1. Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998; 280(20):1747–1751.

2. Axelrod DA, Guidinger MK, McCullough KP, Leichtman AB, Punch JD, Merion RM. Association of center volume with outcome after liver and kidney transplantation. Am J Transplant. 2004; 4(6):920–927.

4. Glance LG, Li Y, Osler TM, Dick A, Mukamel DB. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med. 2006; 34(7):1925–1934.

5. Lin HC, Xirasagar S, Chen CH, Hwang YT. Physician's case volume of intensive care unit pneumonia admissions and in-hospital mortality. Am J Respir Crit Care Med. 2008; 177(9):989–994.

6. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15.

7. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139.

8. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36(1):8–27.

9. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47(6):626–633.

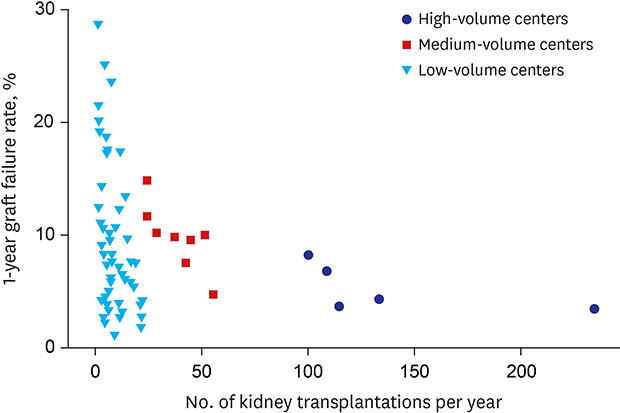
10. Barbas AS, Dib MJ, Rege AS, Vikraman DS, Sudan DL, Knechtle SJ, et al. The volume-outcome relationship in deceased donor kidney transplantation and implications for regionalization. Ann Surg. 2018; 267(6):1169–1172.

11. Tsao SY, Lee WC, Loong CC, Chen TJ, Chiu JH, Tai LC. High-surgical-volume hospitals associated with better quality and lower cost of kidney transplantation in Taiwan. J Chin Med Assoc. 2011; 74(1):22–27.

12. Schurman SJ, Stablein DM, Perlman SA, Warady BA. Center volume effects in pediatric renal transplantation. A report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol. 1999; 13(5):373–378.
13. Perl J, Zhang J, Gillespie B, Wikström B, Fort J, Hasegawa T, et al. Reduced survival and quality of life following return to dialysis after transplant failure: the Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant. 2012; 27(12):4464–4472.

14. Hamed MO, Chen Y, Pasea L, Watson CJ, Torpey N, Bradley JA, et al. Early graft loss after kidney transplantation: risk factors and consequences. Am J Transplant. 2015; 15(6):1632–1643.

15. Cho H, Yu H, Shin E, Kim YH, Park SK, Jo MW. Risk factors for graft failure and death following geriatric renal transplantation. PLoS One. 2016; 11(4):e0153410.

16. Richie RE, Niblack GD, Johnson HK, Green WF, MacDonell RC, Turner BI, et al. Factors influencing the outcome of kidney transplants. Ann Surg. 1983; 197(6):672–677.

17. Lepeytre F, Dahhou M, Zhang X, Boucquemont J, Sapir-Pichhadze R, Cardinal H, et al. Association of sex with risk of kidney graft failure differs by age. J Am Soc Nephrol. 2017; 28(10):3014–3023.

18. Chen YC, Jeng MJ, Lee YS, Lo YC, Tsao PC, Yang CF, et al. The relationship between physician case volume and in-hospital mortality of critically ill children with a diagnosis of pneumonia: a cross-sectional observational analytical study. J Crit Care. 2014; 29(6):1046–1051.

19. Dres M, Tran TC, Aegerter P, Rabbat A, Guidet B, Huchon G, et al. Influence of ICU case-volume on the management and hospital outcomes of acute exacerbations of chronic obstructive pulmonary disease. Crit Care Med. 2013; 41(8):1884–1892.

20. Morales JM, Marcén R, del Castillo D, Andres A, Gonzalez-Molina M, Oppenheimer F, et al. Risk factors for graft loss and mortality after renal transplantation according to recipient age: a prospective multicentre study. Nephrol Dial Transplant. 2012; 27(Suppl 4):iv39–iv46.

21. El-Agroudy AE, Bakr MA, Shehab El-Dein AB, Ghoneim MA. Death with functioning graft in living donor kidney transplantation: analysis of risk factors. Am J Nephrol. 2003; 23(3):186–193.

22. Farrugia D, Cheshire J, Begaj I, Khosla S, Ray D, Sharif A. Death within the first year after kidney transplantation--an observational cohort study. Transpl Int. 2014; 27(3):262–270.
23. Chkhotua AB, Klein T, Shabtai E, Yussim A, Bar-Nathan N, Shaharabani E, et al. Kidney transplantation from living-unrelated donors: comparison of outcome with living-related and cadaveric transplants under current immunosuppressive protocols. Urology. 2003; 62(6):1002–1006.

24. Centers for Medicare & Medicaid Services (CMS), Department of Health and Human Services (HHS). Medicare program; hospital conditions of participation: requirements for approval and re-approval of transplant centers to perform organ transplants. Final rule. Fed Regist. 2007; 72(61):15197–15280.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download