Abstract
The diverse infectious diseases can occur everywhere in the world, but high-risk infectious diseases should be monitored immediately after the occurrence, and be controlled not to spread to the public. Other highly contagious ones also should be screened with the surveillance system and made to be prevented from a serious effect on public health. The outbreak information, articles and news reports concerning global infectious disease outbreaks were collected from known web-based resources and deposited in Global Center for Infectious Diseases since 2016. The number of reports collected from various sources was analyzed on the respect of Blueprint priority diseases and vaccine-preventable diseases, and the characteristic outbreak trend was shown in the geographic distribution and the so-called socio-economic level of countries. The WHO R&D Blueprint priority diseases are being reported especially in the region of Africa and Asia. The vaccine-preventable and other infectious diseases also are reported continuously and world-widely. They threaten the safety of life continuously in public. Therefore, keeping close observation and strengthening infectious disease surveillance is needed, and more effort to expand the collecting resources to get more outbreak information is warranted.
No one can live without interacting with the environments including other humans, animals, and microorganisms, regardless of whether it is beneficial or harmful to humans (1). Especially, communicable infectious diseases from the interactions with microorganisms such as bacteria or viruses have threatened public health throughout the history of human. (2). The rapid development of transportation systems and frequent world-wide traveling and trading have affected the wide-spread of infectious agent in a very short time (3). It took about a month for the Spanish flu pandemic (1918) to spread from one continent to another, but nowadays it is possible in two or three days (4).
Establishing strategies for the prevention of communicable infectious diseases and applying timely measures require developing surveillance systems, which provide appropriate, efficient, and up-to-date information, to recognize outbreaks at an earlier stage (5). Many countries have developed their own surveillance systems which collect, analyze, and interpret the obtained information to evaluate the risk to the public health, but they usually do not disseminate all events to the public because of national security issues (6).
The R&D Blueprint is a global strategy and preparedness plan that enables the rapid activation of R&D activities during epidemics (7). It has determined several diseases that could seriously threaten the public health; priority diseases include Crimean-Congo hemorrhagic fever (CCHF), Ebola virus disease (EVD), Marburg virus disease, Lassa fever, Middle East respiratory syndrome coronavirus (MERS-CoV), Severe Acute Respiratory Syndrome (SARS), Nipah, henipaviral diseases, Rift Valley fever (RVF), Zika, and Disease X since 2018 (7).
In this study, we developed a surveillance system using our GCID website (Global Center for Infectious Diseases; www.gcid.or.kr) collecting outbreak information, articles and news reports concerning global infectious disease outbreaks since 2016. The collected data were categorized into the prioritized R&D Blueprint diseases and vaccine-preventable diseases and then, the outbreak trends were analyzed. Vaccine-preventable diseases are diverse and some of them have higher risks while others have lower risks. They could be an indicator reflecting the national socio-economical level and regional characteristics because they could be prevented if people are properly vaccinated. The R&D Blueprint priority diseases have been reported mainly in Africa, the Middle East, and some parts of Asia, but vaccine-preventable diseases have been reported world-widely. It is necessary to continuously develop efficient surveillance systems to collect, analyze, and provide information about communicable infectious diseases to the public, infection specialists, and health-care authorities.
The data used for this research are global infectious diseases outbreak information and reports collected from specific sources. The data have been collected in GCID webpage (Global Center for Infectious Diseases, www.gcid.or.kr), ‘Daily Alert’ board. The ‘Alerts’ have been collected from January, 2016 until June, 2019, and the data has been counted and sorted by date, country, and disease.
Sources for the data include WHO (World Health Organization, https://www.who.int/), ProMed-mail (the Program for Monitoring Emerging Diseases, http://www.promedmail.org/), Outbreak News Today (http://outbreaknewstoday.com/), Centers for Disease Control and Prevention (CDC, www.cdc.gov/), European Centre for Disease Prevention and Control (ECDC, www.ecdc.europa.eu/), Healthmap (www.healthmap.org/), and Korean Centers for Disease Control & Prevention (KCDC, www.cdc.go.kr/).
