This article has been
cited by other articles in ScienceCentral.
Abstract
Background and Purpose
This randomized controlled study examined the effect of repetitive transcranial magnetic stimulation (rTMS) on spasticity in patients with multiple sclerosis (MS).
Methods
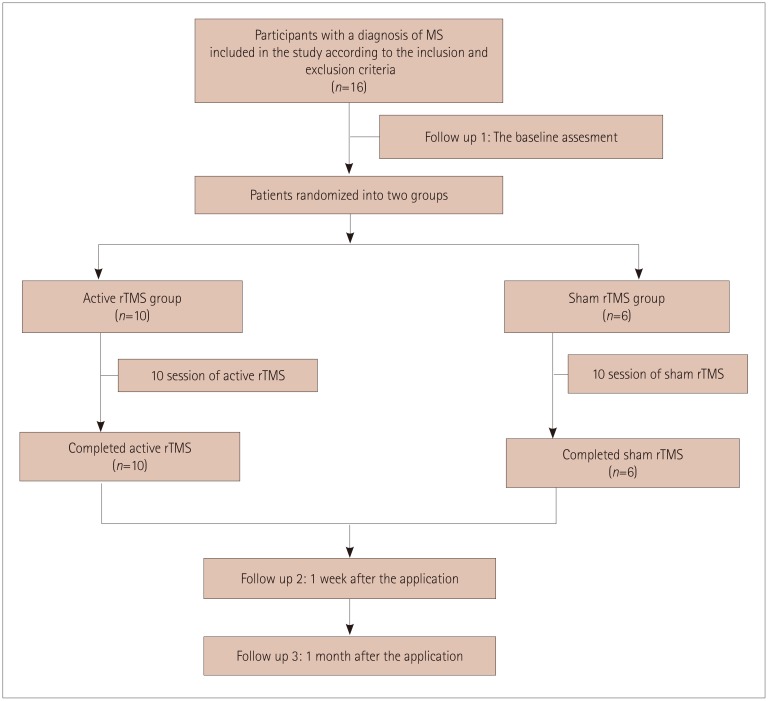
This study included 16 patients with a history of MS and spasticity in the adductor hip muscles according to the Modified Ashworth Scale (MAS). The participants were randomized into the active group (n=10) and control group (n=6), in which active rTMS and sham rTMS were applied in 10 sessions, respectively. A physical therapy and rehabilitation program was applied along with rTMS sessions in both groups. The evaluation parameters were assessed at baseline and then 1 week and 1 month after applying rTMS.
Results
Statistical analyses with post-hoc correction revealed statistically significant improvements in the active group compared to the control group in the bilateral MAS score, Penn Spasm Frequency Scale score, patient satisfaction, amount of urine leakage, actual health status, perceived health status, energy and fatigue, role limitations due to physical problems, social function, overall quality of life, cognitive functioning, physical health composite score, mental health composite score, and total score on the Multiple Sclerosis Quality of Life-54 (MSQOL-54) (p<0.05). Statistically significant changes were detected in the MSQOL-54 social function and physical health composite scores of patients in the control group (p<0.05).
Conclusions
Active rTMS combined with a physical therapy program reduced spasticity in MS patients compared to the control group that received only physical therapy. Further comprehensive and more advanced studies are needed to confirm the present findings.
Go to :

Keywords: repetitive transcranial magnetic stimulation, multiple sclerosis, spasticity
INTRODUCTION
Multiple sclerosis (MS) is an autoimmune, chronic, and inflammatory disorder characterized by demyelination in the central nervous system.
1 The pathology is related to a series of immunomediated reaction chains, specifically directed against axons and myelin. The balance of T helper 1 and 2 cells is impaired in the direction of inflammation, and white matter is degraded.
2 A loss of strength, fatigue, balance problems, cognitive impairments, double vision, sensorial complaints, and emotional changes are common symptoms of the disease.
34 The symptoms of MS play a decisive role in the prognosis of this clinical condition.
Spasticity is a common symptom of MS and one of the causes of disability, and it gives rise to secondary problems such as sleep disorders, pain, bladder dysfunction, and walking and movement disorders.
