Abstract
Purpose
Peripheral arterial disease (PAD) is a common vascular problem and has serious morbidity and mortality in advanced situations. However, the prevalence and risk factors for PAD in Korea have not been reported. The purpose of this study was to evaluate the prevalence and risk factors of PAD in the Korean population.
Methods
The study was processed by visiting community welfare centers. Inclusion criteria were people who participated in this study. Screening was performed by history taking followed by the measurement of ankle brachial index (ABI). PAD was defined when an ABI of 0.9 or less was found in one or both legs. All statistical analyses were conducted with SPSS ver. 22.0.
Results
Between January 2008 and December 2012, a total of 2,044 participants were included with 810 men (39.6%) and 1,234 women (60.4%). PAD was detected in 95 (4.6%). Borderline ABI (0.91–0.99) showed in 212 (10.4%), and severe decreased ABI defined as 0.5 or less showed in 3 (0.1%). Significant risk factors for PAD were old age (odd ratio, 1.952; P = 0.045), hypertension (odd ratio, 1.645; P = 0.050), and cardiovascular disease (odd ratio, 2.047; P = 0.039). Significant risk factors for borderline PAD were old age (odd ratio, 1.019; P = 0.024), hypertension (odd ratio, 1.461; P = 0.038), and chronic obstructive lung disease (odd ratio, 3.393; P = 0.001).
Peripheral arterial disease (PAD) is a common vascular problem in which progressive narrowing of the arteries due to atherosclerosis reduces blood flow in the lower extremities. Previous studies have demonstrated that PAD has a significantly elevated risk of morbidity and mortality from cardiovascular disease [123]. Therefore, early diagnosis and proper management of PAD is crucial. However, PAD has been underdiagnosed and undertreated, in part, because most patients are asymptomatic or happen to present with atypical symptoms.
Most population-based prevalence studies were conducted in Western countries. In Korea, the prevalence of PAD is essentially unknown. This is thought to be primarily because of the lack of data on symptomatic or asymptomatic PAD. Moreover, most studies have focused on symptomatic or clinic-based populations and are limited to the assessment of risk factors that affect PAD [45].
However, the prevalence of asymptomatic PAD in Korea and analysis thereof according to the specific range of ABI values has not been reported. The purpose of this study was to evaluate the prevalence and risk factors of asymptomatic PAD in the Korean population.
This study was based on the data of noninstitutionalized citizens who voluntarily participated from 2008 to 2012. The study took place in 6 cities in Korea, which were Gangdong-gu of Seoul, Hanam, Uiwang, Guri, Namyangju, and Ulsan cities. A total of 3,030 participants who agreed to enroll were recruited from community welfare centers in each city. People who had previously been diagnosed with PAD or did not agree to participate were excluded. A population-based sample of 2,044 was included. Visits to each community center were made for history taking, completion of a questionnaire, and physical examination. Past medical history, familial history, and personal medical history were also obtained for the evaluation of risk factors for PAD.
This study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong, Seoul, Korea (KHMNC 2010-019). The Institutional Review Board waived the need of participant's consent due to no information of participant's identification.
For diagnosis of PAD, the participant was required to rest for at least 5 minutes. Afterwards, a standard blood pressure cuff was placed around the ankles and arms. The subject was laid in the supine position. The systolic blood pressure (SBP) in the bilateral arms (Brachial) was measured. The systolic pressures of the posterior tibial (PT) artery or, if absent, the dorsalis pedis artery of bilateral ankles was also measured. The ankle brachial index (ABI) was calculated by dividing the ankle SBP by the higher brachial one. The ABI was used to classify participant into 4 categories; PAD was defined as an ABI of 0.9 or less in either lower extremity [26], Borderline PAD was defined as an ABI 0.90 to 0.99, severe PAD was lower than 0.5 in either lower extremity.
Body mass index (BMI) was defined as body weight in kilograms divided by height in meters squared. Hypertension was defined as an SBP over 140 mmHg and/or diastolic blood pressure over 90 mmHg in an individual currently taking antihypertensive medication. Other past medical history, familial history, and social history were obtained based on a self-reported questionnaire completed either before or after the measurement of blood pressure. Diabetes, hyperlipidemia, pulmonary disease, cardiovascular disease (previous myocardial infarction, angina, and heart failure), cerebrovascular disease (stroke and transient ischemic attack) and chronic kidney disease (decreased renal function despite treatment or on dialysis) were examples of past medical history. A smoker was defined in cases who have smoked at least a hundred cigarettes during their life and defined on the basis of self-report. A positive history for drinking was defined as a person who drank more than half a bottle of beer twice per week. Exercise was defined by when they had a regular exercise plan such as walking, cycling, stair climbing, tiptoe raises, dancing, or static/dynamic leg exercises for more than 30 minutes.