The sources have been checked and collected every weekday, while some reports that were judged to be inappropriate were filtered afterwards (outbreaks concerning plants and animals have been ruled out). The filtered-out data have not been posted in GCID webpage, and were not used for this research.
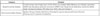
The collected infectious diseases have been categorized to ‘Blueprint priority disease’ and ‘vaccine-preventable disease’ (Table 1). ‘Blueprint priority disease’ refers to R&D Blueprint priority infectious diseases reported by WHO. ‘Vaccine-preventable disease’ refers to the infectious diseases preventable by the vaccines that are available for human.
The WHO has compiled and prioritized a list of diseases that have the potential to cause epidemic outbreaks and public health emergency in the future (7).
The list used for this research is the list reviewed on 2018 annual review of the Blueprint list of priority diseases held in February 2018 (Geneva, Switzerland). They include CCHF, EVD and Marburg virus diseases, Lassa fever, MERS-CoV and SARS, Nipah and henipaviral diseases, RVF, Zika and Disease X. However, in this research, Disease X was excluded from ‘Blueprint priority disease’, and will be discussed separately.
In this research, vaccine-preventable diseases refer to measles, mumps, rubella, diphtheria, poliomyelitis (vaccine-derived poliovirus), pertussis, influenza, and JE (Japanese Encephalitis).
Although outbreaks of chronic infectious diseases such as Human Immunodeficiency Virus infection, tuberculosis, hepatitis B, and so on, are important in public health, the emergency and the way of response to them are different from acute infectious diseases, and they are not included in this study.
We categorized the reported cases of the Blueprint priority and vaccine-preventable diseases during 2016~2018; the blue represents the Blueprint priority diseases and the purple represents the vaccine-preventable diseases (Fig. 1 and 2). The gray in Fig. 2 represents all the other diseases except for the Blueprint priority diseases and the vaccine-preventable diseases collected by the GCID surveillance systems called GCID Daily Alert. The number of total reported cases was 407 in 2016, 1849 in 2017 and 1425 in 2018. Although the reported number of Blueprint priority diseases have been increasing world-wide since 2017 (Fig. 1), the percentage of Blueprint priority diseases had been decreasing since 2016 (Fig. 2), suggesting that the surveillance system applying the appropriate measures had been working, and so, we should keep focusing on them. In the case of vaccine-preventable diseases, their reported number of cases also had been increasing but the reported places where they occurred (Fig. 1) and the percentage of them were similar for each year (Fig. 2), suggesting people were not vaccinated appropriately and in a timely manner because of the low national economical level, regional characteristics, or disbelief in vaccinations. It is notable that all the other diseases except for the Blueprint priority diseases and the vaccine-preventable diseases have significantly increased since 2016 (Fig. 2), suggesting the types of monitored infectious diseases have increased.
Fig. 3 shows that CCHF and MERS was reported in Middle East Asian countries; most CCHF cases were reported in Pakistan (8 cases) and Uganda (7 cases), and most MERS cases were reported in Saudi Arabia. EVD and Lassa fever were mostly reported in Africa; the Democratic Republic of the Congo had the most EVD cases, and Nigeria had the most Lassa fever cases. Nipah virus, RVF, and Zika cases were shown in various parts of the globe.
Fig. 4 shows the vaccine-preventable diseases reported world-wide in the GCID during 2016–2018. MMR (Measles, Mumps, and Rubella) cases are distributed all over the globe, especially in North America, Europe, and Oceania. MMR cases were reported mostly by the USA (Measles: 103 cases, Mumps: 91 cases, Rubella: 0 cases), Canada (Measles: 14 cases, Mumps: 17 cases, Rubella: 0 cases), and Australia (Measles: 28 cases, Mumps: 4 cases, Rubella: 0 cases). European countries including the United Kingdom, Ukraine, Greece, France, and Italy reported frequent MMR cases during this period. Diphtheria cases have been reported in South America and Middle East Asian regions. Venezuela had the most diphtheria reports (17 cases), followed by Yemen (11 cases) and Haiti (6 cases). Poliomyelitis has been reported in Asia, Africa and Oceania. Syria (13 cases), Papua New Guinea (12 cases), Pakistan (11 cases), Afghanistan (9 cases), and the Democratic Republic of Congo (8 cases) reported poliomyelitis during 2016-2018. JE has been reported in several Asian countries in Asia, where most were reported in India (38 cases), followed by Taiwan (13 cases). The red circles in Fig. 4 refer to countries that reported more than two kinds of vaccine-preventable diseases. Brazil reported 10 measles, 1 mumps, 4 diphtheria and 2 influenza cases, and South Africa reported 4 measles, 2 diphtheria, and 1 pertussis cases. Well-controllable infectious diseases by vaccine such as MMR until last decade were dramatically increased even in the developed countries due to vaccine hesitancy. These data urge health authorities to practice vaccination up to the WHO-recommended level.
