Abstract
Purpose
In the present study, the volume of hard exudates (HEs) was quantitatively measured using optical coherence tomography (OCT) and the agreement and correlation with area of HEs in fundus photography were analyzed.
Methods
The medical records of patients with diabetic macular edema who underwent focal laser treatment and were followed up more than 3 months were retrospectively evaluated. An automated customized program designed for measuring HE volume was used. The HEs in each OCT B-scan binary image were measured using 512 × 128 pixels, 6 mm × 6 mm OCT cube scans. The volume was measured by summing the segmented HEs in each 128 B-scan image. The area was measured in 6 mm x 6 mm fundus photography. The volume and area were measured before and 3 months after the treatment. The agreement of increase and decrease in HEs, and the correlation of volume and area of HEs were analyzed.
Results
A total of 35 patients (39 eyes) were included in the study. The volume was significantly reduced from 0.07978 to 0.02565 mm3 at 3 months (p < 0.001). The area was also significantly reduced from 15.35 to 8.60 mm2 at 3 months (p < 0.001). The volume was decreased in 34 eyes and increased in 5 eyes. The area was decreased in 37 eyes and increased in 2 eyes. A significant correlation between volume and area was found (p < 0.001) as well as agreement between increase and decrease in volume and area.
Conclusions
In the 3-dimensional quantitative volumetric analysis, the volume and area of HEs were correlated and the direction of increase and decrease was concordant. Considering the distribution of HEs in multiple layers of the retina, volumetric analysis could be considered a substitute for the analysis of HE area.
Diabetic retinopathy is a leading cause of legal blindness in developed countries, and diabetic macular edema (DME) is an important cause of visual impairment in diabetic individuals [12]. The most commonly used indicator of DME is central retinal thickness (CRT), which reflects the amount of accumulated fluid in the center of the fovea [3]. However, based on several reported cases, visual acuity deteriorates even when the CRT is in the normal range and visual acuity improves although CRT increases [4]. Various factors other than CRT are associated with visual acuity in patients with DME.
Hard exudates (HEs), which can be frequently observed with DME [5], are a special form of DME composed of lipoproteins from retinal microaneurysms and dilated capillaries. Accumulation of HEs in the fovea can cause degeneration of both photoreceptors and neurons, resulting in poor visual prognosis [67]. Thus, precise measurement of HEs is important for predicting prognosis or monitoring the results of DME treatment.
In previous studies, the analysis of HEs was performed with qualitative grading systems. The HE areas were classified as definite (>0 to 0.1 mm2), obvious (>0.1 to 0.5 mm2), moderate (>0.5 to 2.5 mm2), or severe (>2.5 mm2) using the Early Treatment Diabetic Retinopathy Study (ETDRS) classification based on a set of standard photographs [57]. However, this method should tolerate different categorizations depending on the judgment of the investigator. Recently, HEs were evaluated in 2-dimensional images using color fundus photography and quantitative data were obtained [89].
Because HEs are distributed in multiple layers of the retina, the authors hypothesized that volumetric evaluation of HEs might better reflect the actual amount. Herein, a new method for quantitative analysis of HEs using optical coherence tomography (OCT) is introduced. In the current study, the agreement and correlation between a new volumetric evaluation of HEs and conventional area analysis in color fundus photography were analyzed.
This was a retrospective, consecutive case series study. The medical records of patients with DME who underwent focal laser treatment were reviewed. All patients were treated between January 2015 and December 2017 and followed up for more than 3 months. The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the institutional review board of Haeundae Paik Hospital (2010-10-011). Written informed consent was waived due to the retrospective nature of the study.
Inclusion criteria were CRT ≥250 µm as measured using spectral domain OCT (SD-OCT; Cirrus OCT, Carl Zeiss Meditec, Dublin, CA, USA) and presence of HEs in the perifoveal area confirmed both on SD-OCT and color fundus photography (TRC-NW8, Topcon, Tokyo, Japan). Exclusion criteria were pan-retinal photocoagulation (PRP) within 6 months, previous history of focal or grid laser, and presence of other ophthalmologic diseases (e.g., age-related macular degeneration, epiretinal membrane, retinal vascular disease) that could affect the results. Focal laser treatment was performed with a modified ETDRS technique using burns that are lighter than originally specified in the ETDRS.
The following baseline characteristics were investigated: age, sex, duration of diabetes mellitus, glycated haemoglobin (HbA1c) level, previous history of PRP, intravitreal injections prior to laser treatment, and associated systemic diseases such as hypertension and hyperlipidemia. The volume and area of HEs were measured before and 3 months after the focal laser treatment. The CRT was measured at the fovea center using the built-in SD-OCT software.
The volume of HEs was measured using an automated customized program (Fig. 1A–1C). Using 512 × 128 pixels, 6 mm × 6 mm OCT cube scans, the HEs in each OCT B-scan binary image were measured (Fig. 1B). The retina was bounded by internal limiting membrane and retinal pigment epithelium (RPE), and the target HEs were measured by filtering the pixel signal using binarization. The threshold of binarization was set as a uniform cut-off value. The volume of HEs was measured by summing the segmented HEs in each 128 B-scan image (Fig. 1C).
