This article has been
cited by other articles in ScienceCentral.
Dual antiplatelet therapy (DAPT) with aspirin and P2Y
12 receptor inhibitor is the standard treatment in patients with acute coronary syndrome (ACS) or undergoing percutaneous coronary intervention (PCI).
1) The availability of different P2Y
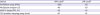
12 receptor inhibitors (clopidogrel, prasugrel and ticagrelor) with different levels of antiplatelet potency has enabled physicians to adopt individualized antiplatelet treatment. In addition, the development of point-of-care platelet function testing (PFT) to measure platelet reactivity to adenosine diphosphate can be fit for use in clinical practice. Like the therapeutic range of international normalized ratio (between 2 and 3) during warfarin treatment, consensus and clinical studies have suggested the therapeutic range of platelet reactivity during P2Y
12 inhibitor by applying uniform cutoff values of high- and low-platelet reactivity (HPR and LPR) (
Table 1).
1) In the near future, a tailored DAPT approach guided by PFT (escalation or de-escalation) may be an important way to precision medicine.
Available PFTs can be classified as point-of-care assays (VerifyNow, Multiplate, thromboelastography) and laboratory-based methods (light transmission aggregometry, vasodilator-stimulated phosphoprotein).
1) The point-of-care assays would be preferred in terms of practical aspect, but selection of assays needs to depend on their availability and local site experience. Although simple application with consensus-defined cutoffs of HPR/LPR can be a practical guide for tailored antiplatelet treatment, confirmative clinical evidences are required to strengthen the concept of a therapeutic window in PCI-treated patients. The cutoffs for HPR/LPR can be changed according to the clinical setting (stable angina vs. ACS), the phase of the disease entity (early vs. late phase), the complexity of PCI (simple vs. complex PCI) and the risk for bleeding complications. Of importance, how to adjust antiplatelet regimen in high-risk patients out of the therapeutic window may affect the consequent clinical outcomes remains to be verified. In addition, the optimal timing of PFT to predict post-PCI events remains a topic of debate. Although single measurements of on-treatment platelet reactivity have been conducted in most of previous clinical studies, its clinical usefulness may be questionable.
1) Patients' phenotype of HPR and LPR may change over time since influencing factors are subject to change over time.
2)3)4)5)
In this edition of the
Korean Circulation Journal, Yun et al.
5) have published their study to evaluate the variability of platelet reactivity over time in ACS patients treated with PCI (n=198) during clopidogrel or ticagrelor administration. Platelet reactivity was measured using multiple electrode platelet aggregometry (Multiplate analyzer; Roche Diagnostic GmbH, Mannheim, Germany), in which HPR was defined as ≥47 U, and LPR was defined as ≤18 U.
1) Platelet reactivity in the clopidogrel group increased over time (38.2±21.7 U at 48 hours vs. 44.7±25.5 U at 6 months; p=0.018), whereas this value in the ticagrelor group was not significantly changed (21.4±12.6 U at 48 hours vs. 22.8±13.8 U at 6 months; p=0.392). Between 48 hours and 6 months, 43% of patients changed their response status (HPR or normal response) in the clopidogrel group, and 13% in the ticagrelor group (p<0.001). They concluded that ticagrelor treatment resulted in less temporal variability of platelet reactivity than clopidogrel treatment in terms of HPR.
Although this study covers the important issue regarding tailored strategy of antiplatelet treatment, there are several important concerns to be pointed. Because the investigators did not evaluate the degree of drug adherence and change of concomitant medication over time, there would be the risks of unrecognized noncompliance and change in drug-drug interaction. In addition, they did not check time interval between last-dose administrations and blood sampling for measurement. The ONSET/OFFSET (Onset and Offset of Antiplatelet Effects Comparing Ticagrelor, Clopidogrel, and Placebo With Aspirin) study showed that platelet reactivity during P2Y
12 inhibitor administration can be variable over 8 hours after the last-dose administration, especially reversible-binding ticagrelor.
6) More importantly, the levels of platelet reactivity during the acute (at 48 hours) vs. chronic phase (at 6 months) can be different. In addition, the activity of disease entity (stable angina vs. ACS) and administered dose of study drug (loading vs. maintenance) could influence the level of platelet reactivity at the measuring point. Between 1 and 6 months, platelet reactivity on clopidogrel was not significantly changed (41.4±22.3 U vs. 44.7±25.5 U; p=0.256), and this value on ticagrelor did not differ significantly (20.0±12.2 U vs. 22.8±13.8 U; p=0.071) in the present study. Previous studies also showed the similar level of on-clopidogrel platelet reactivity and low prevalence of change in the response status (6.5–15.7%) during the chronic phase.
2)3)4)
Potent P2Y
12 inhibitors inevitably increased the risk of major bleeding in ACS patients, compared with clopidogrel.
7)8) Meanwhile, the antiplatelet effect on ticagrelor vs. prasugrel treatment appears greater in ACS patients.
9) Platelet reactivity at 30-day post-PCI in patients on ticagrelor was lower than those on prasugrel following acute myocardial infarction (21.1±26.1 vs. 67.3±62.5 P2Y12 reaction units measured by VerifyNow; p<0.001). In the present study, ticagrelor treatment almost abolished the risk of HPR, but more than 50% of the patients had LPR phenotype (≤18 U).
5) Absolute increase of non-CABG TIMI major bleeding (+0.6%) seemed similar between ticagrelor and prasugrel, compared with clopidogrel.
7)8) Compared with the short plasma exposure of thienopyridine (prasugrel and clopidogrel) active metabolites (up to 6 hours), ticagrelor has significant 24-hour systemic exposure of a direct active compound (reversible-binding property)
6); this unique profile of ticagrelor may be characterized by its fast and strong platelet inhibition with a wider therapeutic window (
Figure 1). The dedicated clinical studies to indicate the different cutoffs of LPR during thienopyridine or ticagrelor treatment are needed to guide the tailored strategy to target the therapeutic window of platelet reactivity.
Specific considerations may be warranted for East Asian patients, who have a different benefit/risk ratio compared with the Caucasian population.
1)10) During antithrombotic treatment, East Asian patients have shown a lower risk of atherothrombotic event and a higher tendency of bleeding; this phenomenon was first denominated in 2011 by Jeong and coinvestigators who developed the concept of “East Asian Paradox”, suggesting a different therapeutic targeting of antiplatelet effect in East Asian patients.
10) In East Asian population with ACS, reduced-dose ticagrelor and prasugrel may provide more acceptable clinical efficacy and safety comparing with standard-dose treatment, but there are no large-scale prospective studies to confirm the clinical benefit of this antiplatelet strategy.
The experience has accumulated over the past decade on studies of PFT and its use has been proposed as optional methods to aid clinical decision making in the selective scenarios.
1) Although the results of proof-of-concept studies made a guided choice of antiplatelet regimen attractive, the robustness of the evidence and limitations of “therapeutic window” concept based on PFT (e.g., temporal variability of platelet reactivity over time) still may not allow routine recommendation of PFT use in clinical practice. Nevertheless, escalation strategy may be required when thrombotic risk outweighs bleeding risk (e.g., clopidogrel treatment after complex PCI), whereas de-escalation strategy may be desired when bleeding risk outweighs thrombotic risk (e.g., chronic ticagrelor treatment in East Asian patients with ACS). The results of ongoing clinical trials will further fine-tune the personalized strategy of P2Y
12 inhibitor in high-risk patients undergoing PCI.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download