As shown in Fig. 5, unknown or unidentified diseases (known as likely Disease X) are occurring in different parts of the world, on all continents. India and Liberia had the most reported unknown cases during 2016–2018. All reported unidentified infectious disease were not high-risk ones, and no serious and wide-spreading disease X outbreak have occurred so far since 2016.
During the first 6 months of 2019, a total of 1139 cases of infectious diseases were collected. The distribution of the cases from all continents between January and June 2019 was reported shown in Fig. 6. The country with most reported cases was the USA (331 cases), but there were no reported cases of Blueprint priority diseases.
Fig. 7 shows the kinds of diseases that occurred during the same period in Fig.6. The ten most reported infectious diseases were Measles (303 cases), Dengue (105 cases), Hepatitis A (72 cases), Mumps (37 cases), MERS (36 cases), Hantavirus (30 cases), Poliomyelitis (27 cases), Lassa fever (26 cases), Cholera (23 cases), and Chikungunya, Legionellosis, and Influenza (22 cases each). Among these only MERS and Lassa fever are the Blueprint priority diseases ranked 5th and 8th, respectively, but it does not mean that these are less important than the high ranked infectious diseases. High ranked infectious diseases may imply that they are wide-spreading and have a tendency for a rapid increase. As a matter of fact, EVD could be updated almost every day since the first outbreak in the Eastern region of the Democratic Republic of Congo (1976), but it continues to remain in the restricted area, and the number of reported cases is low. On the basis of its continuation from 2016–2018, the outbreak trend in 2019 is similar in geographic distribution.
We collected the reported outbreak cases of infectious diseases, and categorized them as Blueprint priority diseases and vaccine-preventable diseases, and their characteristic outbreak trend was observed by geographic distribution and the so-called socio-economic level of countries. For instance, some diseases were only reported in specific areas; EVD were only reported in Central African countries, and MERS and CCHF cases were only reported in the Middle East, with the exception of imported cases. Other diseases, such as cholera and diphtheria, were mostly reported in areas where the public health service system was poor, which may indicate poor hygiene, a low supply of drinking water, and low vaccination rates.
There are some limitations in this study. Due to the limited area accessibility, the search was restricted to a limited number of selected sources, and only the number of reports were considered. The reports were not official references, and only the number of articles were considered for this research, which means that the actual number of patients were not considered. Neither geographical climate information nor political situations were considered.
The most reported disease in Asia was dengue hemorrhagic fever, which is an arboviral disease epidemic in Asia, the Americas, and some Pacific islands, especially across tropical and subtropical regions (89). South East Asian countries (Philippines, Vietnam, Thailand, Singapore, Malaysia etc.) had frequent reports of dengue especially since this year. The Philippines recorded 146,062 dengue cases from January to July 20, 2019, and has declared a national epidemic of dengue fever for the first time in a century (10). The reported case number is well correlated with the real outbreak incidence.
South Asia (Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri Lanka; defined by the World Bank) is being threatened by various kinds of emerging and re-emerging infectious diseases, which is a serious problem because it has some of the world's most densely populated cities (11). This region had frequent reports of Blueprint priority disease cases: Nipah in Bangladesh and India, CCHF in Pakistan and India, Zika in India. India has reported the most diverse kinds of diseases. JE, malaria, chikungunya, Zika virus and Kyasanur forest disease are frequently reported in this country. Several factors including extreme geo-climatic diversity, increasing population, poverty and malnutrition, urbanization and deforestation and change in agricultural practices make India one of the crucial regions to keep a close observation to strengthen disease surveillance (12).
