Abstract
Purpose
To report a case of pituitary apoplexy presenting as isolated bilateral oculomotor nerve palsy.
Case summary
A 46-year-old male presented with bilateral ptosis and acute severe headaches for 6 days. He underwent head surgery and bilateral vitrectomy 12 years prior to his visit because of ocular and head trauma. He mentioned that previous visual acuities in both eyes were not good. The initial corrected visual acuity was finger counting in the right eye and 20/500 in the left eye. Ocular motility testing revealed the limitation of adduction, supraduction, and infraduction with complete bilateral ptosis in both eyes, and his left pupil was dilated. He was diagnosed with an isolated bilateral oculomotor nerve palsy. Magnetic resonance imaging indicated pituitary gland hemorrhage with a tumor, which was suspicious of pituitary apoplexy. The patient was treated intravenous with 1.0 g methylprednisolone to prevent the corticotropic deficiency. In addition, he underwent surgical decompression using a navigation-guided transsphenoidal approach and aspiration biopsy. He was confirmed with pituitary adenoma using a pathological examination. The patient's ocular movements began to dramatically improve by the third day postoperatively. At 4 months postoperative follow-up, his ocular movement and double vision were completely recovered.
Figures and Tables
Figure 1
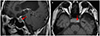
Nine cardinal gaze position at initial visit. Ocular movement was revealed the limitation of adduction, supraduction, and infraduction with complete ptosis in both eyes and a dilated pupil was shown in the left eye.

References
2. Hage R, Eshraghi SR, Oyesiku NM, et al. Third, fourth, and sixth cranial nerve palsies in pituitary apoplexy. World Neurosurg. 2016; 94:447–452.

3. Bills DC, Meyer FB, Laws ER Jr, et al. A retrospective analysis of pituitary apoplexy. Neurosurgery. 1993; 33:602–609.

4. Jeon HJ, Kang JH, Cho BM, et al. Clinical manifestations and surgical outcome of pituitary apoplexy. J Korean Brain Tumor Soc. 2008; 7:120–126.
5. Komurcu HF, Ayberk G, Ozveren MF, Anlar O. Pituitary adenoma apoplexy presenting with bilateral third nerve palsy and bilateral proptosis: a case report. Med Princ Pract. 2012; 21:285–287.

6. Man BL, Fu YP. Pituitary apoplexy presenting with bilateral oculomotor nerve palsy. BMJ Case Rep. 2015; 2015:Accessed Oct 15, 2015. https://casereports.bmj.com/content/2015/bcr-2015-212049.

7. Lau KK, Joshi SM, Ellamushi H, Afshar F. Isolated bilateral oculomotor nerve palsy in pituitary apoplexy: case report and review. Br J Neurosurg. 2007; 21:399–402.

8. Lee HG, Noh JS, Rhim JK, Chung BS. Isolated third cranial nerve palsy with ptosis presented in pituitary apoplexy: case report. J Korean Brain Tumor Soc. 2011; 10:20–21.
9. Yadegari S. Approach to a patient with blepheroptosis. Neuro Sci. 2016; 37:1589–1596.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download