Abstract
Purpose
In Korea, the prevalence of dementia patients has increased, which makes the care burden of nurses important. The purpose of this study is to identify factors affecting the care burden of nurses caring elderly patients with dementia.
Methods
A cross-sectional design was conducted using a convenience sample of 127 nurses from two hospitals and a nursing home in Korea. Participants completed questionnaires on knowledge of and attitudes toward dementia, social support, self-esteem, dementia problematic behavior (DPB), and professional caregiver burden index. The data were analyzed by using the t-test, ANOVA, Pearson correlation, and multiple regression with the SPSS/windows version 21.0 program.
Dementia is a disease defined by memory impairment and cognitive disorder. It is commonly accompanied by at least two of the following symptoms: aphasia, apraxia, agnosia, and performance dysfunction [1]. In Korea, the number of patients with dementia exceeds 500,000. This number is expected to double every 20 years, reaching 1.14 million patients by 2030 and 2.13 million by 2050. Moreover, due to a rapidly aging population, dementia has emerged as a major health problem in Korea [2].
The causes of dementia can largely be attributed to any of the following diseases: degenerative disease, vascular dementia, metabolic disease, infectious disease, addictive disease, and deficiency disease [3]. Dementia is associated with impairment of memory, orientation, language, calculation, and judgment, as well as changes in mood, emotional control, or behavior and challenges in performing activities of daily living. It is accompanied by various behavioral symptoms with negative impacts on daily functions [4]. These behavioral symptoms may induce extreme stress in family members and increase the burden of caregivers, which may be the most important reason for the admittance of these patients into nursing homes [5].
Korea introduced the National Responsibility Policy for Dementia Care in 2017, mandating the placement of 1 nurse for every 25 patients in elderly care facilities, and Dementia Safe Centers are required to have at least 1 nurse with more than five years of experience [6]. Thus, the role of nurses in the care of dementia patients has increased. However, despite the need to secure nursing personnel for dementia patients, nurses face a great burden in caring for them, making it difficult to secure the necessary nursing capacity. This burden faced by nurses negatively affects care for dementia patients and leads to a negative cycle of lower quality care provided for dementia patients.
Recent studies of the burden of caring for dementia patients suggest that variables related to dementia patients themselves include behavioral and psychological symptoms of dementia [5], severity of cognitive decline, and a decline in the level of abilities to perform the activities of daily living [7]. Factors related to the personal characteristics of the caregivers include sociodemographic characteristics such as age, gender, and relationship with dementia patients, and perceived health, knowledge of dementia, and attitude toward dementia patients [89]. Self-esteem, which can influence the care burden, is a positive self-perception; it has been confirmed that the self-esteem of nurses who care for dementia patients at a hospital is related to the quality of care provided to the patients [10]. On the other hand, social support, as a psychosocial factor, is related to care burden [11]. Social support refers to the emotional, informational, and material support received by the target from the social network, and has been identified as a factor that has a positive influence on the caregivers who experience the burden of caring for dementia patients [12].
However, research to date on the burden of care associated with dementia patients has largely focused on the families [9], caregivers [5], and care assistants [13] caring for the dementia patients, while little research has investigated the burden of care experienced by the nurses at the center of care for dementia patients.
According to the theory of stress, appraisal, and coping of Lazarus and Folkman, the stress experience is a result of the interaction between humans and the environment, and this theory emphasizes coping and supportive resources as crucial elements of adaptation in stressful situations [14]. In one study of the burden of caregivers for the elderly with dementia that applied the stress, appraisal, and coping theory, it was found that the coping and support of the caregivers are important factors explaining their stress [13].
Therefore, in this study, the stress, appraisal, and coping theory of Lazarus and Folkman [14] was selected as the theoretical foundation to confirm the factors influencing the burden of care for nurses caring for dementia patients. This can help secure nursing resources for the care of dementia patients in the future, and may also contribute to increasing the quality of care for dementia patients.
The purpose of this study was to identify factors affecting the knowledge of dementia, attitude toward dementia, self-esteem, dementia problematic behaviors, social support, and care burden of nurses caring for elderly patients with dementia.