The area of HEs was measured in 6 mm x 6 mm color fundus photography (Fig. 2A–2C) using ImageJ software (National Institutes of Health, Bethesda, MD, USA; http://rsb.info.nih.gov/ij) semi-automatically. Reference length was adopted from the corresponding OCT image scale. Fundus photography images were imported into ImageJ software and green channel image was used for the analysis. The binarization image was generated over the automatic threshold function of ImageJ. In this binarization image, pixels other than HEs, including vessel or optic disc, were manually eliminated by the examiner (H.R.K) after comparison with baseline fundus photography. Fovea was identified by overlaying the OCT fundus image. Then total area of HEs was measured.
The following were excluded from the present study due to poor quality: 1) poor clarity; 2) segmentation errors; 3) a local weak signal <7 in SD-OCT; and 4) inability to sort HEs from vessels, hemorrhages and background normal retina.
All the statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The Wilcoxon's signed rank test was used to evaluate the changes in area and volume of HEs before and 3 months after the treatment. The changes in HEs were categorized as increase or decrease. The cut-off value was 10% change from baseline to 3 months. The agreement of increase and decrease in volume and area was analyzed using McNemar's chi-square test. Spearman correlation coefficients were used to analyze the correlation between the volume and area using baseline and 3-month data. Multiple regression analysis was performed to investigate the factors predicting the reduction of HEs. Univariate regression analysis was used for continuous variables, logistic regression analysis was used for categorical variables, and multiple regression analysis was performed by selecting only variables with a p-value <0.20. For others, p < 0.05 was considered statistically significant.
A total of 39 eyes of 35 patients were included in the study. The mean age was 58.4 ± 9.4 years and 48.6% (17 / 35) were male. The mean duration of diabetes mellitus was 11.1 ± 7.2 years, preoperative HbA1c was 8.2 ± 2.2%, and systemic hypertension was seen in 11 eyes and hyperlipidemia in 7 eyes. The best-corrected visual acuity (logarithm of the minimum angle of resolution) was 0.27 ± 0.33 and the mean CRT was 292.4 ± 52.1 µm. The baseline characteristics are summarized in Table 1.
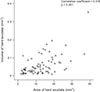
In the volumetric analysis, the HEs decreased significantly from 0.07978 to 0.02565 mm3 at 3 months (p < 0.001). In the area analysis, the HEs also decreased significantly from 15.35 to 8.60 mm2 at 3 months (p < 0.001). From baseline to 3 months, the volume of HEs was decreased in 34 eyes and increased in five eyes. The area of HEs was decreased in 37 eyes and increased in two eyes. The agreement of increase and decrease in volume and area was concordant (p = 0.248, McNemar's chi-square test). The volumetric analysis showed a positive predictive value of 40% and a negative predictive value of 100%. The sensitivity and specificity were 100% and 91.9%, respectively. The volume was correlated with area with moderate strength (correlation coefficient = 0.516, p < 0.001) (Fig. 3).
Three cases showed discrepancy in the measurements of HEs; decrease in area and increase in volume. In two cases, increase of HEs in the outer retina was noted (Fig. 4A–4F). In the other case, HEs were indistinct in the fundus photography. In addition, hyperreflective materials suspected as HEs, were detected on OCT (Fig. 5A, 5B).
Based on a multiple regression logistic test, significant decrease of HEs at 3 months after the treatment was correlated with more extensive volume of baseline HEs (p < 0.001, R2 = 0.791). Age, sex, prior intravitreal injection, anticipatory PRP, duration of diabetes mellitus, and presence of hyperlipidemia or hypertension did not affect the decrease in HEs.
In the current study, a new method for quantitative volume analysis of HEs using SD-OCT was introduced. The volume of HEs significantly correlated with conventional area of HEs, and the direction of increase and decrease was concordant. However, in some cases, discrepancy between the volume and area analysis was observed.
In previous studies, the usefulness of OCT as a diagnostic tool and staging marker of diabetic retinopathy has been reported [1011]. Specifically, OCT can detect early changes of HEs [11]. In addition to earlier detection of HEs, the authors of the present study hypothesized the accurate measurement of HEs as a potential prognostic indicator of diabetic retinopathy can be performed using OCT, and developed a customized program to measure hyperreflective materials on OCT.
Hyperreflective foci, first described by Bolz et al. [12], are considered lipid extravasations acting as subclinical HEs [131415]. Niu et al. [13] proposed that large hyperreflective foci form confluent deposits in the outer retina and appear clinically as HEs on color fundus photography. Thus, the hyperreflective materials on OCT scans might reflect the amount of HEs, although other hyperreflective materials not associated with HEs are of concern. Small hyperreflective foci might represent aggregates of activated microglial cells or migrated RPE cells [131617], hence interfering with the measurement of HEs. When designing this study, we considered this problem, however, technically discriminating migrated RPEs from HEs was difficult. Most hyperreflective foci are considered precursors of HEs in patients with diabetic retinopathy [13], and migrated RPE cells are frequently observed in patients with age-related macular degeneration [17]. To minimize the influence of migrated RPE cells, only DME patients were enrolled in the present study.
