Abstract
Purpose
We aimed to compare clinical outcomes after carotid endarterectomy (CEA) between Korean patients with and without severe contralateral extracranial carotid stenosis or occlusion (SCSO).
Methods
Between January 2004 and December 2014, a total of 661 patients who underwent 731 CEAs were stratified by SCSO (non-SCSO and SCSO groups) and analyzed retrospectively. The study outcomes included the occurrence of major adverse cardiovascular events (MACE), defined as stroke or myocardial infarction, and all-cause mortality during the perioperative period and within 4 years after CEA.
Results
There were no significant differences in the incidence of MACE or any individual MACE manifestations between the 2 groups during the perioperative period or within 4 years after CEA. On multivariate analysis to identify clinical variables associated with long-term study outcomes, older age (hazard ratios [HRs], 1.06; 95% confidence intervals [CIs], 1.03–1.09; P < 0.001) and diabetes mellitus (HR, 1.71; 95% CI, 1.14–2.57; P = 0.010) were significantly associated with an increased risk of MACE occurrence, while preexisting SCSO was not associated with long-term incidence of MACE and individual MACE components. Kaplan-Meier survival analysis showed similar MACE-free (P = 0.509), overall (P = 0.642), and stroke-free (P = 0.650) survival rates in the 2 groups.
Cerebrovascular accidents are a major cause of morbidity and mortality worldwide, causing a heavy financial burden. There may be ethnic disparities in the incidence of mortality and morbidity of stroke and coronary heart disease [1]; in South Korea, it was observed that stroke incidence was higher than the incidence of myocardial infarction (MI) [2]. Although both carotid endarterectomy (CEA) and carotid artery stenting (CAS) are established as effective treatment options for the prevention of cerebrovascular events in symptomatic and asymptomatic patients with severe carotid bifurcation stenosis [34567], it could be expected that CEA provides a greater benefit than CAS for these patients in the Korean population [8]. However, the reported effects of severe contralateral extracranial carotid stenosis or occlusion (SCSO) on the perioperative and long-term outcomes of CEA are variable from previous studies. Several multicenter clinical trials have reported an increased risk of perioperative stroke after CEA in both symptomatic and asymptomatic patients with preexisting SCSO [9], while many single-center studies found comparable perioperative results for patients with and without SCSO [10].
In this study, we aimed to compare early and late outcomes after CEA between Korean patients with and without SCSO. We also investigated the clinical outcomes according to the presence of contralateral extracranial carotid occlusion (occlusion vs. nonocclusion), preexisting stroke symptoms (symptomatic vs. asymptomatic carotid stenosis), and anesthetic technique (regional vs. general anesthesia).
In this single-center, retrospective observational study, we analyzed data extracted from the medical records of patients receiving CEA. The study protocol was approved by the Institutional Review Board of Asan Medical Center (2018-1467), and the requirement for informed patient consent was waived given the retrospective nature of the study.
Between January 1, 2004, and December 31, 2014, a total of 772 consecutive patients who underwent 853 CEAs at our hospital were screened for inclusion in this study. Of these patients, 111 patients (122 CEAs) who were followed up at other hospitals were excluded to ensure that the impact of SCSO after CEA on early and late outcomes in patients with aggressive risk factor control, specifically, was analyzed. We ultimately included 661 patients (731 CEAs, 85.7%) stratified by SCSO (non-SCSO group vs. SCSO group) and analyzed them retrospectively. All CEAs had been performed to relieve significant carotid bifurcation stenosis, as defined by velocity criteria, based on peak systolic velocity (PSV) and end-diastolic velocity values recorded from within the most stenotic segment. The diagnoses were also guided by criteria established by the North American Symptomatic Carotid Endarterectomy Trial (NASCET) [511].
The criteria were as follows, using carotid duplex ultrasonography (DUS): 50%–99% luminal narrowing in patients with symptomatic carotid stenosis, and >70% in those with asymptomatic carotid stenosis. Patients were considered to be symptomatic if they had transient ischemic attacks, amaurosis fugax, or non-disabling stroke ipsilateral to significant carotid stenosis within the previous 6 months [1213]. In cases of discrepancy in the degree of carotid stenosis determined using velocity criteria and luminal narrowing based on the NASCET criteria, the estimation of carotid stenosis was based primarily on the velocity criteria [11]. In patients with bilateral carotid bifurcation stenosis, the first side for operation (ipsilateral) was determined according to the following priority criteria: the presence of neurological symptoms, the degree of carotid stenosis, the presence of asymptomatic cerebral infarcts, and the dominant cerebral hemisphere [1214]. The most symptomatic or higher-grade carotid artery stenosis was identified as the primary lesion (the ipsilateral lesion) and was treated first, and the less symptomatic or lower-grade carotid artery stenosis was referred to as the contralateral lesion [12]. Of the included patients, SCSO was defined as >70% luminal narrowing of the contralateral extracranial carotid stenosis or occlusion based on the DUS diagnostic criteria described above.
