Abstract
Background
Classical Hodgkin lymphoma (cHL) is a clinicopathologically unique, aggressive lymphoma arising from germinal center B-cells and is one of the most curable hematological malignancies. This study aimed to determine the clinical course, treatment regimens, response rates, and survival data of patients diagnosed with cHL in a tertiary center.
Methods
A retrospective review was conducted to include patients with a diagnosis of cHL from 2013 to 2017. Data of demographic and clinical characteristics, treatment regimens, and outcomes were collected and analyzed.
Results
We recruited 94 patients with a median age of 27.0 [interquartile range (IQR), 12] years. Most of the patients were male (61.7%) and 73.4% were ethnic Malay. Nodular sclerosis was the most common histology (77.6%), followed by mixed cellularity (6.4%) and others (16%). The median follow-up time was 28.0 (IQR, 32) months. All patients received chemotherapy but only 13.8% received radiotherapy as consolidation. The doxorubicin-bleomycin-vinblastine-dacarbazine regimen was the most common (85.1%), followed by the escalated bleomycin-etoposide-doxorubicin-cyclophosphamide-vincristineprednisolone-procarbazine regimen (14.9%). Following treatment, 76.1% of patients achieved complete response. The 2-year overall survival (OS) and progression-free survival (PFS) of the entire cohort were 96.5% and 71.1%, respectively. The 2-year OS and PFS for advanced-stage disease were 93.9% and 62.8%, compared to 100% and 82.7% for early-stage disease, respectively (P=0.252 and P=0.052, respectively).
Hodgkin lymphoma (HL) is a clinicopathologically unique, aggressive lymphoma, originating from germinal center B cells. HL is one of the most curable of all hematological malignancies. With an annual incidence of 2–3 per 100,000, it accounts for 0.5% of all new cancers diagnosed in the United States [1]. There are huge variations in the epidemiologic and clinicopathological characteristics in relation to geographical and socioeconomic status. Although bimodal age distribution is common among industrialized countries, the disease appears predominantly during childhood in developing countries and its incidence decreases with age [2].
HL is classified into two major types: classical HL (cHL) and nodular lymphocyte-predominant HL, accounting for 95% and 5% of all HL cases, respectively [3]. Classical HL is further subdivided into four major histological subtypes: nodular sclerosis, lymphocyte-rich, lymphocyte-depleted, and mixed-cellularity [4]. The combination of different, highly effective treatment modalities has led to progressive improvements in outcomes and higher long-term cure rates [5]. The use of intensive chemotherapy regimens as first-line treatments has shown additional benefits with regards to progression-free survival, compared to conventional chemotherapy with ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine), for advanced-stage cHL [6].
In Malaysia, the crude incidence rate for HL from 2007 to 2011 was reported as 0.6 and 0.4 for men and women, respectively [7]. Unfortunately, there is a lack of outcome data for HL patients treated in Malaysia. Therefore, this study was designed to determine the clinical course, treatment regimens, response rates, and survival data for patients diagnosed with cHL in our large tertiary center. Different treatment regimens were compared retrospectively to obtain the survival benefit and progression-free survival. This study aims to improve the management of HL for our future patients. To the best of our knowledge, this is the first published study evaluating clinical features and treatment outcomes for HL in Malaysia.
Patients aged 13 years and older who were diagnosed with cHL between January 2013 and December 2017 in the main tertiary referral hospital in Johor, Malaysia, were recruited in this retrospective study. A total of 120 patients were diagnosed with HL during this period; of these, 1 patient with nodular lymphocyte-predominant Hodgkin lymphoma and 1 patient with a composite tumor (with diffuse large B-cell lymphoma) were excluded. Records for 10 patients were either missing or incomplete. Among the remaining 108 patients, 14 were not included in the outcome analysis for the following reasons: 8 withdrew from front-line treatment, 4 did not receive any treatment (patients declined), and 2 transferred to other centers for treatment, leaving 94 patients available for outcome analysis. This study was registered with the National Medical Research Register, Malaysia, and the ethical approval for this study was obtained from the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia.