The cut-off value for binarization was another issue because a different value could significantly affect the results, thus, a uniform cut-off value was determined for OCT images. The OCT scan is originally a monochromatic image and has an automatic function to adjust the overall contrast. After comparing more than 100 cases, the most appropriate threshold was determined that did not misinterpret other retinal tissues as HEs. The uniform cut-off value provided consistent results throughout program development. However, in fundus photographs, each photograph varies in white balance and contrast resulting from exposure to the light, and even brightness of the posterior pole and the peripheral retina differs in the same image. Therefore, the uniform cut-off value was not appropriate for the estimation of fundus photographs. Instead, the auto-threshold function of ImageJ and manual elimination of noise signal (e.g., retinal vessels, hemorrhages, retinal nerve fibers) were used for precise measurements. In addition, this method has shown relatively consistent results in previous studies [78].
The agreement and correlation between the area and volume showed relatively good results. However, three cases showed disagreement between the volume and area of HEs. There are two possible reasons for this disagreement. First, increased HEs in the outer retina may be the cause, as shown in Fig. 4. Distributional change in HEs has already been reported in a previous study. Pemp et al. [18] suggested the change in HE distribution after intravitreal injection of anti-vascular endothelial growth factor in DME subjects. Although their study included only patients treated with intravitreal injections, distributional change may occur in patients treated with a focal laser, resulting in discrepancy of area and volume. Second, the resolution of SD-OCT (1 to 10 µm) [13] is higher than color fundus photograph, rendering SD-OCT more favorable for detecting small amounts of HEs. In Fig. 5, HEs which were indistinct in fundus photography were detected on OCT. Davoudi et al. [19] previously reported hyperreflective foci on OCT and indistinct HEs, or any other pathology, in the corresponding area on fundus photographs.
When analyzing discrepant cases, the advantages of volumetric analysis over conventional area analysis were considered in the present study. HEs are distributed in 3-dimensional patterns because they are deposited in multiple layers of the retina. The 3-dimensional volume analysis is more likely to reflect the actual amounts of HEs than 2-dimensional area analysis. In addition, volume analysis can detect small amounts of HEs that are not obvious in fundus photography, although not because of volumetric analysis but the use of OCT.
Widely known predictors of visual prognosis of diabetic eyes include age, sex, duration of diabetes mellitus, baseline best corrected visual acuity, presence of subretinal fluid, presence of HEs, baseline CRT, glycemic variability (e.g., HbA1c), lipid/lipoprotein related complexes, and blood pressure [2021]. However, factors associated with the change in HEs in diabetic retinopathy have not been clarified. In the present study, the above-mentioned factors were not significantly associated with the change of HEs in both area and volume analyses. Further studies elucidating causal and influential factors of HEs are warranted.
The present study had several limitations including a small sample size and retrospective design. In addition, errors in measuring HEs in the fundus photographs may be caused by some lesions (e.g., blood vessels, cotton wool spots, and even normal retinal nerve fiber layer with similar reflectivity of HEs). Furthermore, hyperreflective materials observed on the OCT image were not always consistent with HEs, hindering the accuracy of the measurement. Finally, single measurements of HEs did not eliminate the interobserver variability, resulting in possible inaccuracies. Nevertheless, to the best of the authors' knowledge, this is the first report in which a new method of quantitative volumetric analysis of HEs was introduced.
In conclusion, the volume and area of HEs were significantly correlated and the agreement of increase and decrease was concordant. Considering the distribution of HEs in multiple layers of the retina, volumetric analysis could be considered a substitute for conventional area analysis.
Figures and Tables
 | Fig. 1Volumetric analysis of hard exudates. (A) Optical coherence tomography B-scan image before binarization. (B) Binary image of optical coherence tomography B-scan. (C) Summation of each 128 binary image to calculate the volume of hard exudates. |
 | Fig. 2Area analysis of hard exudates. (A) Fundus photography before binarization. (B) Binary image of fundus photograph. (C) Measurement of area within 6 × 6 mm image. |
 | Fig. 4Representative case of discrepancy between the volume and area of hard exudates. Color fundus photographs before (A) and after (B) the focal laser show decreased area of hard exudates. In the cross-sectional optical coherent tomography and optical coherent tomography binary images of the same location (sky-blue arrows), hard exudates (yellow arrows) were increased in the outer retina after focal laser (D,F) compared with baseline (C,E). |
 | Fig. 5Representative case of discrepancy between the volume and area of hard exudates. (A) In fundus photography, presence of hard exudates is not obvious (arrow). (B) On optical coherence tomography, hyperref lective materials (arrows), suspected as hard exudates, are visible in horizontal (top) and vertical (bottom) scans. |
References
1. Schachat AP, Wilkinson CP, Hinton DR, et al. Ryan's retina: volume 2 medical retina. 6th ed. St. Louis: Elsevier;2017. p. 1038.
2. Klein R, Klein BE, Moss SE, et al. Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology. 1984; 91:1464–1474.
3. Csaky KG, Richman EA, Ferris FL 3rd. Report from the NEI/FDA Ophthalmic Clinical Trial Design and Endpoints Symposium. Invest Ophthalmol Vis Sci. 2008; 49:479–489.