567 Spasticity is a motor disorder that occurs as a result of hyperexcitability of stretch reflexes accompanied by a velocity-dependent increase in tonic stretch reflexes and hyperbolic tendon jerks.
8
The spasticity in MS can be associated with denervation hypersensitivity and the formation of new branches in the descending motor pathways to create new synaptic connections with spinal neurons.
6 The spasticity that occurs in MS is much more common in the lower extremities.
67 Because the adductor muscles are significantly affected, restrictions in movement and the usage of a wheelchair can occur that lead to the need for increased patient care and the risk of pressure ulcers.
679
New treatment approaches are needed for patients with MS in whom full recovery is not possible in order to get improve their motor and mental functions.
10 It was recently thought that rehabilitation techniques able to drive central nervous system plasticity could be effective.
11 As a result, noninvasive brain stimulation modalities such as repetitive transcranial magnetic stimulation (rTMS) and transcranial direct-current stimulation (tDCS) have been used for treating the spasticity in patients with MS.
101112 rTMS is a noninvasive method of brain stimulation that modulates the cortical excitability of the motor field, and so it can affect the descending corticospinal pathway.
13 The modifications may be affected by the frequency of the stimulation.
1415 rTMS at a frequency of 1 Hz or lower can induce cortical inhibition, and while treatment at 5 Hz or higher may result in cortical stimulation.
14
In this study we examined the effect of rTMS on spasticity in patients with MS. We also evaluated the benefits of the treatment on pain, spasm frequency, sleep status, voiding pattern, and range of joint motion. To the best of our knowledge, this study is the first to evaluate the long-term efficacy of rTMS on spasticity in patients with MS with a 1-month follow-up.
Go to :

METHODS
A randomized, prospective, and sham-controlled study was performed at a rehabilitation center. The primary end point in this study was the efficacy of rTMS applied to spasticity in patients with a diagnosis of MS. The effects of the treatment on pain, spasm frequency, sleep state, voiding pattern, and joint range of motion were examined as secondary end points. The participants were assessed at baseline and then 1 week and 1 month after applying the stimulation. During the evaluation process, the Modified Ashworth Scale (MAS) score, Penn Spasm Frequency Scale (PSFS) score, Visual analogue scale (VAS) score, Passive Range of Motion Measurement, Epworth Sleepiness Scale, patient satisfaction, voiding diary, and Multiple Sclerosis Quality of Life-54 scale (MSQOL-54) scores were used as outcome measures. There are many clinical instruments available for assessing disability and neurological impairment in MS.
16 Although the Expanded Disability Status Scale is the most commonly used scale in this application, it is characterized by poor reproducibility and a poor ability to assess cognitive and upper extremity functions.
1718 On the other hand, MSQOL-54 is a disease-specific scale for assessing cognitive functioning, level of pain, sexual functioning, overall quality of life, level of anxiety provoked by the health status, level of energy, and sexual and social functioning,
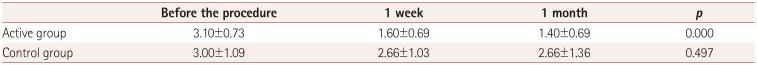
19 and the clinical efficacy of this MSQOL-54 prompted us to use this scale in the present study. This study included 16 patients after applying the inclusion and exclusion criteria. The patients were randomized into two groups: the active rTMS group (
n=10) and sham rTMS group (
n=6) (
Fig. 1).