Demographics, risk factors, and other data, including clinical characteristics and 30-day and 4-year outcomes, were recorded for all consecutive patients in an Excel (Microsoft Corp., Redmond, WA, USA) database and retrospectively analyzed.
The surgical procedures were performed as previously detailed [1213]. CEA was performed under general anesthesia with routine carotid shunting or regional anesthesia with selective shunting. During the early period of our study, CEA was preferably performed in awake patients under regional anesthesia with selective shunting based on the tolerance of carotid artery cross-clamping, assessed by evaluating the level of consciousness and motor function. Motor function and consciousness tests included counting numbers and squeezing a squeaking rubber doll placed in the contralateral hand. General anesthesia was selectively used for patients who did not tolerate regional anesthesia, while in the late period, we changed the anesthetic technique for general anesthesia with routine shunting. In patients who received regional anesthesia, a carotid shunt was inserted immediately when speech or motor dysfunction developed after carotid artery cross-clamping [13]. The preferred option for CEA was an endarterectomy with patch angioplasty in the standard fashion as previously described [1213]. Postoperatively, all patients were given dual antiplatelet therapy with a statin in combination with stringent blood pressure control and close observation in an intensive care unit for at least 24 hours. All patients were followed up both clinically and by magnetic resonance imaging with angiography before discharge.
Follow-up included carotid DUS to assess patency and exclude the development of new or contralateral lesions, as well as independent neurological examination using the National Institutes of Health Stroke Scale [15] and the modified Rankin scale at 6 months, 12 months, and annually [1213]. Once stability had been established over 3 years, surveillance was performed at longer intervals of about 2 years [1213].
The study outcomes of interest were the occurrences of major adverse cardiovascular events (MACE), defined as fatal or nonfatal stroke or MI, and all-cause mortality during the perioperative period (within 30 days after CEA) and within 4 years after CEA. Only the first event of each outcome was included in the analysis.
Postoperative stroke diagnosis was based on the World Health Organization (WHO) definition of acute, focal, occasionally global, loss of neurological function lasting for 24 hours or more, with a vascular etiology [16]. The diagnosis was categorized as major or minor as previously detailed [1213]. MI was defined as previously described [121317]. Peripheral arterial occlusive disease (PAOD) was defined as a previous history of any therapeutic interventions for PAOD or an ankle-brachial index ≤0.9, measured using Doppler ultrasound [18]. Following CEA, restenosis was diagnosed based on DUS criteria, defined as >70% luminal narrowing with a PSV threshold of ≥274 cm/sec [19]. The diagnosis of subclinical coronary artery disease (CAD) was based on preoperative radionuclide adenosine stress myocardial perfusion imaging, and additional coronary computed tomography angiography or coronary angiography in patients without a history of CAD, as described previously [172021].
Categorical variables are reported as frequencies or percentages, and continuous variables are reported as means and standard deviations. Differences between the 2 groups were compared using chi-square test or Fisher exact test for categorical variables and Student t-test for continuous variables. Univariate and multivariate logistic regression analyses were used to identify the association between clinical variables and perioperative outcomes (within 30 days after CEA), and odds ratios with 95% confidence intervals (CIs) are reported. Long-term event-free rates in terms of MACE-free, overall, and stroke-free survival rates in the 2 groups were estimated with Kaplan-Meier analysis and were compared with estimations calculated using the log-rank test. Univariate and multivariate analyses of the association between clinical variables and long-term outcomes (within 4 years after CEA) were conducted with Cox proportional hazards modeling, using the event of interest and the period from CEA to the date of the event or last follow-up as the outcome. Univariate Cox proportional hazard regression models were fitted to calculate hazard ratios (HRs) with 95% CIs to estimate the associations between clinical variables and outcomes. Variables with a P-value of <0.1 on univariate analysis were included in the multivariate analysis. A P-value <0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA).
The study cohort consisted of 661 patients who received 731 CEAs at our hospital. The non-SCSO group consisted of 625 patients with 651 CEAs (89.1%), and the SCSO group consisted of 80 patients with 80 CEAs (10.9%). During the study period, staged bilateral CEAs were performed on 70 patients: 26 CEAs in the non-SCSO group and 44 CEAs in the SCSO group. Of the patients in the SCSO group who underwent staged bilateral CEAs, the first CEA on the primary (ipsilateral) lesion was included in the SCSO group, and the second CEA (on the contralateral lesion) following the first CEA was included in the non-SCSO group.