MERS is reported in Middle-Eastern countries, especially Saudi Arabia almost every week. Cholera and poliomyelitis cases are consistently reported in this region as well.
MERS-CoV has shown a clear potential and tendency to cause large outbreaks even outside the Middle East region as exemplified by the 2015 MERS-CoV outbreak in Korea (https://www.who.int/csr/don/30-may-2015-mers-korea/en/) (13).
Blueprint priority diseases have occurred the most in African countries; EVD in the Democratic Republic of the Congo, Lassa fever in Nigeria, and rift valley fever in Mayotte have been frequently reported by online resources. Nigeria had the most diverse kinds of reported cases including Lassa fever, yellow fever, vaccine-derived poliovirus, and Monkey pox. However, the most serious outbreak is EVD in the Democratic Republic of the Congo. The WHO declared the EVD outbreak in the Democratic Republic of the Congo a Public Health Emergency of International Concern (PHEIC) in July 2019 (14). Africa struggles with the greatest infectious disease burden, with a low level of hygiene, poverty, lack of political stability and poor public health infrastructure (15). Unsurprisingly, many more infectious disease cases may occur than what has been reported because the level of research, training, and surveillance are poor. A large number of endemic diseases may not have had been reported to the public.
Dengue, Chikungunya, and Zika virus are reported often in Central and South American regions. In Brazil, all 4 dengue virus serotypes circulate. Venezuela has been in economic crisis, which is responsible for serious impacts on the population's health and health care system, and has been confronted by diverse vaccine-preventable infectious disease outbreaks (16).
The USA has, by far, the most online reported cases collected for this research. However, this may be because many cases from the USA were reported at the state level rather than at the country level, and it may tell that us that the USA has well-organized reporting system.
Vaccination is recognized as a modern scientific achievement, and it is an essential preventive measure for the lives and health of children all over the world (17). The most reported infectious disease in 2019 was measles shown in Fig. 7. Measles, which is a vaccine-preventable disease had been largely eliminated by the use of the MMR vaccine. However, global measles cases have been spreading fast recently, and have been reported to be at the highest point since 2006 by the WHO (18). One hundred eighty-two countries reported 364,808 measles cases from January 1 to July 3, 2019, which is almost three times as many as 2018 (19). Although countries with low measles vaccination coverage had reported the largest outbreaks, countries with high national vaccination rates are having outbreaks as well. In the USA, the Centers for Disease Control and Prevention reported 1,044 measles cases in 28 states in June 2019 (20). The reported cases are well correlated with the outbreaks as well.
This rapid outbreak trend may be due to the worldwide hesitancy toward vaccines. Vaccine hesitancy is defined as a “delay in acceptance or refusal of vaccines despite availability of vaccination services”, by the WHO, and has been reported in more than 90% of the countries in the world, and not restricted to any specific region or continent (21). The reasons why some parents refuse or hesitate to vaccinate their children widely vary; religious reasons, personal beliefs or safety reasons (22). In Korea, one of the main reasons to hesitate and refuse vaccination was that people were not recognizing the meaningfulness of infection prevention (23). Unfortunately, when people choose not to vaccinate their child, he or she is not only harming their own child, but possibly exposing other children and families as well. Vaccine hesitancy is a complex global concern and requires ongoing monitoring.
Conclusively the prioritized R&D Blueprint diseases chosen by the WHO are being reported in many parts of the world, especially in the region of Africa and Asia. The vaccine-preventable and other infectious diseases are continuously reported world-wide. In this study, we analyzed the Blueprint priority diseases and vaccine-preventable diseases. Monitoring both serious diseases prioritized by the Blueprint and vaccine-preventable diseases that still occur worldwide is essential in predicting and preventing infectious diseases. Keeping close observation and strengthening infectious disease surveillance are needed, and more effort is warranted to expand the collecting resources to get more outbreak information.
Figures and Tables
Figure 1
The distribution of the Blueprint priority diseases cases (blue) and the vaccine-preventable diseases cases (purple) collected in GCID Daily Alert, 2016~2018 by country (World map, A: 2016, B: 2017, and C: 2018).