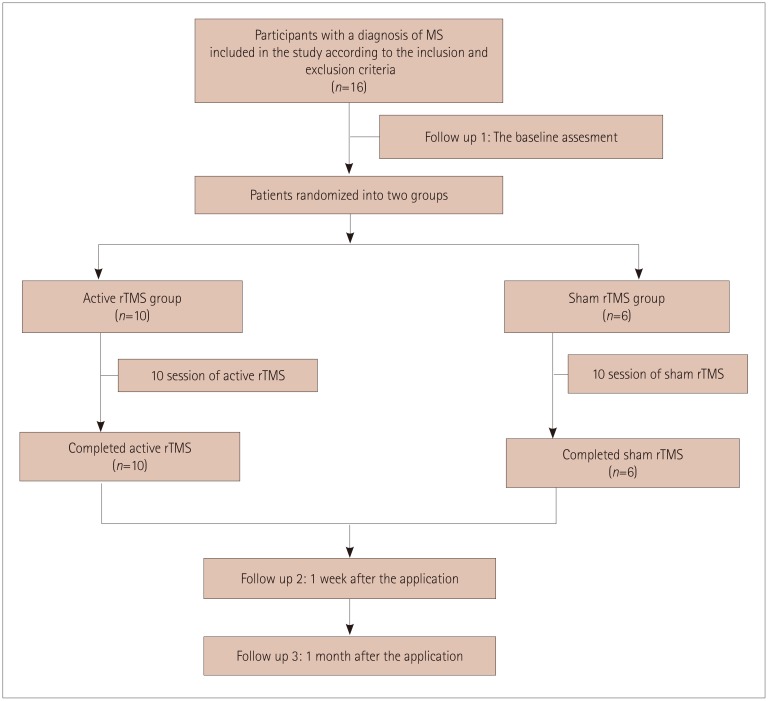 | Fig. 1Flow chart of the study. MS: multiple sclerosis, rTMS: repetitive transcranial magnetic stimulation.
|
The inclusion criteria were being aged 18–50 years, being diagnosed with MS at least 6 months previously, having a hip adductor muscle tone grade of between 2 and 4 on the MAS, and being willing to voluntarily participate in this study. The included patients had a past history of using antispasmolytic medications, but they reported that the level of their spasticity had not been relieved by medical treatments. Therefore, none of the patients were receiving a drug therapy that had the possibility of modifying cortical excitability. All of the participants also required assistance for ambulation. Exclusion criteria were major general health problems (e.g., heart failure or chronic obstructive pulmonary disease), skin lesions, serious infectious disorder, pregnancy, malignancy, bleeding disorder, implanted pacemaker, cardiac arrhythmia, or refusing to participate. All of the participants signed an informed consent form, and they were allowed to withdraw from this study at any time for any reason. The Local Ethics Committee granted approval for the study (IRB No. 2016-KAEK-03; 2016/01).
Patients were randomized to receive rTMS using an active figure-eight-shaped coil or a sham coil. In the active treatment group, rTMS was applied at a frequency of 5 Hz consisting of 900 pulses over 15 minutes over the vertex region targeting the lower extremity motor area for 10 sessions lasting 2 weeks. The lower extremity motor area of the cerebral cortex was localized using the Brainsight TMS Navigation System (Rogue Research, Montréal, Canada) available in our hospital. The intensity of rTMS stimulation was adjusted to 110% of the resting motor-unit potential threshold obtained by stimulating the tibialis posterior muscle on the side where the weakness was more prominent. In the control group, sham rTMS was administered with a 70-mm figure-eight-shaped sham coil for 10 sessions over 2 weeks (for a total of 10 days), with each session lasting 15 minutes and one session performed per day. During rTMS, a physical therapy and rehabilitation program that included the joint range of motion, stretching, strengthening, walking exercises, and balance-and-coordination training was applied by a physiotherapist to both groups. Thus, the physical therapy program was performed with all patients in both groups as the primary treatment and patients received rTMS as the secondary treatment.
Statistical analyses were performed using version 22.0 of SPSS software (IBM Corp., Armonk, NY, USA). Mean±SD, median, minimum, and maximum values were determined. The Kolmogorov-Smirnov test was used to compare two groups and determine whether the obtained parameters conformed to a normal distribution. The Mann-Whitney U test was used to compare continuous variables between two groups, and the chi-square test was used for intergroup comparisons of intermittent variables. The Friedman test was applied for multiple comparisons within groups, and the Bonferroni-corrected Wilcoxon test was carried out as a post-hoc test. The Spearman correlation test was used to evaluate correlations between variables, while the McNemar test was used to perform intragroup comparisons of intermittent variables. A probability value of p<0.05 was considered statistically significant.
Go to :

RESULTS
The 16 patients with MS who completed this study were aged 49.93±12.27 years. There was a male preponderance in the active group but a female preponderance in the control group. The duration of MS was 16.5±9.01 years. The patient characteristics are presented in
Table 1, none of which differed significantly between the groups (
p>0.05).
