL and without were presented in
TABLE 3. The incidence of progression or newly development of OPLL was significantly higher in pre-existing OPLL group (
p=0.01). Also, monthly growth rate of longitudinal height and thickness of OPLL showed higher significance in pre-existing OPLL group (
p=0.04 and
p=0.01, respectively). In 11 cases showing the progression of the OPLL, the mean size of OPLL progression was 4.16 mm (range, 0.34–18.87 mm) in the longitudinal axis and 1.57 mm (range, 0.54–3.91 mm) in horizontal axis. According to the direction of the progression of the OPLL mass, two cases showed progression to the ACDF level, 6 cases to the TDR level, and 4 cases to the adjacent level where no operation was performed.
TABLE 2
Detailed features of pre-existing OPLL
|
Characteristics |
HNP w/o OPLL (n=11) |
HNP w/ OPLL (n=11) |
p-value |
|
Age |
41.73±6.0 |
39.64±4.39 |
0.362 |
|
Sex, Male |
11 |
11 |
- |
|
Comorbidity |
1 (DM) |
3 (DM 1, HTN 2) |
0.353 |
|
Smoking |
5 |
10 |
0.092 |
|
BMI (kg/m2) |
26.40±2.07 |
25.17±1.99 |
0.170 |
|
Operation type |
|
|
0.452 |
|
TDR only |
4 |
3 |
|
Hybrid |
6 |
9 |

TABLE 3
Results of the statistical analysis comparing the patients with pre-existing OPLL and without were presented
|
Characteristics |
No progression of OPLL (n=10) |
Progression of OPLL (n=12) |
p-value |
|
Age |
41.8±6.09 |
39.75±4.48 |
0.374 |
|
Comorbidity |
1 (DM) |
3 (DM 1, HTN 2) |
0.353 |
|
Smoking |
5 |
10 |
0.092 |
|
BMI (kg/m2) |
26.40±2.07 |
25.17±1.99 |
0.170 |
|
Level (TDR) |
|
|
0.360 |
|
C3/4 |
0 |
1 |
|
C4/5 |
2 |
5 |
|
C5/6 |
4 |
4 |
|
C6/7 |
4 |
2 |
|
Progression type |
|
|
NA |
|
TDR level |
- |
6 |
|
ACDF level |
- |
2 |
|
Adjacent level w/o surgery |
- |
4 |
|
Pre-existing OPLL |
2 |
9 |
0.01*
|
|
Longitudinal growth (mm) |
0 |
3.47±5.08 |
0.038 |
|
Horizontal growth (mm) |
0 |
1.58±0.93 |
0.001 |

However, there was no significant difference in OPLL progression according to surgery types (TDR-only and hybrid surgery, TDR+ACDF) (p=0.546). Smoking, BMI, and comorbidity did not affect the progression of OPLL; one patient underwent reoperation due to implant migration and one patient underwent additional fusion surgery due to adjacent segment disease.
Go to :

DISCUSSION
The current study reveals that the increase of OPLL size was significantly higher in patient with pre-existing OPLL group. Also, we could identify that pre-existence of OPLL was significantly higher in OPLL progression patients. Overall, we could suspect that there might be an association between pre-existing OPLL and its progression.
OPLL is a pathologic condition that can lead to spinal cord compression and neurological complications.
10) The prevalence of OPLL is higher in East Asians, including Koreans, Japanese, and Taiwanese, than in Caucasian populations.
111316) In Korean male patients, the prevalence rate of cervical OPLL was 163.3 per 100,000 people.
12) OPLL progression has been shown on radiographic observation in about 40%–60% of all cases. Progression is either to the cranial or caudal side, and inward to the canal side. Several factors can influence the progression to a higher rate, including age (under 40 years old), type of OPLL, and excessive cervical range of motion.
145) Also, some studies suggest that bone markers and systemic factors have been associated with the progression of OPLL.
714) Among the various factors, the authors sought to understand how conserving the movement affected the progression or development of OPLL by conducting studies using TDR. There were some studies that suggested a motion-related progression of the OPLL after surgery that does not involve fusion, including laminoplasty or laminectomy alone. Lee et al.
8) reported that the incidence of progression accounted for 45.5% in the laminoplasty group, 62.5% in the laminectomy alone group, and 30.0% in the laminectomy and fusion group. Chiba et al.
1) reported the rate of progression of OPLL at 56.5% after posterior decompression, after more than a 2-year follow-up period. Moreover, Hori et al.
5) reported progression of OPLL in 71% of participants after laminoplasty, after more than a 10-year follow-up period. These reports, however, have studied the phenomenon seen in the posterior approach, which limits the understanding of the relevance of the anterior approach.
Interestingly, our series showed that progression of OPLL occurred more frequently at the level of TDR (n=6) and an adjacent segment (n=2) than the level of ACDF (n=2). These results suggest that preserving motion may have a greater impact on the development or progression of OPLL than union does. The TDR surgery for cervical diseases acted as a risk factor for the progression of OPLL in the case of pre-existing OPLL before the surgery.
TDR was considered for younger patients and especially for patients with special tasks such as soldiers, where the limitation of movement of the vertebral joints could have a major impact on their performance if there was no other contraindication of TDR. Although the authors performed the cervical TDR for cervical disc herniation in patients with relatively minimal sized and only segmental-type OPLL, significant results were shown in that the prevalence and change in the size of the OPLL progression were higher in OPLL group than in the non-OPLL group (
p<0.05). Therefore, our study cautiously suggests that surgeons should think carefully about whether to apply the surgical method to preserve motion if OPLL is present, even though the OPLL may not be severe. Some studies report that the incidence of heterotopic ossification was more frequently observed after cervical TDR.
29) Other reports have noted that postoperative OPLL progressions were higher in the continuous-type and mixed-type of OPLL.
14)
This study has some limitations. The authors could not evaluate certain clinical information, such as the Japanese Orthopedic Association (JOA) scoring system and the visual analogue scale (VAS) due to a lack of questionnaires about the clinical results, since this was a retrospective case series study. However, no patient had undergone additional decompressive surgery due to OPLL progression, so the results of the progression of OPLL could not be ascertained until clinical impairment due to OPLL progression.
Go to :

CONCLUSION
The progression of OPLL after cervical TDR was more frequent in patients with pre-existing OPLL than in patients without OPLL. Additionally, the direction of progression occurred more at the motion-preserving level than at the fusion level. Even though TDR is a major alternative to the treatment of cervical lesions to preserve vertebral segmental motion, careful attention should be paid to whether TDR should be used in patients with OPLL and this should be fully explained to the patient.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download