The 2 groups did not differ significantly in demographic characteristics, risk factors, or clinical characteristics, except that the patients in the SCSO group were more likely to have subclinical CAD (2.6% vs. 8.8%, P = 0.011). However, there was no significant difference in CAD history between the 2 groups (19.0% vs. 21.3%, P = 0.638) (Table 1). Additional coronary computed tomography angiography or coronary angiography conducted on 24 patients with subclinical CAD indicated 1-, 2-, or 3-vessel disease in 8 (33.3%), 7 (29.2%), and 9 patients (37.5%), respectively. According to our management strategy as detailed elsewhere [22], 11 patients (45.8%) received medical treatment, 4 (16.7%) received staged percutaneous coronary intervention followed by CEA, and 9 (37.5%) received staged CEA followed by coronary artery bypass graft. There were no significant differences in the anesthetic (P = 0.580), reconstruction techniques (P = 0.999), and rates of intraoperative shunt placement (P = 0.865) between the 2 groups. Among the patients undergoing CEA under regional anesthesia with selective shunting, no significant difference was noted in the rate of shunt placement in the SCSO group (5 of 38 patients, 13.2%) compared with the non-SCSO group (27 of 288 patients, 9.4%) (P = 0.398).
Patients with and without SCSO did not differ significantly in the incidence of MACE occurrence during the perioperative period (2.2% vs. 3.8%, P = 0.418) or within 4 years after CEA (12.4% vs. 15.0%, P = 0.517) (Table 2). There were no significant differences between the 2 groups in any of the individual MACE manifestations. Clinical variables associated with perioperative outcomes were analyzed using univariate and multivariate logistic regression analyses; for the incidence of MACE and individual MACE manifestations, the univariate analysis identified no statistically significant factor, which precluded the execution of multivariate analysis (Supplementary Table 1).
Univariate and multivariate Cox proportional hazards regression analyses were performed to identify clinical variables associated with long-term outcomes. After adjustment for potential confounding variables, multivariate analysis of the association between clinical variables and long-term incidence of MACE indicated that older age (HR, 1.06; 95% CI, 1.03–1.09; P < 0.001) and diabetes mellitus (HR, 1.71; 95% CI, 1.14–2.57; P = 0.010) were independent predictors of an increased risk of MACE occurrence (Table 3). For the analyses of the association between clinical variables and individual MACE manifestations, older age (HR, 1.08; 95% CI, 1.05–1.12; P < 0.001) was significantly associated with an increased mortality rate within 4 years after CEA, while hypertension (HR, 0.51; 95% CI, 0.30–0.85; P = 0.010) was independently associated with a decreased 4-year mortality rate (Supplementary Table 2). There was no statistically significant factor associated with an increased 4-year incidence stroke or MI (Supplementary Table 3). Preexisting SCSO was not associated with long-term overall MACE incidence or with any of the individual MACE manifestations.
The mean duration of follow-up was 68.7 ± 34.2 months (median, 66 months; range, 12–167 months): 68.4 ± 33.9 months (median, 66 months; range, 12–166 months) in the non-SCSO group and 70.6 ± 36.1 months (median, 65 months; range, 13–167 months) in the SCSO group. Kaplan-Meier survival analysis showed similar MACE-free (P = 0.509), overall (P = 0.642), and stroke-free (P = 0.650) survival rates in the 2 groups (Fig. 1). During the study period, restenosis was noted in 15 CEAs (2.1%): 13 CEAs (2.0%) in the non-SCSO group and 2 CEAs (2.5%) in the SCSO group (P = 0.675). There was no restenosis-related stroke.
We performed subgroup analysis based on the presence of contralateral extracranial carotid occlusion (occlusion vs. nonocclusion) (Supplementary Table 4), preexisting stroke symptoms (symptomatic vs. asymptomatic carotid stenosis) (Supplementary Table 5), and anesthetic technique (regional vs. general anesthesia) (Supplementary Table 6). In terms of the contralateral extracranial carotid occlusion, preexisting stroke symptoms, and anesthetic technique, there were no significant between-group differences in overall MACE incidence or the incidence of any of the individual MACE manifestations.
It is well known that CEA is a reliable procedure for preventing recurrent neurological symptoms and strokes in patients with significant carotid artery stenosis [5623]. However, there is some controversy about the early and late efficacy of CEA in patients with SCSO, because previous related studies have had relatively small sample sizes and significant variability in anesthetic and surgical techniques [2224]. A recent meta-analysis of patients with contralateral carotid occlusion undergoing CEA indicated that the presence of contralateral carotid occlusion results in higher rates of preoperative symptoms and increases the perioperative risk of neurological complications after CEA, but it does not have a significant impact on perioperative mortality or stroke-free survival at 5 years [24]. However, findings from most clinical trials in Western populations may not be directly applicable to Asians because there may be ethnic differences in environmental and genetic factors, in addition to differences in anatomical characteristics and the prevalence of extracranial carotid lesions [1]. According to data from the WHO's Department of Measurement and Health Information, there is a significant difference in the risk of MACE between different ethnic groups; stroke incidence is higher than MI incidence in Asian populations, which contrasts with Western populations [12].