In this study, the stress, appraisal, and coping theory of Lazarus and Folkman [14] was selected as the conceptual framework to confirm the factors influencing the care burden of nurses caring for elderly patients with dementia. The key concepts of this theory are stress, coping, and adaptation; the stress-appraisal coping theory explains the process of adapting to environmental stimuli or difficulties as a result of the interaction between humans and the environment. Therefore, in this study, the causal and independent variables of stress faced by nurses caring for dementia patients have been divided into the nurses' personal factors and dementia patients' factors. Personal factors include the knowledge, attitude, and self-esteem of nurses, and the patient factors include problematic behaviors associated with dementia. Appraisal factors include social support, and a long-term coping process, which is a negative and not a positive construct, was set for the burden of care through a final assessment (Figure 1).
This study was a descriptive correlation investigative study that aimed to discover whether the knowledge of dementia, attitude toward dementia, self-esteem, dementia problematic behaviors, and social support impact the care burden of nurses caring for patients with dementia. This study was conducted using convenience sampling.
This study included experienced nurses who provide care to elderly patients with dementia in a geriatric hospital, a dementia ward in a mental hospital, and a nursing home. The duration of this study was from October 1st, 2013, to January 30th, 2014. The number of subjects was calculated for a significance level of .05 and medium effect size of .15 to secure 80% statistical power for multiple regression analysis using the G*power 3.1.2 program. This study of effect size was based on the medium effect size found in a previous study of the care burden of patients with dementia [15].
The adequate sample size was determined to be 118 persons. Survey questionnaires were administered to 154 participants to allow for a typical dropout rate. The number of samples in this study was 150 persons; after excluding 23 subjects who did not complete the questionnaire or had missing data, the final total number of subjects for analysis was 127. The purpose of the study was explained to the head of each facility, and the subjects' consent was obtained before data collection was conducted.
The Knowledge of Dementia Scale was developed by Jung [16]. This tool comprises 10 questions about knowledge of dementia, 3 about knowledge treatments, and 7 about knowledge of nursing dementia, for a total of 20 questions. All responses were yes or no, and correct answers were scored 1 point for a maximum possible score of 20 points. Higher scores indicated greater knowledge of dementia. Cronbach's α was .64 in Jung's [16] study and .68 in the current study.
This tool was developed to measure attitudes toward dementia by Norbergh et al. [17] and translated into Korean by Park [8]. This tool comprises 24 ethical-aesthetic questions, 6 questions on ability to experience, 4 questions on ability of social interactions, and 4 questions on the ability to understand, for a total of 38 questions. Responses are scored on a 7-point scale, with scores ranging from a minimum of 38 points to a maximum of 266 points; higher scores indicate greater negative attitudes. Cronbach's α was .87 in Park's [8] study and .96 in the current study.
This instrument to measure self-esteem was developed by Rosenberg [18] and translated into Korean by Jon [19]. This tool includes 5 questions on positive self-esteem and 5 questions on negative self-esteem, for a total of 10 questions. Measurements are made on a 4-point scale; negative questions are inversely scored and converted, and the scores range from a minimum of 10 points to a maximum of 40 points. Higher scores mean higher self-esteem. Cronbach's α was .93 in Jon [19] and .74 in the current study.
This instrument developed by Kim [20] was used to measure inappropriate behaviors of dementia that result in negative consequences for the caregiver. The DPB Scale comprises 25 items rated on a 3-point Likert scale: 6 items of aggressive behavior, 6 items of agitation behavior, 5 items of nursing resistance, 3 items of physical symptoms, 3 items of neurological symptoms, and 2 items of psychotic symptoms. The total score ranges from 0 to 75, with higher scores indicating higher levels of dementia problematic behaviors. Cronbach's α was .91 in Kim [20] and .96 in the current study.
The Social Support Scale was developed by House and Wells [21] to quantify social support, and was translated into Korean by Jung [22]. This tool measures the extent of perceived support from superiors, coworkers, family members, and friends, and comprises 24 items scored on a 5-point Likert scale; the scores range from a minimum of 24 points to a maximum of 120 points, where higher scores indicate that nurses receive more support. Cronbach's α was .93 in Jung [22] and .95 in the current study.