4. Diabetic Retinopathy Clinical Research Network. Browning DJ, Glassman AR, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007; 114:525–536.

5. Grading diabetic retinopathy from stereoscopic color fundus photographs: an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991; 98(5 Suppl):786–806.
6. Domalpally A, Ip MS, Ehrlich JS. Effects of intravitreal ranibizumab on retinal hard exudate in diabetic macular edema: findings from the RIDE and RISE phase III clinical trials. Ophthalmology. 2015; 122:779–786.
7. Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996; 114:1079–1084.
8. Jeon S, Lee WK. Effect of intravitreal bevacizumab on diabetic macular edema with hard exudates. Clin Ophthalmol. 2014; 8:1479–1486.
9. Shin YU, Hong EH, Lim HW, et al. Quantitative evaluation of hard exudates in diabetic macular edema after short-term intravitreal triamcinolone, dexamethasone implant or bevacizumab injections. BMC Ophthalmol. 2017; 17:182.

10. De Benedetto U, Sacconi R, Pierro L, et al. Optical coherence tomographic hyperreflective foci in early stages of diabetic retinopathy. Retina. 2015; 35:449–453.

11. Lammer J, Bolz M, Baumann B, et al. Detection and analysis of hard exudates by polarization-sensitive optical coherence tomography in patients with diabetic maculopathy. Invest Ophthalmol Vis Sci. 2014; 55:1564–1571.

12. Bolz M, Schmidt-Erfurth U, Deak G, et al. Optical coherence tomographic hyperreflective foci: a morphologic sign of lipid extravasation in diabetic macular edema. Ophthalmology. 2009; 116:914–920.
13. Niu S, Yu C, Chen Q, et al. Multimodality analysis of hyper-reflective foci and hard exudates in patients with diabetic retinopathy. Sci Rep. 2017; 7:1568.

14. Framme C, Schweizer P, Imesch M, et al. Behavior of SD-OCT-detected hyperreflective foci in the retina of anti-VEGF-treated patients with diabetic macular edema. Invest Ophthalmol Vis Sci. 2012; 53:5814–5818.

15. Ota M, Nishijima K, Sakamoto A, et al. Optical coherence tomographic evaluation of foveal hard exudates in patients with diabetic maculopathy accompanying macular detachment. Ophthalmology. 2010; 117:1996–2002.

16. Lee H, Jang H, Choi YA, et al. Association between soluble CD14 in the aqueous humor and hyperreflective foci on optical coherence tomography in patients with diabetic macular edema. Invest Ophthalmol Vis Sci. 2018; 59:715–721.

17. Miura M, Makita S, Sugiyama S, et al. Evaluation of intraretinal migration of retinal pigment epithelial cells in age-related macular degeneration using polarimetric imaging. Sci Rep. 2017; 7:3150.

18. Pemp B, Deak G, Prager S, et al. Distribution of intraretinal exudates in diabetic macular edema during anti-vascular endothelial growth factor therapy observed by spectral domain optical coherence tomography and fundus photography. Retina. 2014; 34:2407–2415.

19. Davoudi S, Papavasileiou E, Roohipoor R, et al. Optical coherence tomography characteristics of macular edema and hard exudates and their association with lipid serum levels in type 2 diabetes. Retina. 2016; 36:1622–1629.

20. Sophie R, Lu N, Campochiaro PA. Predictors of functional and anatomic outcomes in patients with diabetic macular edema t reated with ranibizumab. Ophthalmology. 2015; 122:1395–1401.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download