Baseline characteristics such as demographics, medical history, and social history were summarized. Measurable parameters were expressed as mean ± standard deviation and analyzed by a chi-square test or paired t-test. Descriptive statistics were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). P-value < 0.05 was considered statistically significant.
The characteristics of the study population are summarized in Table 1. A total of 2,044 subjects were enrolled in this study. Among them, the female population was 1,234 (60.4%). The mean age of the enrolled population was 67.3 ± 9.1 years (range, 26–100 years). The mean BMI was 24.4 ± 3.1 kg/m2 (range, 15.9–40.6 kg/m2). As the risk factors for the development of PAD, hypertension was most common followed by hyperlipidemia, diabetes, cardiovascular disease, cerebrovascular disease, chronic obstructive pulmonary disease, and chronic kidney disease. Stroke was the most common in terms of family history. About one-third of the subjects were smokers and drinkers.
The prevalence of PAD and borderline PAD by age groups were shown in Table 2. Among 2,044 participants, PAD was detected in 95 (4.6%). Among the 95 subjects with ABI ≤ 0.90, 3 subjects (0.1%) were diagnosed with severe PAD. PAD was detected most commonly in age group ≥ 80 years (12; 9.0%), followed by 70–79 years (41; 5.3%), 60–69 years (29; 3.8%) and 50–59 years (10; 3.2%). Borderline PAD in the population was detected in 212 (10.4%). The mean ABI decreased with age, incrementally.
Table 3 shows the distribution of risk factors among those individuals with and without PAD. The PAD group was almost 2 years older than the non-PAD group (69.4 years vs. 67.2 years, P = 0.025). The BMI was higher in the PAD group with statistical significance. The typical risk factors such as hypertension (P < 0.001), diabetes (P = 0.004), hyperlipidemia (P = 0.011), and history of cardiovascular disease (P = 0.001) were more common in PAD group. As part of social history, smoking was more common in the PAD group (47.4% vs. 32.9%, P = 0.003).
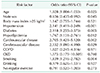
Table 4 shows the odds ratio of risk factors for PAD by univariate analysis. The history of cardiovascular disease was highly associated with PAD (odds ratio [OR], 2.705; 95% confidence interval [CI], 1.429–5.120; P = 0.002). Other risk factors such as old age (OR, 1.028; 95% CI, 1.004–1.053; P = 0.025), male gender (OR, 0.656; 95% CI, 0.435–0.992; P = 0.045), hypertension (OR, 2.141; 95% CI, 1.411–3.249; P < 0.001), diabetes (OR, 2.118; 95% CI, 1.255–3.573; P = 0.005), hyperlipidemia (OR, 1.767; 95% CI, 1.131–2.761, P = 0.012), and smoking (OR, 1.839; 95% CI, 1.216–2.782; P = 0.004) showed significant risk factor for the development of PAD.
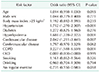
The univariate analysis for borderline PAD is shown in Table 5. The history of COPD was highly associated with borderline PAD (OR, 3.227; 95% CI, 1.588–6.559; P = 0.001). In addition, hypertension (OR, 1.712; 95% CI, 1.270–2.307; P < 0.001), hyperlipidemia (OR, 1.688; 95% CI, 1.228–2.322, P = 0.001), and cardiovascular disease (OR, 2.042; 95% CI, 1.211–3.441; P = 0.007) were statistically significant risk factors.
Multivariate analysis adjusted for age, sex, BMI, self-reported past medical histories and social histories were done. Table 6 shows the multivariate analyses for PAD and borderline PAD adjusted for variables previously mentioned and results were presented as OR. Old age (OR, 1.952; 95% CI, 0.520–7.330; P = 0.045), hypertension (OR, 1.645; 95% CI, 0.996–2.718; P = 0.050), and history of cardiovascular disease (OR, 2.047; 95% CI, 1.038–4.036; P = 0.039) remained statistically significant for PAD. For borderline PAD, old age (OR, 1.019; 95% CI, 1.003–1.037; P = 0.024), hypertension (OR, 1.461; 95% CI, 1.020–2.091; P = 0.038), and history of COPD (OR, 3.393; 95% CI, 1.503–7.178; P = 0.001) were significant risk factors for borderline PAD.
As the population ages, PAD is likely to become an increasing issue. Previous prevalence estimates for PAD have derived individuals from hospital settings, which would be expectedly overestimated because of the concern of disease in the general population. In particular, studies published in Korea have mostly reviewed the prevalence of PAD in association with risk factors such as history of ischemic heart disease, stroke, and smoking. These studies including only under a hundred people cannot be applied to the population because of selection bias and the small scale of the studies [457]. We selected welfare centers in order to represent the population while minimizing selection bias. The total number of participants was increased to create a larger-scale research.
In earlier epidemiological studies carried out in Western countries on adult populations, which used same diagnostic criteria, the prevalence of PAD was about 4.5% [38]. In the present study, the prevalence of PAD in Korean adults was 4.6%. When the prevalence of PAD was compared with that of Western countries, it showed a similar prevalence in the Korean population.