Table 1
Comparison of the pretreatment characteristics of the patients between the two study groups


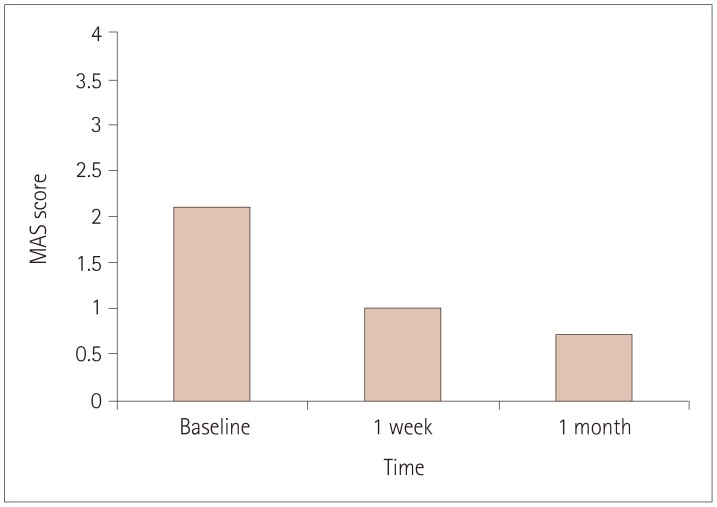
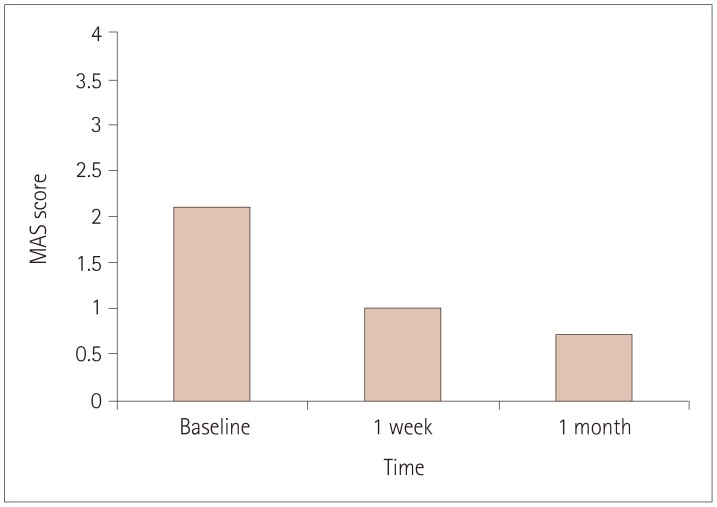
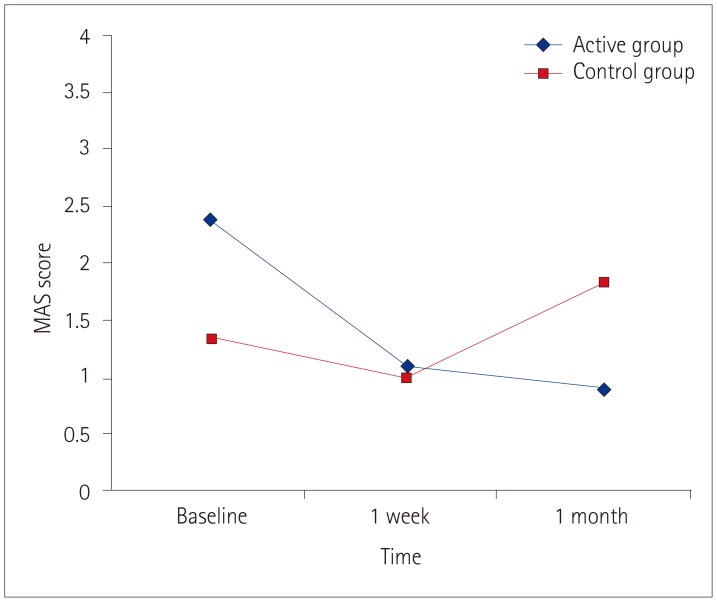
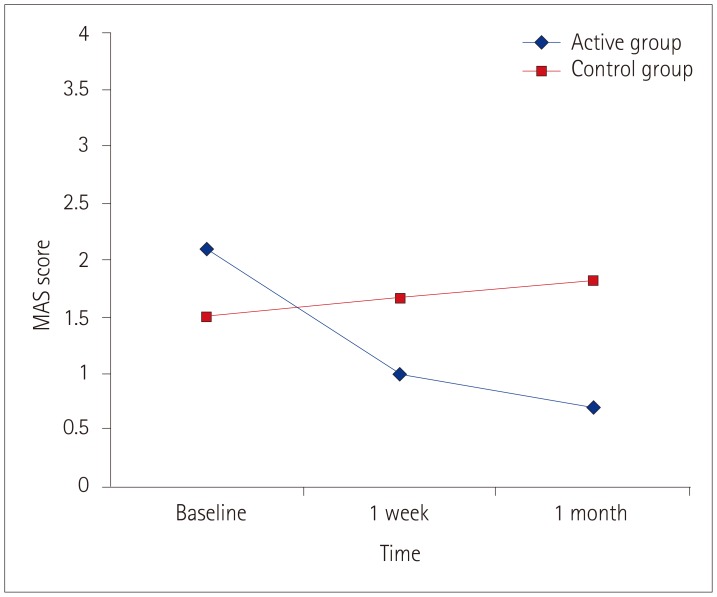
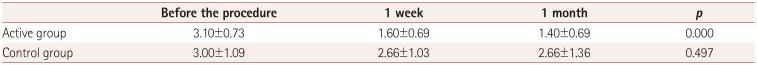
Significant reductions in the MAS scores for the hip adductors bilaterally were detected over time after rTMS in the active group (
p=0.005) (
Figs. 2 and
3). In contrast, there were no statistically significant differences between the MAS scores measured in the control group (