The Professional Caregiver Burden Index (PCBI) was developed by McCarty and Drebing [23] and translated into Korean by Song et al. [5]. The K-PCBI includes 4 questions on physical burden, 4 questions on emotional burden, 4 questions on lack of empathy/indifference, and 4 questions on negative working attitude/ability, for a total of 16 questions scored on a 4-point scale; the scores range from a minimum of 16 points to a maximum of 64 points. Higher scores signify greater caregiver burden. Cronbach's α was .92 in Song et al. [5] and .88 in the current study.
The data collected in this study were analyzed using the SPSS Statistics 21.0 program. The general characteristics of the subjects and the burden of nursing care were analyzed using descriptive statistics. Furthermore, the correlation between variables was analyzed with Pearson's correlation coefficients. Differences in nurses' burden of care by general characteristics of the subjects were analyzed by independent t-tests and one-way ANOVA. Hierarchical regression analysis was then conducted to examine the influence of the variables presented in the conceptual framework of the nurses' burden of care in relation to the subjects.
This study was approved by the appropriate ethics committee prior to data collection (Registration #2013-0037-1). The objectives of this study, as well as the risks and benefits of participation and the contact number of the researcher, were disclosed. Moreover, the participants were informed of the possibility of withdrawal. They were assured that data collection was solely for research purposes and that their anonymity would be honored. The completed surveys were placed in separately sealed envelopes, which were then collected in larger envelopes prepared beforehand for each institution. Upon completion of data collection, the larger envelopes were also sealed, and the researcher visited each institution personally to collect them.
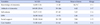
The participants' characteristics are shown in Table 1. The mean age of the participants was 40.79 years, and 82 (64.6%) were married. Among them, 54.3% were college graduates and 66.9% were religious. The mean clinical career was 12.01 years, and 82 (64.6%) were working in geriatric hospitals. The results of the analysis of the difference of care burden by the general characteristics of the study subjects indicated statistically significant differences in the care burden according to the type of work (F=4.21, p=.017). According to the Scheffé test, the care burden of nurses was higher in those with day shifts than in those with rotating and night shifts (Table 1).
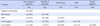
The mean knowledge score in the participants was 16.80 (with a range of 0~20), and the rate of correct answers was 84.3%. The mean attitude score of subjects in this study was 169.08 (with a range of 38~266), and the average item score was 4.42 out of 7 points. The score for self-esteem was 32.27 points and the score for dementia problematic behaviors was 36.58 points. The mean social support score of subjects in this study was 91.80 and the average item score was 3.84 out of 5 points, and the subjects' care burden had a mean of 31.08 points out of 64 (Table 2).
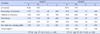
The knowledge of dementia (r=−.13, p=.148), attitude towards dementia (r=.17, p=.071), and care burden of our subjects did not show statistically significant correlations. Analysis of the correlation between care burden and each of the main variables found that self-esteem (r=−.28, p=.002) and social support (r=−.26, p=.004) show a negative correlation with participation in care burden, while dementia problematic behaviors (r=.26, p=.011) showed a positive correlation (Table 3). In other words, as the level of self-esteem and social support became lower, the level of the care burden increased. On other hand, as the levels of dementia problematic behaviors became higher, the level of the care burden increased.
This study conducted a hierarchical regression analysis based on the stress, appraisal, and coping model of Lazarus and Folkman [14]. The independent variables included in the regression model were dementia knowledge and attitude, self-esteem, dementia problematic behaviors, and social support. In the univariate analysis, type of work was analyzed using dummy variables. The possible presence of auto-correlation and multicollinearity for the regression model were assessed with the Durbin-Watson statistic (2.09), tolerance (.87~.98), and variance inflation factor (1.01~1.14), confirming that the basic requirements of regression analysis were satisfied.