Demographic data, presenting symptoms, routine laboratory and histopathology results, staging, treatment plans, and treatment outcomes were reviewed from patients' records. Pathological specimens were classified according to the World Health Organization (WHO) classification [4]. Patients were staged according to the Ann Arbor Staging system [8]. Staging procedures used, including data of history, clinical examination, contrast-enhanced computed tomography (CECT) or positron emission tomography (PET-CT), and bone marrow examination, were recorded. Bulky disease was defined as lymph node mass >10 cm in diameter or mediastinal mass exceeding one-third of the maximum chest cavity on an upright posteroanterior chest radiograph or CECT [9]. Patients with stage I, IIA, and IIB (non-bulky with no extranodal disease) were considered to have early-stage disease. Those with stage IIB (bulky or with extranodal disease), III, and IV disease were considered to have advanced-stage disease. Patients with advanced-stage disease were also classified according to the International Prognostic Score (IPS) [10]. This score considers 7 risk factors that have been shown to be associated with failure-free survival and overall survival: age >45 years, male sex, stage IV disease, albumin level <4 g/dL, hemoglobin level <10.5 g/dL, white cell counts >15,000/µL, and lymphocyte counts <600/µL or 8% of the white cell count [10]. Patients with 2 or fewer risk factors were considered low-risk, while those with 3 or more were considered high-risk. The treatment modality and chemotherapy regimens were recorded and use of adjuvant radiotherapy was documented.
The treatment plan for patients with early-stage cHL was 6 cycles of ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy with or without consolidative radiotherapy. In advanced-stage disease, patients were treated with either ABVD chemotherapy or escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, prednisolone, procarbazine) with interim PET-CT assessment. Consolidative radiotherapy was administered at the end of chemotherapy for bulky tumors or localized end of treatment PET-CT positivity. Escalated BEACOPP was utilized in our center beginning in November 2016. Interim PET-CT was performed for assessment, and patients with a good response were de-escalated to ABVD for the subsequent cycles. Due to resource constraints and long waiting lists, patients would receive 2–4 cycles of escalated BEACOPP prior to PET-CT assessment. Patients with refractory or relapsed disease were administered salvage chemotherapy, followed by high-dose therapy and autologous stem cell transplantation, when possible. Salvage therapy included ICE (ifosfamide, carboplatin, etoposide), DHAP (dexamethasone, cytarabine, cisplatin), and GDP (gemcitabine, cisplatin, dexamethasone). As brentuximab vedotin was not routinely available in our center, only selected patients received it as maintenance therapy post autologous stem cell transplantation.
Responses were defined according to the revised response criteria for lymphoma [11]. Imaging evaluations included both CECT and PET-CT. Progression was defined as relapse or failure to achieve complete response (CR). Overall survival (OS) was calculated from the date of diagnosis to the date of death or last contact. Progression-free survival (PFS) was calculated from the date of diagnosis until the date of progression or death or last contact.
The data collected were analyzed using the Statistical package for the Social Sciences (SPSS) version 22 (SPSS Inc., Chicago, IL, USA). Categorical data were expressed as frequencies with percentages and continuous data were expressed as mean±standard deviation. Survival was estimated by the Kaplan-Meier method. Potential prognostic factors (age, sex, B symptoms, bulky disease, extranodal disease, clinical stages, and IPS) for OS and PFS were screened by applying the two-sided log-rank test. A multivariate cox proportional hazard model was used to identify independent predictors. All P-values were 2-sided and P-values <0.05 were considered statistically significant.
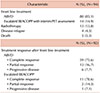
Ninety-four patients were included in this retrospective study with a median age of 27 years (IQR, 12) at diagnosis. The baseline characteristics of these patients are shown in Table 1. There was an early peak in young adults aged 15 to 30 years without a second peak at a later age group. Fifty-eight patients (61.7%) were men, and the male to female ratio was 1.61:1. Most of the patients were ethnic Malay (73.4%) followed by Chinese (14.9%), and Indian (10.6%). The most common presentation was palpable lymph node mass (81.4%) and 73.4% had B symptoms upon diagnosis. Thirty-four (36.2%) patients had bulky disease and 26 (27.7%) had extranodal involvement.