p>0.05). The changes in MAS scores are compared between the two groups in
Figs. 4 and
5.
 | Fig. 2Changes in MAS score for the right hip adductor muscles in the active group over time. MAS: Modified Ashworth Scale.
|
 | Fig. 3The changes in MAS scores of the left hip adductor muscles in active group over time. MAS: Modified Ashworth Scale.
|
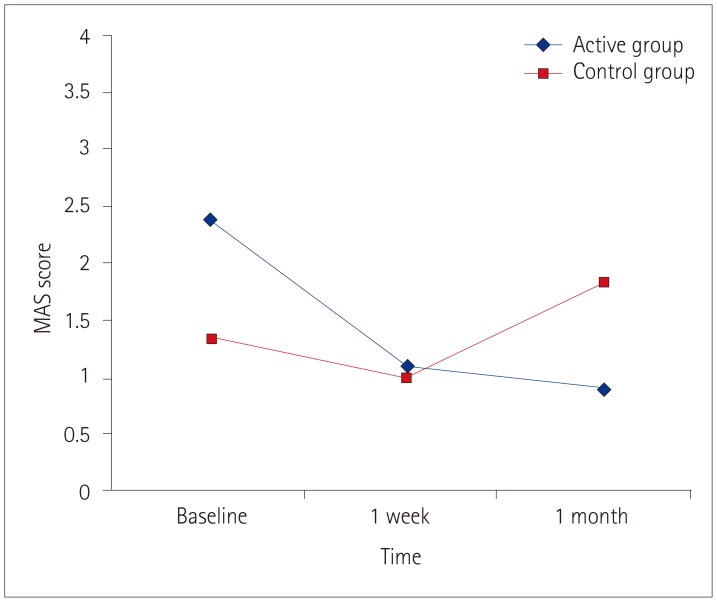 | Fig. 4Comparison of the active and control groups according to the changes in MAS scores of the right hip adductor muscles before and after the application. MAS: Modified Ashworth Scale.