The results of the present study showed that PAD disproportionately affects older individuals. This is consistent with previous studies [7910]. We also demonstrated that there was a particularly high prevalence of PAD among smokers than in persons who are nonsmokers. The smokers were divided into ‘yes (ex- and current smokers)’ and ‘no’ and this factor was analyzed as well. We formed the questionnaire to determine either former or current smoker. Interestingly, we were able to confirm that the accumulation of smoking being associated with a higher risk of PAD was consistent with previous studies [4111213].
The results of the present study showed that PAD was in fact not associated with “traditional” cardiovascular risk factors such as diabetes, hyperlipidemia, and status of smoking in multivariate analysis. This result showed discordance with previous studies [1415161718]. Explanation to clarify these results was as of yet insufficient. However, we found the reason in the methods. The use of self-reported data for past medical history could underestimate the prevalence because most of these patients received management from hospitals rather than community welfare centers in Korea. Further studies are needed to clarify this association.
Borderline PAD, in which ABI was 0.91 to 0.99, was associated with increased risk of premature death and severe events [19]. The current study revealed that the prevalence of borderline PAD was 10.4%, and this is comparable to previous studies with 8.7% of prevalence in reports of United States (US) adults > 40 years of age [20]. Prior studies mentioned persons with borderline PAD showing higher rates of functional decline such as mobility loss and progress to walk for 6 minutes continuously at 5-year follow-up [51321]. Furthermore, according to previous reports, borderline PAD itself was a risk factor for cardiovascular disease even after modification of other traditional cardiovascular risk factors [78]. Our study shows the prevalence of asymptomatic borderline PAD was 10.4% of the population with a much higher prevalence in older populations (11.4% and 16.9% in 70s and 80s, respectively). Our study will contribute to early diagnosis and active treatment for persons with borderline PAD, and may result in improved functional outcome and reduce the risk of cardiovascular disease.
In addition, we conducted analyses on severe PAD with an ABI < 0.5. Diagnosis of severe PAD and timely treatment for these patients is extremely important because it has a significant impact in the aspects of medical cost, patient morbidity, and patient's quality of life. Previously published studies showed that severe PAD is associated with severe complications such as limb loss, and is associated with a higher mortality rate. Our study showed the prevalence of severe PAD was 0.1%, which is lower than the rate of the report of the US population by Baxter et al. [22] at 0.32%. We had no subgroup analysis on these severe PAD groups compared with borderline ABI or normal ABI groups because this study focused on the epidemiology of PAD according to ABI values. We speculated that the root of this finding was our study design. Our study was conducted based on community welfare centers in big cities only. Therefore, there is a possibility that people who are more interested in health, and who manage their health, have participated and have a tendency to be sensitive and well-managed in health. If we collect the data from small cities or rural communities with differences in diet and lifestyle, the prevalence may be different. We hope future study will cover this area.
There were several limitations that deserve consideration before application of these results to the population. The first limitation was that the designated locations in our study included only metropolitan areas. Secondly, the people who visit welfare centers tend to have a higher interest in health and are in a relatively better physical condition. Because of this form of bias, our study results are likely to underestimate the observed associations between risk factors and PAD. Thus, we cannot claim that the results of this study are an accurate representation of the Korean general population.
However, this study was carried out on a large scale with a total of 2,044 participants and this statistical power allowed the differences between the subject groups to be clarified. Furthermore, although the results of this study are similar with previous studies, our study included a substantially younger population. Therefore, regardless of these limitations, this study can provide an important description of PAD prevalence and risk factors in the Korean population.
In conclusion, the prevalence of PAD was 4.6% in the Korean population. Aging and history of cardiovascular disease were the significant risk factors of PAD. Also, borderline PAD was found in 10.4% of the population, and old age, hypertension, and COPD were significant risk factors. Severe PAD was found in 0.1% of the population. Further study is needed on a national scale.
Figures and Tables
References
1. Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilson PW, et al. The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham Study. Arch Intern Med. 2003; 163:1939–1942.
2. Newman AB, Shemanski L, Manolio TA, Cushman M, Mittelmark M, Polak JF, et al. Ankle-arm index as a predictor of cardiovascular disease and mortality in the Cardiovascular Health Study. The Cardiovascular Health Study Group. Arterioscler Thromb Vasc Biol. 1999; 19:538–545.
3. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004; 110:738–743.