Figure 2
The proportion chart of the Blueprint priority diseases cases (blue), the vaccine-preventable diseases cases (purple), and the other diseases (gray) collected in GCID Daily Alert, 2016~2018.

Figure 3
The distribution of the Blueprint priority diseases marked on the world map, indicated by color (Red: Crimean-Congo hemorrhagic fever, Orange: Ebola virus disease, Yellow: Lassa fever, Blue: MERS-CoV, Purple: Nipah virus, Green: Rift Valley fever, Beige: Zika virus).

Figure 4
The distribution of the vaccine-preventable diseases marked on the world map, indicated by color (Blue: Measles, Mumps, Rubella, Yellow: Influenza, Orange: Diphtheria, Pink: Poliomyelitis, Red: Varied, more than two kinds of vaccine-preventable diseases).

Acknowledgments
This work was supported partly by a grant (No.2014K1B1A1073282) from Ministry of Science and ICT, Republic of Korea, and partly by the Education and Research Encouragement Fund of Seoul National University Hospital.
References
2. Abat C, Chaudet H, Rolain JM, Colson P, Raoult D. Traditional and syndromic surveillance of infectious diseases and pathogens. Int J Infect Dis. 2016; 48:22–28.

3. Grout A, Howard N, Coker R, Speakman EM. Guidelines, law, and governance: disconnects in the global control of airline-associated infectious diseases. Lancet Infect Dis. 2017; 17:e118–e122.

4. Martini M, Gazzaniga V, Bragazzi NL, Barberis I. The Spanish Influenza Pandemic: a lesson from history 100 years after 1918. J Prev Med Hyg. 2019; 60:E64–E67.
5. Drouin S, Collins DL. PRISM: An open source framework for the interactive design of GPU volume rendering shaders. PLoS One. 2018; 13:e0193636.

6. Wolicki SB, Nuzzo JB, Blazes DL, Pitts DL, Iskander JK, Tappero JW. Public Health Surveillance: At the Core of the Global Health Security Agenda. Health Secur. 2016; 14:185–188.

7. WHO. 2018 Annual review of the blueprint list of priority diseases. https://www.who.int/blueprint/priority-diseases/en/.
8. Pinheiro FP, Corber SJ. Global situation of dengue and dengue haemorrhagic fever, and its emergence in the Americas. World Health Stat Q. 1997; 50:161–169.
10. Dyer O. Dengue: Philippines declares national epidemic as cases surge across South East Asia. BMJ. 2019; 366:l5098.

11. Laxminarayan R, Kakkar M, Horby P, Malavige GN, Basnyat B. Emerging and re-emerging infectious disease threats in South Asia: status, vulnerability, preparedness, and outlook. BMJ. 2017; 357:j1447.

12. Mourya DT, Yadav PD, Ullas PT, Bhardwaj SD, Sahay RR, Chadha MS, et al. Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian J Med Res. 2019; 149:447–467.

13. Al-Tawfiq JA, Omrani AS, Memish ZA. Middle East respiratory syndrome coronavirus: current situation and travel-associated concerns. Front Med. 2016; 10:111–119.

14. WHO. Ebola outbreak in the Democratic Republic of the Congo declared a Public Health Emergency of International Concern. https://www.who.int/news-room/detail/17-07-2019-ebola-outbreak-in-the-democratic-republic-of-the-congo-declared-a-public-health-emergency-of-international-concern.
15. Fenollar F, Mediannikov O. Emerging infectious diseases in Africa in the 21st century. New Microbes New Infect. 2018; 26:S10–S18.

16. García-Gómez P, Jiménez-Martín S, Labeaga JM. Consequences of the Economic Crisis on Health and Health Care Systems. Health Econ. 2016; 25 Suppl 2:3–5.

17. Edwards KM, Hackell JM. COMMITTEE ON INFECTIOUS DISEASES. THE COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE. Countering Vaccine Hesitancy. Pediatrics. 2016; 138:e20162146.

18. WHO. New measles surveillance data from WHO. 2019. https://www.who.int/immunization/newsroom/new-measles-data-august-2019/en/.
19. Mahase E. Measles cases at highest point since 2006 as outbreaks continue to spread. BMJ. 2019; 366:l5141.

20. CDC. Measles Outbreaks. 2019. https://www.cdc.gov/measles/cases-outbreaks.html.
21. Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy--country-specific characteristics of a global phenomenon. Vaccine. 2014; 32:6649–6654.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download