|
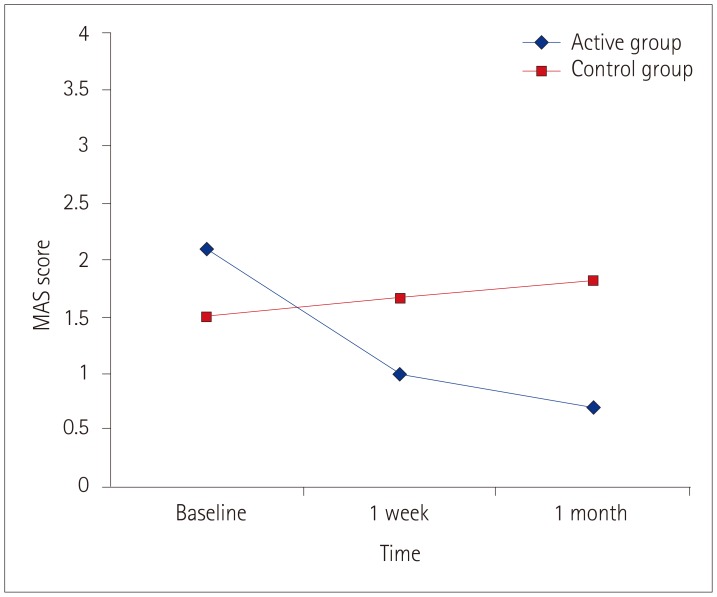 | Fig. 5The comparision of the active and control groups according to the changes in MAS scores of left hip adductor muscles before and after the application. MAS: Modified Ashworth Scale.
|
Participants in the active group showed significant improvements in the PSFS score at the follow-up visits (
p<0.01). No significant differences were detected in the PSFS scores in the control group (
p>0.05) (
Table 2).
Table 2
Comparison of the active and control groups according to the changes in Penn Spasm Frequency Scale scores for the left hip adductor muscles between before and after the treatment

We also analyzed the effect of rTMS on the amount of urinary leakage. The amounts of urinary leakage in the active group were 842.90±1,916.46, 402±1,264, and 0.60±1.89 drops/day at baseline, 1 week, and 1 month, respectively; this change was statistically significant (p=0.002). In contrast, the urinary leakage did not change significantly in the control group (p>0.05).
We detected significant changes in the actual health status, perceived health status, energy and fatigue, role limitations due to physical problems, social functioning, overall quality of life, cognitive functioning, MSQOL-54 components, physical health composite score, mental health composite score, and total score on the MSQOL-54 of the patients in the active group (p<0.05). There were no significant differences in the other parameters in the active group (p>0.05) during the follow-up period. On the other hand, significant improvements were detected in the MSQOL-54 social function component, physical health composite score, and total score in the control group during the follow-up period (p<0.05).
Patient satisfaction improved significantly in the active group after the treatment (p=0.020), while it did no change significantly in the control group (p>0.05). No adverse effects or complications were observed in either group during the follow-up period.
The present analysis and post-hoc evaluations revealed that the active treatment protocol did not significantly change the pain level, sleep state, range of joint motion, or voiding-diary parameters; the only exception was the amount of urinary leakage.
Go to :

DISCUSSION
This study found that active rTMS reduced spasticity and the spasm frequency in patients with MS. This effect was seen 1 month after the treatment sessions in the active group. Spasticity had not changed significantly after the treatment in the sham group.
Read et al.
20 investigated the effects of high-frequency spinal cord stimulation on the functional status of patients with MS and also the underlying mechanism, and found a significant reduction in the degree of lower extremity spasticity in 6 of 11 patients. The present results are consistent with those previous findings. Those authors reported that a direct muscle response could be elicited by spinal cord stimulation via direct excitation of the anterior horn cells or inducing the descending pathways, and that this intensive and sustained descending inhibition could explain the depression and healing in local reflexes associated with voluntary working muscles. It is predicted that TMS can either provide inhibition or excitation by generating depolarization or hyperpolarization at the cellular level in the region of efficacy.
212223
Centonze et al.
13 applied rTMS at 5 Hz for 2 weeks to 19 patients diagnosed with MS and lower extremity spasticity. A significant difference was found in the lower extremity MAS scores at assessments performed immediately and 1 week after the protocol, while no significant difference was detected between pretreatment and after 2 weeks.