This study cohort consisted of only Korean Asians and may not be representative of other ethnic groups. However, this may be both a limitation and a unique benefit of this study because there are limited data on benefits after CEA in Asian populations with SCSO. Our major finding was that the cumulative risk of MACE occurrence and individual MACE manifestations were similar between the non-SCSO and SCSO groups. SCSO did not have a significant impact on 30-day or 4-year outcomes following CEA in these patients. These findings are inconsistent with previously reported results involved in Western populations [2225]. Although our study sample size was small, with the SCSO group comprising only 10.9% of the entire cohort, potentially contributing to type I error, the discrepancies between our findings and those of previous studies are likely attributable in part to ethnic disparities between Asian and Western populations. As limited data are available in Asian populations, our findings help inform clinicians on the best treatments for Asian SCSO patients undergoing CEA. Further studies with larger cohorts are needed to better understand the impact of SCSO on clinical outcomes following CEA in Asian populations.
In patients with SCSO, the impaired cerebral hemodynamic status may contribute to an increased risk of perioperative stroke following CEA, even if the patients are asymptomatic, and there are no structural brain changes on neuroimaging. This is likely because of decreased cerebral perfusion, particularly after carotid cross-clamping, in patients with compromised collateral cerebral circulation [22]. Several studies monitoring cerebral perfusion during CEA have reported an inverse correlation between cerebral collateral perfusion pressure and degree of contralateral carotid artery stenosis, as well as a significantly higher rate of intraoperative shunt placement in patients with SCSO [2224252627]. According to the General Anesthesia versus Local Anesthesia for carotid surgery trial, there was no definite difference in outcome between general and local anesthesia for carotid surgery [28].
In our study, CEA was performed under either regional anesthesia with selective shunting, or general anesthesia with routine shunting. Among the patients undergoing CEA under regional anesthesia with selective shunting, our study showed similar rates of intraoperative shunting in the SCSO group compared with the non-SCSO group, and there was no significant difference in perioperative outcomes between the 2 groups. Although there is no agreement as to which methods of protection are optimal, cerebral protection is extremely important during CEA in patients with SCSO [24]. Our results suggest that timely use of carotid shunting during CEA could reduce the occurrence of perioperative MACE in patients with SCSO.
Preexisting SCSO could have a considerable impact on late outcomes after CEA because of the adverse effects of an increased overall burden of cardiovascular risk in patients with SCSO. Recently, Patel et al. [22] reported that SCSO was an independent predictor of late mortality, with long-term survival rates significantly worse for patients with SCSO in addition to significantly higher rates of perioperative MI. The authors found that SCSO was an additional marker of higher systemic cardiovascular disease burden, and was associated with significantly higher rates of early and late MACE occurrence after CEA [22]. Similar findings were reported in high-risk patients eligible for the Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy (SAPPHIRE) trial [29]. In contrast, we found that preexisting SCSO was not associated with an increased risk of perioperative or long-term MACE incidence in patients undergoing CEA. Our study included only patients who were followed up at our hospital with aggressive risk factor control. Although we cannot conclude causality, as with all observational studies, this potentially explained our observation of no significant differences in early and late outcomes after CEA between the non-SCSO and SCSO groups.
It is clear that our study has substantial limitations, including its retrospective design and small sample size in a single-center cohort. Therefore, there was potential for selection and information biases on the part of the physicians or patients. Indication bias and patient self-selection for anesthetic technique may have also influenced our findings. There are other important factors not available in our data sources, such as intracranial carotid lesions with the status of collateral vertebrobasilar circulation, plaque morphology, and intraoperative monitoring of cerebral perfusion, which may have explained some of the differences in outcome compared with other studies. Furthermore, the study cohort consisted entirely of Korean Asians; therefore, these results may not be generalizable to other Asians or other ethnic groups. Finally, this study was likely underpowered to detect the effect of certain risk factors on outcomes and to validate the association of SCSO with early and late outcomes after CEA. Despite these limitations, our data add to the discussion of SCSO effects on early and late outcomes after CEA in contemporary literature.
In our study, there were no significant differences in overall MACE incidence or incidence of individual MACE manifestations after CEA between the non-SCSO and SCSO groups. Moreover, preexisting SCSO was not associated with an increased risk of perioperative or long-term incidence of MACE after CEA. Patients with SCSO undergoing CEA may benefit from the timely placement of intraoperative shunting, aggressive perioperative hemodynamic management, and adequate postoperative risk factor control.
Figures and Tables
Fig. 1
Kaplan-Meier analyses of the cumulative event-free rates. Major adverse cardiovascular event (MACE)-free (A), overall (B), and stroke-free survival (C) rates in patients, with and without severe contralateral extracranial carotid stenosis or occlusion (SCSO), who underwent carotid endarterectomy.