The results of the hierarchical regression analysis indicated that the first step-regression model was statistically significant (F=6.61, p<.001) in terms of nurse factors and patient factors, and the explanatory power of the first step model was 24%. Statistically significant characteristics included self-esteem (β=−.28, p=.004), dementia problematic behaviors (β=.25, p=.009), and day shift (β=.34, p<.001). The second step-regression model showed the addition of social support as a factor, and the fit of the regression model was statistically significant (F=6.65, p<.001). Significant factors in the second step-regression model were, in order, self-esteem (β=−.23, p=.015), dementia problematic behaviors (β=.24, p<.010), day shift (β=.33, p<.001), and social support (β=−.19, p=.038); the explanatory power of the final model was 28% (Table 4).
This study attempted to identify the factors affecting the care burden of nurses caring for elderly patients with dementia based on the stress, appraisal, and coping theory of Lazarus and Folkman [14].
The average care burden score among our subjects was 31.16±6.62 out of 64 points. This is higher than the average score of 27.6 for the burden in professionals who work with patients with Alzheimer's disease measured using the same tool [23], and the average score of 24.3 in Song et al.[5], which measured the burden of caregivers working in nursing homes. In our study, 64.6% of the subjects were working in geriatric hospitals treating patients with severe dementia accompanied by medical or surgical diseases. This suggests that as the number of nurses caring for patients at geriatric hospitals with greater severity increases, so will the rates of caregiver burden.
We found that the factor most strongly influencing the burden of care for nurses caring for dementia patients was working day shifts, which was found to be more burdensome than rotating shifts. This is in line with the findings that nurses who work daytime work shifts are more burdened as they typically engage in bathing and caring for patients as well as administrative work and updating evaluation charts during the daytime [24]. The results suggest that the care burden of nurses working day shifts was high because the burden of day shift workers was higher than that of rotating or night shift workers. Therefore, the higher levels of care burden for day shift workers may mean that an assertive institutional support focused on day shift workers is necessary.
Dementia problematic behaviors were found to be the second most important factor influencing care burden. For the caregivers of dementia patients, the most painful experiences were those related to the behavioral and psychological symptoms of dementia (BPSD), which include aggression, wandering, and inappropriate sexual behaviors [5]. One study conducted in Korea found that BPSD constitutes a factor reducing the quality of life for families who care for dementia patients, as well as a factor that reduces the motivation to work among medical staff [25]. In the study by Kim and Lee [26], which analyzed interviews of nurses' experiences of caring for terminal-stage dementia patients, nurses indicated work-related pressure from the problematic behaviors of dementia patients. While some nurses care for the elderly with dementia based on their responsibility as nurses and understand that such activities were symptoms of dementia, it is necessary to provide knowledge of BPSD and encourage a positive attitude among these nurses through ongoing education.
The third factor that influenced the burden of care was self-esteem. Self-esteem can provide incentives to initiate change in the behavior of nurses, and can also positively influence nurses' nursing activities. These findings are consistent with studies showing that self-esteem affects nurses' burden [27], as well as results indicating that nurses with higher perceived self-esteem experience lower levels of psychological burnout [10].
The fourth factor that influenced the care burden of nurses caring for patients with dementia was social support. Caregivers of dementia patients experience psychological depression and pain almost ten times as great as that of caregivers of general patients [28]. Cooke et al.[12] indicated that social support programs such as emotional support, phone counselling, and educational psychological support reduced the burden of caregivers, as well as showing that the application of social support programs for dementia caregivers led to reductions of care burden and tension and increased quality of life over time [29]. Accordingly, social support is an important determinant in managing the burden of care for nurses providing care services to elderly patients with dementia. Therefore, to minimize the care burden of nurses dealing with elderly dementia patients, an administrative system that promotes social support may be necessary.
In this study, among the individual factors related to nurses, dementia knowledge and attitude had no significant influences on care burden. The studies by Sung et al. [9] and Hwang and Jang [30] of nursing staff and geriatric nursing home workers indicated a significant correlation between knowledge and attitude toward dementia. However, these findings were inconsistent with the findings of this study, perhaps because in our study the subjects had a high level of knowledge of dementia (83.9% correct answers) and positive scores on attitude toward dementia.