13 To the best of our knowledge, the present study had the longest follow-up period (a 1-month assessment), and we observed significant improvements in MAS scores and spasm frequency beginning 1 week after applying rTMS.
rTMS has also been used in many neurological conditions including cerebral palsy, stroke, and spinal cord injury.
1124252627 Kumru et al.
25 examined the efficacy of rTMS at 20 Hz in 15 patients with incomplete spinal cord injury and lower extremity spasticity, and found significant reductions in MAS and modifications to PSFS scores that were similar to the results of the present study. Those authors also detected improvement in the spasticity-related VAS score and sleep quality in the active rTMS group. In contrast, we found no significant improvements in VAS and Epworth Sleepiness Scale scores between the active and control groups. Gupta et al.
26 reported the superiority of rTMS compared to standard therapy in patients with spastic cerebral palsy. In that study the patients in the experimental group received both rTMS and standard treatment, while only the standard treatment was applied in the control group. Those authors found a significant large decrease in muscle tone in the study group, but only a small decrease in muscle tone in the control group. Mori et al.
28 randomized their study participants into three interventions: intermittent transcranial magnetic theta-burst stimulation (iTBS) plus exercise therapy (ET), sham stimulation plus ET, and iTBS alone. Those authors found significant improvements in both MAS scores and multiple-sclerosis-related scale scores only in the combined-treatment group. The results of our study also suggest that the combining rTMS and physical therapy could be more effective. During the rTMS, a physical therapy and rehabilitation program that included the joint range of motion, stretching, strengthening, walking exercises, and balance-coordination training was provided to both groups by a physiotherapist. This particular design of the present study meant that rTMS acted as a supportive treatment for physical therapy programs, which was the main treatment modality for patients in both the active and control groups.
Read et al.
20 examined the effect of spinal cord stimulation on the functional status of patients with MS, and reported that the descending inhibition induced by such stimulation can depress bladder function, which might improve the symptoms of the patients. We therefore hypothesized that spasticity can induce voiding pattern disorders secondarily, and we aimed to improve both spasticity and the related voiding disorders by using rTMS to induce the inhibitory pathways in this study. Centonze et al.
15 investigated the effects of applying excitatory rTMS at 5 Hz to the lower extremity motor area in patients with MS who had urinary tract system complaints. Those authors concluded that rTMS at 5 Hz had no effect on the filling phase of the bladder, but that relaxation of the urethral sphincter was facilitated by the increased excitability of the corticospinal pathway induced by excitatory rTMS. Our study also investigated the effect of 5-Hz rTMS on voiding symptoms, but we did not detect any significant improvement in voiding-diary parameters other than in the amount of urinary leakage in the active group.
There is also a dearth of studies of the effect of other noninvasive brain stimulation modalities such as tDCS on spasticity in patients with MS. The only study reported on in the literature was performed by Iodice et al.,
29 in which ten patients received anodal tDCS to the primary motor cortex on the more-affected side for 20 minutes/day for 5 consecutive days, while the patients in the control group received sham tDCS. The MAS score did not differ significantly between their tDCS and sham groups. Further prospective and randomized controlled studies are needed to analyze the efficacy of tDCS on the spasticity experienced by patients with MS.
No side effects were observed in our patients. Nielsen et al.
30 reported that all patients experienced a squeezing sensation around the midthoracic level during the stimulation, and a single episode of dizziness occurred in one patient. In another study by the same authors, two patients complained of short-term dizziness after treatment sessions, and one patient complained of dysrhythmia 2 hours after the treatment session.
24 Those authors considered that the treatment may exert a systemic hemodynamic effect, but the dizziness of the patient could also have had an orthostatic source. On the other hand, the electrocardiographic record of their patient reporting dysrhythmia did not confirm their complaint.
While the present study achieved its intended objectives, it had limitations of the small number of participants (due to the application of comprehensive inclusion criteria) and the lack of electrophysiological and urodynamic recordings as evaluation parameters. However, this study can provide guidance for future studies because the present findings reflect clinical data and the direct complaints of the included patients.
In conclusion, the findings of this study indicate that rTMS may benefit patients with MS. However, further comprehensive and more advanced studies are needed to confirm the present findings.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download