Table 1
Baseline demographics and clinical characteristics of the study patients according to the severe contralateral extracranial carotid stenosis or occlusion (SCSO) status
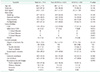
Table 2
MACE in patients undergoing CEA according to SCSO status

Values are presented as number (%).
MACE, major adverse cardiovascular events; CEA, carotid endarterectomy; MI, myocardial infarction; SCSO, severe contralateral extracranial carotid stenosis or occlusion.
a)Including the occurrence of MACE during the perioperative period. b)Any stroke, myocardial infarction, or death.
References
1. Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702–2709.
2. Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA. 1999; 282:2149–2155.
3. Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010; 363:11–23.

4. Silver FL, Mackey A, Clark WM, Brooks W, Timaran CH, Chiu D, et al. Safety of stenting and endarterectomy by symptomatic status in the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST). Stroke. 2011; 42:675–680.

5. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Barnett HJM, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991; 325:445–453.

6. European Carotid Surgery Trialists' Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet. 1991; 337:1235–1243.
7. Skerritt MR, Block RC, Pearson TA, Young KC. Carotid endarterectomy and carotid artery stenting utilization trends over time. BMC Neurol. 2012; 12:17.

8. Lee J, You JH, Oh SH, Shin S, Kim BM, Kim TS, et al. Outcomes of stenting versus endarterectomy for symptomatic extracranial carotid stenosis: a retrospective multicenter study in Korea. Ann Vasc Surg. 2019; 54:185–192.e1.

9. Gasecki AP, Eliasziw M, Ferguson GG, Hachinski V, Barnett HJ. Long-term prognosis and effect of endarterectomy in patients with symptomatic severe carotid stenosis and contralateral carotid stenosis or occlusion: results from NASCET. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. J Neurosurg. 1995; 83:778–782.
10. Kretz B, Abello N, Astruc K, Terriat B, Favier C, Bouchot O, et al. Influence of the contralateral carotid artery on carotid surgery outcome. Ann Vasc Surg. 2012; 26:766–774.

