1. Modlin IM, Sandor A. An analysis of 8305 cases of carcinoid tumors. Cancer. 1997; 79:813–829.

2. Caplin ME, Buscombe JR, Hilson AJ, Jones AL, Watkinson AF, Burroughs AK. Carcinoid tumour. Lancet. 1998; 352:799–805.

3. Godwin JD 2nd. Carcinoid tumors. An analysis of 2,837 cases. Cancer. 1975; 36:560–569.
4. Yang K, Cheng YS, Yang JJ, Jiang X, Guo JX. Primary hepatic neuroendocrine tumor with multiple liver metastases: a case report with review of the literature. World J Gastroenterol. 2015; 21:3132–3138.

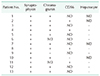
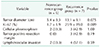
5. Qiu MJ, Chen YB, Bi NR, Yang SL, He XX, Xiong ZF. Comparative clinical analysis of gastroenteropancreatic neuroendocrine carcinomas with liver metastasis and primary hepatic neuroendocrine carcinomas. Dis Markers. 2018; 2018:9191639.

6. Creutzfeldt W, Stockmann F. Carcinoids and carcinoid syndrome. Am J Med. 1987; 82(5B):4–16.

7. Huang YQ, Xu F, Yang JM, Huang B. Primary hepatic neuroendocrine carcinoma: clinical analysis of 11 cases. Hepatobiliary Pancreat Dis Int. 2010; 9:44–48.
8. Oberg K. Neuroendocrine gastrointestinal tumors--a condensed overview of diagnosis and treatment. Ann Oncol. 1999; 10 Suppl 2:S3–S8.
9. Shetty PK, Baliga SV, Balaiah K, Gnana PS. Primary hepatic neuroendocrine tumor: an unusual cystic presentation. Indian J Pathol Microbiol. 2010; 53:760–762.

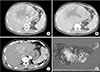
10. Kellock T, Tuong B, Harris AC, Yoshida E. Diagnostic imaging of primary hepatic neuroendocrine tumors: a case and discussion of the literature. Case Rep Radiol. 2014; 2014:156491.

11. Wang LX, Liu K, Lin GW, Jiang T. Primary hepatic neuroendocrine tumors: comparing CT and MRI features with pathology. Cancer Imaging. 2015; 15:13.

12. Kim JE, Lee WJ, Kim SH, Rhim H, Song HJ, Park CK. Three-phase helical computed tomographic findings of hepatic neuroendocrine tumors: pathologic correlation with revised WHO classification. J Comput Assist Tomogr. 2011; 35:697–702.
13. Li RK, Zhao J, Rao SX, Chen CZ, Zeng MS, Qiang JW. Primary hepatic neuroendocrine carcinoma: MR imaging findings including preliminary observation on diffusion-weighted imaging. Abdom Imaging. 2013; 38:1269–1276.

14. Yalav O, Ulku A, Akçam TA, Demiryurek H, Doran F. Primary hepatic neuroendocrine tumor: five cases with different preoperative diagnoses. Turk J Gastroenterol. 2012; 23:272–278.

15. Oberg K. Diagnostic work-up of gastroenteropancreatic neuroendocrine tumors. Clinics (Sao Paulo). 2012; 67 Suppl 1:109–112.

16. Rocca A, Calise F, Marino G, Montagnani S, Cinelli M, Amato B, et al. Primary giant hepatic neuroendocrine carcinoma: a case report. Int J Surg. 2014; 12 Suppl 1:S218–S221.

17. Oberg K, Eriksson B. Nuclear medicine in the detection, staging and treatment of gastrointestinal carcinoid tumours. Best Pract Res Clin Endocrinol Metab. 2005; 19:265–276.
18. Gabriel S, Garrigue P, Dahan L, Castinetti F, Sebag F, Baumstark K, et al. Prospective evaluation of
68Ga-DOTATATE PET/CT in limited disease neuroendocrine tumours and/or elevated serum neuroendocrine biomarkers. Clin Endocrinol (Oxf). 2018; DOI:
10.1111/cen.13745. [Epub].
19. Hwang S, Lee YJ, Lee SG, Kim CW, Kim KH, Ahn CS, et al. Surgical treatment of primary neuroendocrine tumors of the liver. J Gastrointest Surg. 2008; 12:725–730.

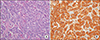
20. Brown DC, Gatter KC. Ki67 protein: the immaculate deception? Histopathology. 2002; 40:2–11.

21. Bahra M, Jacob D, Pascher A, Plockinger U, Kristiansen G, Neuhaus P, et al. Surgical strategies and predictors of outcome for malignant neuroendocrine tumors of the pancreas. J Gastroenterol Hepatol. 2007; 22:930–935.

22. Knox CD, Anderson CD, Lamps LW, Adkins RB, Pinson CW. Long-term survival after resection for primary hepatic carcinoid tumor. Ann Surg Oncol. 2003; 10:1171–1175.

23. Zhang A, Xiang J, Zhang M, Zheng S. Primary hepatic carcinoid tumours: clinical features with an emphasis on carcinoid syndrome and recurrence. J Int Med Res. 2008; 36:848–859.

24. Le Treut YP, Delpero JR, Dousset B, Cherqui D, Segol P, Mantion G, et al. Results of liver transplantation in the treatment of metastatic neuroendocrine tumors. A 31-case French multicentric report. Ann Surg. 1997; 225:355–364.
25. Lehnert T. Liver transplantation for metastatic neuroendocrine carcinoma: an analysis of 103 patients. Transplantation. 1998; 66:1307–1312.
26. Fenwick SW, Wyatt JI, Toogood GJ, Lodge JP. Hepatic resection and transplantation for primary carcinoid tumors of the liver. Ann Surg. 2004; 239:210–219.

27. Kress O, Wagner HJ, Wied M, Klose KJ, Arnold R, Alfke H. Transarterial chemoembolization of advanced liver metastases of neuroendocrine tumors--a retrospective single-center analysis. Digestion. 2003; 68:94–101.
28. Varker KA, Martin EW, Klemanski D, Palmer B, Shah MH, Bloomston M. Repeat transarterial chemoembolization (TACE) for progressive hepatic carcinoid metastases provides results similar to first TACE. J Gastrointest Surg. 2007; 11:1680–1685.

29. Krishnamurthy SC, Dutta V, Pai SA, Kane SV, Jagannath P, Desouza LJ, et al. Primary carcinoid tumor of the liver: report of four resected cases including one with gastrin production. J Surg Oncol. 1996; 62:218–221.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download