This study has limited generalizability, as the participants were selected from two hospitals and one nursing home in Gyeonggi-do using convenience sampling. Among the 150 participants of this study, 23 dropped out. We visited each institution to distribute the surveys and ensure that the results of the surveys could be received by mail. Among the collected responses, 15 participants indicated that they did not want to reply and 8 only agreed to participate in, but failed to complete the survey. Inferences regarding the no-response rates led us to believe that the survey construction of this study, which beginning by measuring the knowledge of dementia, may have burdened the participants. Since the Cronbach's α value for the scale measuring knowledge of dementia was low at .68, this must be taken into consideration in future surveys. Even though social support was included as appraisal factors, it was difficult to explain it. Therefore, there was a limitation to reflect the stress, appraisal and coping theory of Lazarus and Folkman [14].
Nevertheless, this study has identified factors of the care burden of nurses caring for elderly patients with dementia and provides information for practical nursing interventions as well as showing the importance of support based on the type of work.
This study found that the level of care burden on nurses caring for elderly patients with dementia was high and was affected by day shifts, dementia problematic behaviors, self-esteem, and social support. Thus, we found that work environment improvements that consider the work support systems and environments of nurses working during the daytime, intervention programs that include ongoing education on BPSD, and self-esteem and social support were critical factors in reducing the care burden of nurses. Based on our findings, the following recommendations are warranted: 1) An active institutional support system must be developed for daytime nurses looking after elderly patients with dementia. 2) To reduce the burden of care, education on the behavioral problems associated with dementia must be provided. 3) It is necessary to conduct an experimental study to develop an intervention program for nurses.
Figures and Tables
Table 2
Levels of Knowledge, Attitude, Self-esteem, Dementia Problematic Behaviors Social Support, and Care Burden (N=127)
References
1. Allen J, Close J. The NICHE geriatric resource nurse model: Improving the care of older adults with Alzheimer's disease and other dementias. Geriatric Nursing. 2010; 31(2):128–132. DOI: 10.1016/j.gerinurse.2010.02.006.

2. Kim KW, Park JH, Kim MH, Kim MD, Kim BJ, Kim SK, et al. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea. Journal of Alzheimer's Disease. 2011; 23(2):281–291. DOI: 10.3233/JAD-2010-101221.

3. Oh BH. Diagnosis and treatment for behavioral and psychological symptoms of dementia. Journal of the Korean Medical Association. 2009; 52(11):1048–1054. DOI: 10.5124/jkma.2009.52.11.1048.

4. Youn JC, Lee DY, Jhoo JH, Kim KW, Choo IH, Woo JI. Prevalence of neuropsychiatric syndromes in Alzheimer's Disease (AD). Archives of Gerontology and Geriatrics. 2011; 52(3):258–263. DOI: 10.1016/j.archger.2010.04.015.

5. Song JA, Park JW, Kim H. Impact of behavioral and psychological symptoms of dementia on caregiver burden in nursing homes. Journal of Korean Gerontological Nursing. 2013; 15(1):62–74.
6. Korean Ministry of Government Legislation. The enforcement regulations of the elderly welfare law [Internet]. Sejong: Korea Ministry of Government Legislation;2017. cited 2017 December 28. Available from: http://www.law.go.kr/lsBylInfoR.do?bylSeq=7179520&lsiSeq=198754&efYd=20171103.
7. Machnicki G, Allegri RF, Dillon C, Serrano CM, Taragano FE. Cognitive, functional and behavioral factors associated with the burden of caring for geriatric patients with cognitive impairment or depression: Evidence from a South American sample. International Journal of Geriatric Psychiatry. 2009; 24(4):382–389. DOI: 10.1002/gps.2133.

8. Park YH. A study on nurses' attitudes toward the elderly suffering from dementia [master's thesis]. [Seoul]: The Catholic University of Korea;2008. 60.
9. Sung MR, Kim KA, Lee DY. Factors influencing burnout in primary family caregivers of elders with dementia. Journal of Korean Gerontology Nursing. 2012; 14(3):200–208.
