1. Giordano SH, Elias AD, Gradishar WJ. NCCN guidelines updates: breast cancer. J Natl Compr Canc Netw. 2018; 16(5S):605–610. PMID:
29784737.

2. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003; 349:546–553. PMID:
12904519.

3. Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol. 2017; 35:561–564. PMID:
27937089.

4. Prendeville S, Ryan C, Feeley L, O'Connell F, Browne TJ, O'Sullivan MJ, et al. Sentinel lymph node biopsy is not warranted following a core needle biopsy diagnosis of ductal carcinoma in situ (DCIS) of the breast. Breast. 2015; 24:197–200. PMID:
25681861.

5. Sakr R, Bezu C, Raoust I, Antoine M, Ettore F, Darcourt J, et al. The sentinel lymph node procedure for patients with preoperative diagnosis of ductal carcinoma in situ: risk factors for unsuspected invasive disease and for metastatic sentinel lymph nodes. Int J Clin Pract. 2008; 62:1730–1735. PMID:
19143859.

6. Tan EY, Lo ZW, Ang CH, Teo C, Seah MD, Chen JJ, et al. Sentinel lymph node biopsy should be included with the initial surgery for high-risk ductal carcinoma-in-situ. Int Sch Res Notices. 2014; 2014:624185. PMID:
27379334.

7. Brennan ME, Turner RM, Ciatto S, Marinovich ML, French JR, Macaskill P, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011; 260:119–128. PMID:
21493791.

8. Sakr R, Antoine M, Barranger E, Dubernard G, Salem C, Daraï E, et al. Value of sentinel lymph node biopsy in breast ductal carcinoma in situ upstaged to invasive carcinoma. Breast J. 2008; 14:55–60. PMID:
18186866.

9. Coufal O, Selingerová I, Vrtělová P, Krsička P, Gabrielová L, Fabian P, et al. A simple model to assess the probability of invasion in ductal carcinoma in situ of the breast diagnosed by needle biopsy. Biomed Res Int. 2014; 2014:480840. PMID:
25114904.

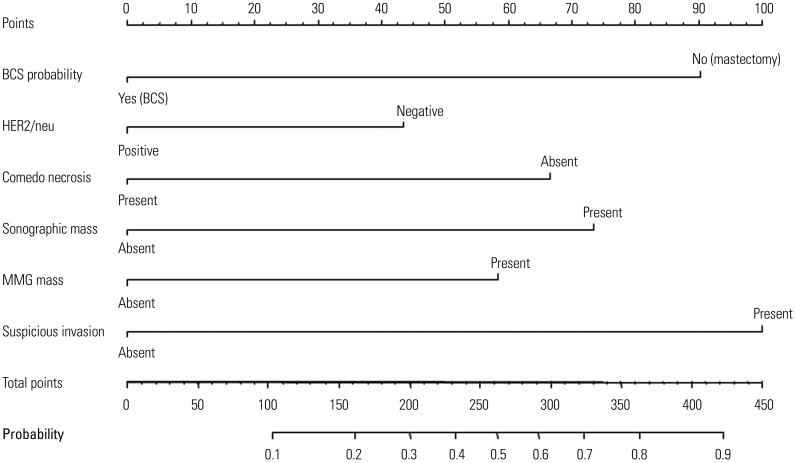
10. Park HS, Kim HY, Park S, Kim EK, Kim SI, Park BW. A nomogram for predicting underestimation of invasiveness in ductal carcinoma in situ diagnosed by preoperative needle biopsy. Breast. 2013; 22:869–873. PMID:
23601760.

11. Lee SK, Yang JH, Woo SY, Lee JE, Nam SJ. Nomogram for predicting invasion in patients with a preoperative diagnosis of ductal carcinoma in situ of the breast. Br J Surg. 2013; 100:1756–1763. PMID:
24227361.

12. Kondo T, Hayashi N, Ohde S, Yagata H, Yoshida A, Nakamura S, et al. A nomogram associated with high probability of invasive carcinoma on the surgical specimen in patients with preoperative diagnosis of ductal carcinoma in situ of the breast. J Clin Oncol. 2014; 32(15_Suppl):1595. PMID:
24752047.

13. Jakub JW, Murphy BL, Gonzalez AB, Conners AL, Henrichsen TL, Maimone S 4th, et al. A validated nomogram to predict upstaging of ductal carcinoma in situ to invasive disease. Ann Surg Oncol. 2017; 24:2915–2924. PMID:
28766196.

14. Meurs CJC, van Rosmalen J, Menke-Pluijmers MBE, Ter Braak BPM, de Munck L, Siesling S, et al. A prediction model for underestimation of invasive breast cancer after a biopsy diagnosis of ductal carcinoma in situ: based on 2892 biopsies and 589 invasive cancers. Br J Cancer. 2018; 119:1155–1162. PMID:
30327564.

15. Park HS, Park S, Cho J, Park JM, Kim SI, Park BW. Risk predictors of underestimation and the need for sentinel node biopsy in patients diagnosed with ductal carcinoma in situ by preoperative needle biopsy. J Surg Oncol. 2013; 107:388–392. PMID:
23007901.

16. Kang SY, Kim YS, Kim Z, Kim HY, Lee SK, Jung KW, et al. Basic findings regarding breast cancer in Korea in 2015: data from a breast cancer registry. J Breast Cancer. 2018; 21:1–10. PMID:
29628978.

17. Duffy SW, Dibden A, Michalopoulos D, Offman J, Parmar D, Jenkins J, et al. Screen detection of ductal carcinoma in situ and subsequent incidence of invasive interval breast cancers: a retrospective population-based study. Lancet Oncol. 2016; 17:109–114. PMID:
26655422.

18. Suh YJ, Kim MJ, Kim EK, Moon HJ, Kwak JY, Koo HR, et al. Comparison of the underestimation rate in cases with ductal carcinoma in situ at ultrasound-guided core biopsy: 14-gauge automated core-needle biopsy vs 8- or 11-gauge vacuum-assisted biopsy. Br J Radiol. 2012; 85:e349–e356. PMID:
22422382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download