Nodular sclerosis (77.6%) was the most common histological subtype followed by unclassified cHL (14.9%), and mixed cellularity (6.4%). Only one patient had lymphocyte-rich HL, and none had a lymphocyte-depleted subtype. One patient presented with stage I disease, 49 (52.1%) patients presented with stage II, 20 (21.3%) with stage III, and 24 (25.5%) with stage IV disease. Among these patients, 56 (59.6%) had advanced-stage disease, while 38 (40.4%) had early-stage disease.
All patients received chemotherapy. Eighty patients (85.1%) were started on ABVD as first-line treatment, while 14 (14.9%) began with escalated BEACOPP. Among patients with advanced-stage disease, 43 patients received ABVD, while 13 patients received escalated BEACOPP as their first-line treatment (Table 2).
Thirteen patients (13.8%) received radiotherapy (RT) as consolidation post chemotherapy. Thirteen patients underwent autologous stem cell transplantation following salvage chemotherapy in relapsed refractory disease and 5 patients received brentuximab vedotin (BV) maintenance post transplantation.
During front-line therapy, 2 patients died due to disease progression. Among the 92 patients evaluated after front-line treatment, 70 patients (76.1%) achieved CR, 15 (16.3%) had partial response (PR), and 7 patients (7.6%) had progressive disease. The CR rates for early and advanced disease were 84.2% and 70.4%, respectively. Among patients with advanced disease receiving ABVD, the CR rate was 68.3%, compared to 76.9% with escalated BEACOPP.
With a median follow-up duration of 28 months (IQR, 32), the 2-year overall survival (Fig. 1A) and 2-year progression-free survival (Fig. 1B) rates were 96.5% and 71.1%, respectively. The 2-year OS for early and advanced disease were 100% and 93.9%, respectively (P=0.252) (Fig. 2A). The 2-year PFS for early and advanced disease were 82.7% and 62.8%, respectively (P=0.052) (Fig. 2B). Twenty-one patients received salvage chemotherapy (DHAP, ICE, GDP or a combination of the three) following disease progression, partial response, or relapsed disease. Three (14.3%) of these patients died: 2 from disease progression despite salvage therapy and 1 from neutropenic sepsis. Three of the 4 patients who had relapsed after attaining remission achieved a second remission following salvage chemotherapy and autologous stem cell transplantation. Among patients with advanced disease, 12-month OS rates were 94.9% and 100%, respectively, for patients receiving ABVD and escalated BEACOPP (P=0.763) (Fig. 3A), while the 12-month PFS rates were 69.1% and 75.5%, respectively (P=0.427) (Fig. 3B).
The results from log-rank tests for PFS and OS are shown in Table 3. Among the potential risk features and clinical characteristics studied, only extranodal disease had a significant impact on the 5-year PFS (P=0.002) in univariable analysis. Otherwise, none of the other studied features had significant effects on the OS and PFS for our cohort. Extranodal disease remained the independent prognostic factor for poorer PFS under the multivariate cox proportional hazards model (Table 4).
Within our cohort, 5 patients developed neutropenic sepsis during treatment, 3 developed pulmonary fibrosis secondary to bleomycin, and 1 developed cardiomyopathy secondary to anthracycline. No secondary malignancies after treatment were documented in any of the patients.
In our retrospective study, we describe disease presentation and treatment outcomes for HL patients in our center in Malaysia. A bimodal age-specific incidence pattern, with a relatively high proportion of cases in adolescents and young adults, is commonly observed in Western industrialized countries [2]. However, we observed an early peak in young adults without a bimodal age distribution in our cohort and similar findings were also reported among Hong Kong Chinese patients diagnosed with HL [12]. Nodular sclerosis was the most common histological subtype found in our patients followed by mixed cellularity. This is more approximate to the pattern in developed countries in contrast to the developing world, where the mixed cellularity type has been reported to be predominant [13].
More than half of our patients (52.1%) presented with stage II disease and the rest (46.8%) presented with stage III and IV disease. In studies from United States and Europe, 60 to 70% of the patients had early-stage disease (stage I and IIA) [14], while advanced-stage disease is more common among patients from developing countries [151617]. Several factors may contribute to this observation. Firstly, lack of awareness in our population may lead to a delay in diagnosis when the patient notices lymph node masses. Moreover, some patients choose to seek complementary and alternative medicine before seeing a physician and this further delays the diagnosis. Secondly, fine needle aspiration cytology (FNAC) of an enlarged lymph node is often the first sampling investigation performed in Malaysia, but FNAC is unable to reveal the architecture of the involved lymph node; malignant HL cells are not detected by flow cytometry. Thus, FNAC is never sufficient for a new HL diagnosis [13] and may delay a definite diagnosis.