11. Kwon H, Kim HK, Kwon SU, Lee SW, Kim MJ, Park JW, et al. Risk of major adverse cardiovascular events in subjects with asymptomatic mild carotid artery stenosis. Sci Rep. 2018; 8:4700.

12. Kim A, Kwon TW, Han Y, Kwon SU, Kwon H, Noh M, et al. Clinical outcomes of staged bilateral carotid endarterectomy for bilateral carotid artery stenosis. Ann Surg Treat Res. 2015; 89:261–267.

13. Kim JH, Cho YP, Kwon TW, Kim H, Kim GE. Ten-year comparative analysis of bovine pericardium and autogenous vein for patch angioplasty in patients undergoing carotid endarterectomy. Ann Vasc Surg. 2012; 26:353–358.

14. Marrocco-Trischitta MM, Melissano G, Kahlberg A, Setacci F, Abeni D, Chiesa R. Increased incidence of cerebral clamping ischemia during early contralateral carotid endarterectomy. J Vasc Surg. 2006; 43:1155–1161.

15. Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989; 20:864–870.

16. Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980; 58:113–130.
17. Kwon H, Moon DH, Han Y, Lee JY, Kwon SU, Kang DW, et al. Impact of subclinical coronary artery disease on the clinical outcomes of carotid endarterectomy. J Neurosurg. 2017; 126:1560–1565.

18. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45 Suppl S:S5–S67.

19. AbuRahma AF, Stone P, Deem S, Dean LS, Keiffer T, Deem E. Proposed duplex velocity criteria for carotid restenosis following carotid endarterectomy with patch closure. J Vasc Surg. 2009; 50:286–291.

20. Berman DS, Abidov A, Kang X, Hayes SW, Friedman JD, Sciammarella MG, et al. Prognostic validation of a 17-segment score derived from a 20-segment score for myocardial perfusion SPECT interpretation. J Nucl Cardiol. 2004; 11:414–423.
21. Kim YH, Ahn JM, Park DW, Song HG, Lee JY, Kim WJ, et al. Impact of ischemia-guided revascularization with myocardial perfusion imaging for patients with multivessel coronary disease. J Am Coll Cardiol. 2012; 60:181–190.

22. Patel PB, LaMuraglia GM, Lancaster RT, Clouse WD, Kwolek CJ, Conrad MF, et al. Severe contralateral carotid stenosis or occlusion does not have an impact on risk of ipsilateral stroke after carotid endarterectomy. J Vasc Surg. 2018; 67:1744–1751.

23. Cunningham EJ, Bond R, Mehta Z, Mayberg MR, Warlow CP, Rothwell PM, et al. Long-term durability of carotid endarterectomy for symptomatic stenosis and risk factors for late postoperative stroke. Stroke. 2002; 33:2658–2663.

24. Cheng W, Lu H, Hu Y. Influence of contralateral carotid occlusion on outcomes after carotid endarterectomy: a meta-analysis. J Stroke Cerebrovasc Dis. 2018; 27:2587–2595.

25. Kang J, Conrad MF, Patel VI, Mukhopadhyay S, Garg A, Cambria MR, et al. Clinical and anatomic outcomes after carotid endarterectomy. J Vasc Surg. 2014; 59:944–949.

26. Chiriano J, Abou-Zamzam AM Jr, Nguyen K, Molkara AM, Zhang WW, Bianchi C, et al. Preoperative carotid duplex findings predict carotid stump pressures during endarterectomy in symptomatic but not asymptomatic patients. Ann Vasc Surg. 2010; 24:1038–1044.

27. AbuRahma AF, Mousa AY, Stone PA, Hass SM, Dean LS, Keiffer T. Correlation of intraoperative collateral perfusion pressure during carotid endarterectomy and status of the contralateral carotid artery and collateral cerebral blood flow. Ann Vasc Surg. 2011; 25:830–836.

28. GALA Trial Collaborative Group. Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008; 372:2132–2142.
SUPPLEMENTARY MATERIAL
Supplementary Tables 1–6 can be found via https://www.astr.or.kr/src/sm/astr-97-202-s001.pdf.
Supplementary Table 4
Incidence of MACE during the perioperative period and within 4 years after CEA according to contralateral extracranial CO




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download