10. Kim HJ, Lee HR, Choi SO. Resilience to burnout, self-esteem and turnover intention of nurses in long-term care hospitals. Journal of Korean Gerontological Nursing. 2013; 12(3):218–226.
11. Kang JH. Effect of a social support program on caregivers of elders with dementia. Journal of Korean Gerontological Nursing. 2010; 12(2):142–153.
12. Cooke DD, McNally L, Mulligan KT, Harrison MJ, Newman SP. Psychosocial interventions for caregivers of people with dementia: A systematic review. Aging & Mental Health. 2001; 5(2):120–135. DOI: 10.1080/713650019.

13. Park JK, Nam GY. Moderating effects of coping styles and irrational beliefs on the relationship between caregiver's stress and cognitive and daily living functioning in the elderly with dementia. Korean Journal of Clinical Psychology. 2017; 36(3):301–314. DOI: 10.15842/kjcp.2017.36.3.002.
14. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer;1984. p. 456.
15. Kang CM, Kim JS, Jeong JH. Factors influencing quality of caregiving by caregivers for elders with dementia. Journal of Korean Academy of Community Health Nursing. 2016; 27(3):193–201. DOI: 10.12799/jkachn.2016.27.3.193.

16. Jung SM. A study on caregiver's knowledge, burden on dementia and their job satisfaction level in nursing home [master's thesis]. [Seoul]: The Catholic University of Korea;2004. 34.
17. Norbergh KG, Helin Y, Dahl A, Hellzen O, Asplund K. Nurses' attitudes towards people with dementia: The semantic differential technique. Nursing Ethics. 2006; 13(3):264–274. DOI: 10.1191/0969733006ne863oa.
18. Rosenberg M. Society and the adolescent self-image. Princeton NJ: Princeton University Press;1965. p. 326.
19. Jon BJ. Self-esteem: A test of its measurability. Yonsei Nonchong. 1974; 11(1):107–130.
20. Kim KA. Development of an assessment tool of problematic behaviors for institutionalized old people with dementia. Proceeding of the 28th Public Health Conference. Journal of Korean Academy of Public Health Nursing. 2003; 119–120.
21. House JS. Work stress and social support. Reading, MA: Addison-Wesley Publishing Company;1981. p. 156.
22. Jung HC. A study on the job stress of workers at social welfare center [master's thesis]. [Yongin]: Kangnam University;2008. 69.
23. McCarty EF, Drebing C. Burden and professional caregivers: Tracking the impact. Journal for Nurses in Professional Development. 2002; 18(5):250–257.
24. Lee JH, Park JS. End of life care stress and nursing work environment in geriatric hospitals nurses affect burn out. Journal of the Korea Academia-Industrial Cooperation Society. 2017; 18(6):449–458.
25. Lim DY. Coping with dementia related behavior problems of the elderly and care providers. Journal of the Korea Academia-Industrial cooperation Society. 2015; 16(7):4805–4815.

26. Kim CG, Lee YH. Nurses' experiences of end of life care of older adults with dementia. Korean Journal of Adult Nursing. 2017; 29(2):119–130.

27. Park SM, Jang IS, Choi JS. Affecting factors of nurses' burnout in secondary general hospitals. Journal of Korean Academy of Nursing Administration. 2011; 17(4):474–483.

28. Livingston G, Johnston K, Katona C, Paton J, Lyketsos C. Systemic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. The American Journal of Psychiatry. 2005; 162(11):1996–2021. DOI: 10.1176/appi.ajp.162.11.1996.
29. Andren S, Elmståhl S. The relationship between caregiver burden, caregivers' perceived health and their sense of coherence in caring for elders with dementia. Journal of Clinical Nursing. 2008; 17(6):790–799. DOI: 10.1111/j.1365-2702.2007.02066.x.
30. Hwang SY, Jang KS. A study on the levels of dementia-related knowledge, attitude, and practice among nursing assistants caring for institutionalized elders with dementia. Journal of Korean Academy of Adult Nursing. 1999; 11(3):378–388.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download