ABVD remained the most commonly used chemotherapeutic regimen in our center. Ease of outpatient administration, infrequent hospital admissions for neutropenic sepsis, and infrequent use of relatively expensive growth factors following chemotherapy are among the factors leading to its preferred use. In contrast to the recommended PET-guided regimen used in early-stage disease, 6 cycles of ABVD were commonly administered for both early- and advanced-stage disease in our center because of limited access to PET-CT. The lack of an in-house radiotherapy service has led to underutilization of RT; the option of using a single modality i.e. chemotherapy has been described in previous studies [918]. The National Cancer Institute of Canada Clinical Trials Group (NCIC CTG) HD.6 trial compared 4–6 cycles of ABVD alone with subtotal nodal irradiation, adding ABVD only in patients displaying an unfavorable risk profile. After 12 years of follow-up, both treatment approaches had identical OS with a favorable risk profile, and a small but significant OS benefit was observed in patients receiving ABVD alone without irradiation who had an unfavorable risk profile [19]. Therefore, in patients with concerns regarding late radiation toxicities, ABVD alone is a feasible approach.
Our treatment outcomes were comparable with studies published in developed countries for early-stage disease (early favorable and unfavorable) [1920], but inferior for advanced-stage disease [62122]. Among patients with advanced-stage disease, a smaller cohort with a shorter duration of follow-up who started on escalated BEACOPP showed no statistically significant differences in outcomes compared to our study. However, we observed a higher percentage of patients achieving CR (76.9%) compared to ABVD (62.8%). Most of the studies have concluded more intensive chemotherapy such as escalated BEACOPP in advanced-stage disease would lead to a better progression-free survival without a marked improvement in overall survival [23242526]. One of the possible reasons for this is the availability of effective salvage chemotherapy followed by high dose therapy and autologous stem cell transplantation. Longer follow-up for complications, especially secondary malignancy, will be important for this group of patients as recent long-term follow-up from the HD15 trial reported 10-year cumulative incidence rates of second cancers at 7% and 10% for patients treated with 6 and 8 cycles of escalated BEACOPP, respectively [27].
We investigated the relationship of several disease risk features and patients' clinical characteristics, including age, B symptoms, disease stage, LDH levels, bulky disease, and extranodal disease with OS and PFS. Generally, only extranodal disease emerged as a significant prognostic factor in our cohort. The absence of clinical significance between survival and disease stages or IPS is likely due to the short follow-up duration.
This study is limited by its retrospective nature and short follow-up period. Our documentation of long-term monitoring for secondary malignancy or cardiovascular and lung complications from chemotherapy and radiotherapy was not comprehensive. This is important as part of the treatment outcome. Although this is a single center study, it provides insight into the clinical presentation and treatment outcomes among patients with HL in Malaysia. A longer follow-up would be important to discover differences in outcomes with various chemotherapeutic regimens.
Figures and Tables
 | Fig. 2Kaplan-Meier survival curve for 2-year OS and PFS for patients with early-stage and advanced-stage disease. |
 | Fig. 3Kaplan-Meier survival curve for 12-month OS and PFS for patients treated with ABVD and escalated BEACOPP as first-line treatment in newly diagnosed HL. |
ACKNOWLEDGMENTS
The authors would like to thank the Director General of Health Malaysia for permission to publish this paper.
References
1. National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. Cancer stat facts: Hodgkin lymphoma, 2018. Bethesda, MD: National Cancer Institute;2018. Accessed March 20, 2019. at https://seer.cancer.gov/statfacts/html/hodg.html.
2. Thomas RK, Re D, Zander T, Wolf J, Diehl V. Epidemiology and etiology of Hodgkin's lymphoma. Ann Oncol. 2002; 13 Suppl 4:147–152.

