1. Bortolotti A, Bernardini B, Colli E, Di Benedetto P, Giocoli Nacci G, Landoni M, et al. Prevalence and risk factors for urinary incontinence in Italy. Eur Urol. 2000; 37:30–35. PMID:
10671782.

2. Yarnell JW, Voyle GJ, Sweetnam PM, Milbank J, Richards CJ, Stephenson TP. Factors associated with urinary incontinence in women. J Epidemiol Community Health. 1982; 36:58–63. PMID:
7069357.

3. Cummings JM, Rodning CB. Urinary stress incontinence among obese women: review of pathophysiology therapy. Int Urogynecol J Pelvic Floor Dysfunct. 2000; 11:41–44. PMID:
10738933.

4. Mommsen S, Foldspang A. Body mass index and adult female urinary incontinence. World J Urol. 1994; 12:319–322. PMID:
7881469.

5. Rafii A, Daraï E, Haab F, Samain E, Levardon M, Deval B. Body mass index and outcome of tension-free vaginal tape. Eur Urol. 2003; 43:288–292. PMID:
12600433.

6. Whitcomb EL, Subak LL. Effect of weight loss on urinary incontinence in women. Open Access J Urol. 2011; 3:123–132. PMID:
24198645.

7. Morgan DM, Lewicky-Gaupp C, Dunn RL, Jayaraman G, Fenner DE, Delancey JO, et al. Factors associated with urge urinary incontinence after surgery for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2011; 17:120–124. PMID:
22453782.

8. Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993; 47:497–499. PMID:
8120507.

9. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996; 7:81–85. discussion 85–6. PMID:
8798092.

10. Ulmsten U, Falconer C, Johnson P, Jomaa M, Lannér L, Nilsson CG, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998; 9:210–213. PMID:
9795826.

11. Delorme E. [Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women]. Prog Urol. 2001; 11:1306–1313. French. PMID:
11859672.
12. Mellier G, Benayed B, Bretones S, Pasquier JC. Suburethral tape via the obturator route: is the TOT a simplification of the TVT? Int Urogynecol J Pelvic Floor Dysfunct. 2004; 15:227–232. PMID:
15517665.

13. Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008; 112:1253–1261. PMID:
19037033.

14. Guerette NL, Bena JF, Davila GW. Transobturator slings for stress incontinence: using urodynamic parameters to predict outcomes. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:97–102. PMID:
17549430.

15. Dmochowski RR, Blaivas JM, Gormley EA, Juma S, Karram MM, Lightner DJ, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010; 183:1906–1914. PMID:
20303102.

16. Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. EAU guidelines on urinary incontinence. Eur Urol. 2011; 59:387–400. PMID:
21130559.

17. Lee KS, Choo MS, Doo CK, Han DH, Lee YS, Kim JY, et al. The long term (5-years) objective TVT success rate does not depend on predictive factors at multivariate analysis: a multicentre retrospective study. Eur Urol. 2008; 53:176–182. PMID:
17825478.
18. Smith AL, Karp DR, Aguilar VC, Davila GW. Repeat versus primary slings in patients with intrinsic sphincter deficiency. Int Urogynecol J. 2013; 24:963–968. PMID:
23096532.

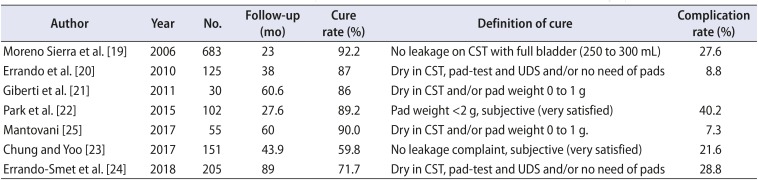
19. Moreno Sierra J, Marqués Queimadelos A, Araño Beltran P, De La Fuente Pérez P, Cerezuela Requena JF, Cortés Otero E, et al. [Spanish registry of the TRT Reemex system in women with stress urinary incontinence (SUI)]. Arch Esp Urol. 2006; 59:169–174. Spanish. PMID:
16649522.
20. Errando C, Rodriguez-Escovar F, Gutierrez C, Baez C, Araño P, Villavicencio H. A re-adjustable sling for female recurrent stress incontinence and sphincteric deficiency: Outcomes and complications in 125 patients using the Remeex sling system. Neurourol Urodyn. 2010; 29:1429–1432. PMID:
20127837.
21. Giberti C, Gallo F, Cortese P, Schenone M. The suburethral tension adjustable sling (REMEEX system) in the treatment of female urinary incontinence due to ‘true’ intrinsic sphincter deficiency: results after 5 years of mean follow-up. BJU Int. 2011; 108:1140–1144. PMID:
21554527.

22. Park BH, Kim JC, Kim HW, Kim YH, Choi JB, Lee DH. Midterm efficacy and complications of readjustable midurethral sling (Remeex system) in female stress urinary incontinence with recurrence or intrinsic sphincter deficiency. Urology. 2015; 85:79–84. PMID:
25530367.
23. Chung JW, Yoo ES. Efficacy and safety of a readjustable midurethral sling (Remeex system) for stress urinary incontinence with female voiding dysfunction. Investig Clin Urol. 2017; 58:127–133.

24. Errando-Smet C, Ruiz CG, Bertrán PA, Mavrich HV. A readjustable sling for female recurrent stress incontinence and intrinsic sphincteric deficiency: long-term results in 205 patients using the Remeex sling system. Neurourol Urodyn. 2018; 37:1349–1355. PMID:
29130569.
25. Mantovani F. ReMeEx device (External Mechanical Regulator) for female stress urinary incontinence: a critical review of a single-operator, long-term experience on implants and readjustments. Urologia. 2017; 84:102–105. PMID:
28315496.

26. Noblett KL, Jensen JK, Ostergard DR. The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. Int Urogynecol J Pelvic Floor Dysfunct. 1997; 8:323–326. PMID:
9609328.

27. Brieger G, Korda A. The effect of obesity on the outcome of successful surgery for genuine stress incontinence. Aust N Z J Obstet Gynaecol. 1992; 32:71–72. PMID:
1586341.

28. Dwyer PL, Lee ET, Hay DM. Obesity and urinary incontinence in women. Br J Obstet Gynaecol. 1988; 95:91–96. PMID:
3342213.

29. Killingsworth LB, Wheeler TL 2nd, Burgio KL, Martirosian TE, Redden DT, Richter HE. One-year outcomes of tensionfree vaginal tape (TVT) mid-urethral slings in overweight and obese women. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:1103–1108. PMID:
19448965.

30. Brennand EA, Tang S, Williamson T, Birch C, Murphy M, Robert M, et al. Calgary Women's Pelvic Health Research Group. Twelve-month outcomes following midurethral sling procedures for stress incontinence: impact of obesity. BJOG. 2015; 122:1705–1712. PMID:
25316484.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download