4. Lee YH, Shin MH, Kweon SS, Choi JS, Rhee JA, Ahn HR, et al. Cumulative smoking exposure, duration of smoking cessation, and peripheral arterial disease in middle-aged and older Korean men. BMC Public Health. 2011; 11:94.

5. Rhee SY, Guan H, Liu ZM, Cheng SW, Waspadji S, Palmes P, et al. Multi-country study on the prevalence and clinical features of peripheral arterial disease in Asian type 2 diabetes patients at high risk of atherosclerosis. Diabetes Res Clin Pract. 2007; 76:82–92.

6. McDermott MM. Ankle brachial index as a predictor of outcomes in peripheral arterial disease. J Lab Clin Med. 1999; 133:33–40.

7. Ahn S, Park YJ, Min SI, Kim SY, Ha J, Kim SJ, et al. High prevalence of peripheral arterial disease in Korean patients with coronary or cerebrovascular disease. J Korean Med Sci. 2012; 27:625–629.

8. Fowkes FG, Housley E, Cawood EH, Macintyre CC, Ruckley CV, Prescott RJ. Edinburgh Artery Study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1991; 20:384–392.

9. De Backer G, Kornitzer M, Sobolski J, Denolin H. Intermittent claudication--epidemiology and natural history. Acta Cardiol. 1979; 34:115–124.
10. Reid DD, Brett GZ, Hamilton PJ, Jarrett RJ, Keen H, Rose G. Cardiorespiratory disease and diabetes among middle-aged male Civil Servants. A study of screening and intervention. Lancet. 1974; 1:469–473.
11. Belch JJ, Topol EJ, Agnelli G, Bertrand M, Califf RM, Clement DL, et al. Critical issues in peripheral arterial disease detection and management: a call to action. Arch Intern Med. 2003; 163:884–892.
12. Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001; 344:1608–1621.

13. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001; 286:1317–1324.

14. Landray MJ, Thambyrajah J, McGlynn FJ, Jones HJ, Baigent C, Kendall MJ, et al. Epidemiological evaluation of known and suspected cardiovascular risk factors in chronic renal impairment. Am J Kidney Dis. 2001; 38:537–546.

15. Lüscher TF, Creager MA, Beckman JA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Circulation. 2003; 108:1655–1661.
16. McDermott MM, Green D, Greenland P, Liu K, Criqui MH, Chan C, et al. Relation of levels of hemostatic factors and inflammatory markers to the ankle brachial index. Am J Cardiol. 2003; 92:194–199.

17. O'Hare A1, Johansen K. Lower-extremity peripheral arterial disease among patients with end-stage renal disease. J Am Soc Nephrol. 2001; 12:2838–2847.
18. Ridker PM, Stampfer MJ, Rifai N. Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA. 2001; 285:2481–2485.
19. Diehm N, Diehm C. Subclinical atherosclerosis of lower limb arteries: a strong predictor for cardiovascular mortality. Eur Heart J. 2006; 27:2495–2496.

20. Menke A, Muntner P, Wildman RP, Dreisbach AW, Raggi P. Relation of borderline peripheral arterial disease to cardiovascular disease risk. Am J Cardiol. 2006; 98:1226–1230.

21. McDermott MM, Guralnik JM, Tian L, Liu K, Ferrucci L, Liao Y, et al. Associations of borderline and low normal ankle-brachial index values with functional decline at 5-year follow-up: the WALCS (Walking and Leg Circulation Study). J Am Coll Cardiol. 2009; 53:1056–1062.

22. Baxter AR, Jacobowitz GR, Guo Y, Maldonado T, Adelman MA, Berger JS, et al. Increased Prevalence of Moderate and Severe Peripheral Arterial Disease in the American Indian (AI)/Alaskan Native (AN) Population; a Study of 96,000 AI/AN. Ann Vasc Surg. 2017; 38:177–183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download