3. Kuppers R. New insights in the biology of Hodgkin lymphoma. Hematology Am Soc Hematol Educ Program. 2012; 2012:328–334.

4. Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. Lyon, France: IARC Press;2017.
5. Canellos GP, Niedzwiecki D, Johnson JL. Long-term follow-up of survival in Hodgkin's lymphoma. N Engl J Med. 2009; 361:2390–2391.

6. Spinner MA, Advani RH. Risk-adapted therapy for advancedstage Hodgkin lymphoma. Hematology Am Soc Hematol Educ Program. 2018; 2018:200–206.

7. Azizah AM, Nor Saleha IT, Noor Hasimah A, Asmah ZA, Mastulu W. Malaysian National cancer registry report 2007 – 2011. Putrajaya, Malaysia: National Cancer Institute, Ministry of Health Malaysia;2016. Accessed March 20, 2019. at https://www.crc.gov.my/wp-content/uploads/documents/report/MNCRRrepor2007-2011.pdf.
8. Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M. Report of the Committee on Hodgkin's Disease Staging Classification. Cancer Res. 1971; 31:1860–1861.
9. Shamoon RP, Ali MD, Shabila NP. Overview and outcome of Hodgkin's Lymphoma: experience of a single developing country's oncology centre. PLoS One. 2018; 13:e0195629.

10. Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease. N Engl J Med. 1998; 339:1506–1514.
11. Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007; 25:579–586.

12. Law MF, Ng TY, Chan HN, et al. Clinical features and treatment outcomes of Hodgkin's lymphoma in Hong Kong Chinese. Arch Med Sci. 2014; 10:498–504.

13. Shanbhag S, Ambinder RF. Hodgkin lymphoma: a review and update on recent progress. CA Cancer J Clin. 2018; 68:116–132.

14. Bazzeh F, Rihani R, Howard S, Sultan I. Comparing adult and pediatric Hodgkin lymphoma in the Surveillance, Epidemiology and End Results Program, 1988-2005: an analysis of 21 734 cases. Leuk Lymphoma. 2010; 51:2198–2207.

15. Avagyan A, Danielyan S, Voskanyan A, et al. Treating adults with Hodgkin lymphoma in the developing world: a hospital-based cohort study from Armenia. Asian Pac J Cancer Prev. 2016; 17:101–104.

16. Shafi RG, Al-Mansour MM, Kanfar SS, et al. Hodgkin lymphoma outcome: a retrospective study from 3 tertiary centers in Saudi Arabia. Oncol Res Treat. 2017; 40:288–292.

17. Arya LS, Dinand V, Thavaraj V, et al. Hodgkin's disease in Indian children: outcome with chemotherapy alone. Pediatr Blood Cancer. 2006; 46:26–34.

18. Jain S, Kapoor G, Bajpai R. ABVD-based therapy for Hodgkin lymphoma in children and adolescents: lessons learnt in a tertiary care oncology center in a developing country. Pediatr Blood Cancer. 2016; 63:1024–1030.

19. Meyer RM, Gospodarowicz MK, Connors JM, et al. ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med. 2012; 366:399–408.

20. Brockelmann PJ, Sasse S, Engert A. Balancing risk and benefit in early-stage classical Hodgkin lymphoma. Blood. 2018; 131:1666–1678.

21. Johnson P, Federico M, Kirkwood A, et al. Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s lymphoma. N Engl J Med. 2016; 374:2419–2429.

22. Gallamini A, Tarella C, Viviani S, et al. Early chemotherapy intensification with escalated BEACOPP in patients with advanced-stage Hodgkin lymphoma with a positive interim positron emission tomography/computed tomography scan after two ABVD cycles: long-term results of the GITIL/FIL HD 0607 trial. J Clin Oncol. 2018; 36:454–462.

23. Merli F, Luminari S, Gobbi PG, et al. Long-term results of the HD2000 trial comparing ABVD versus BEACOPP versus COPP-EBV-CAD in untreated patients with advanced Hodgkin lymphoma: a study by Fondazione Italiana Linfomi. J Clin Oncol. 2016; 34:1175–1181.

24. Carde P, Karrasch M, Fortpied C, et al. Eight cycles of ABVD versus four cycles of BEACOPPescalated plus four cycles of BEACOPPbaseline in stage III to IV, international prognostic score ≥ 3, high-risk Hodgkin lymphoma: first results of the phase III EORTC 20012 intergroup trial. J Clin Oncol. 2016; 34:2028–2036.

25. Viviani S, Zinzani PL, Rambaldi A, et al. ABVD versus BEACOPP for Hodgkin's lymphoma when high-dose salvage is planned. N Engl J Med. 2011; 365:203–212.

26. Cerci JJ, Pracchia LF, Linardi CC, et al. 18F-FDG PET after 2 cycles of ABVD predicts event-free survival in early and advanced Hodgkin lymphoma. J Nucl Med. 2010; 51:1337–1343.

27. Engert A, Goergen H, Markova J, et al. Reduced-intensity chemotherapy in patients with advanced-stage Hodgkin lymphoma: updated results of the open-label, international, randomised phase 3 HD15 trial by the German Hodgkin Study Group. HemaSphere. 2017; 1:e5.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download