1. Rodriguez RM, Anglin D, Langdorf MI, Baumann BM, Hendey GW, Bradley RN, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013; 148(10):940–946.
2. Rodriguez RM, Langdorf MI, Nishijima D, Baumann BM, Hendey GW, Medak AJ, et al. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015; 12(10):e1001883.

3. Young M, Marrie TJ. Interobserver variability in the interpretation of chest roentgenograms of patients with possible pneumonia. Arch Intern Med. 1994; 154(23):2729–2732.

4. Albaum MN, Hill LC, Murphy M, Li YH, Fuhrman CR, Britton CA, et al. Interobserver reliability of the chest radiograph in community-acquired pneumonia. Chest. 1996; 110(2):343–350.

5. Ketai L, Malby M, Jordan K, Meholic A, Locken J. Small nodules detected on chest radiography: does size predict calcification? Chest. 2000; 118(3):610–614.
6. Shah PK, Austin JH, White CS, Patel P, Haramati LB, Pearson GD, et al. Missed non-small cell lung cancer: radiographic findings of potentially resectable lesions evident only in retrospect. Radiology. 2003; 226(1):235–241.

7. Ojutiku O, Haramati LB, Rakoff S, Sprayregen S. Radiology residents' on-call interpretation of chest radiographs for pneumonia. Acad Radiol. 2005; 12(5):658–664.
8. Gourin CG, Watts TL, Williams HT, Patel VS, Bilodeau PA, Coleman TA. Identification of distant metastases with positron-emission tomography-computed tomography in patients with previously untreated head and neck cancer. Laryngoscope. 2008; 118(4):671–675.

9. Testa A, Soldati G, Copetti R, Giannuzzi R, Portale G, Gentiloni-Silveri N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit Care. 2012; 16(1):R30.

10. Kelly BS, Rainford LA, Darcy SP, Kavanagh EC, Toomey RJ. The development of expertise in radiology: in chest radiograph interpretation,“expert” search pattern may predate “expert” levels of diagnostic accuracy for pneumothorax identification. Radiology. 2016; 280(1):252–260.
11. Mehrotra P, Bosemani V, Cox J. Do radiologists still need to report chest x rays? Postgrad Med J. 2009; 85(1005):339–341.

12. Melbye H, Dale K. Interobserver variability in the radiographic diagnosis of adult outpatient pneumonia. Acta Radiol. 1992; 33(1):79–81.

13. McAdams HP, Samei E, Dobbins J 3rd, Tourassi GD, Ravin CE. Recent advances in chest radiography. Radiology. 2006; 241(3):663–683.

14. Girvin F, Ko JP. Pulmonary nodules: detection, assessment, and CAD. AJR Am J Roentgenol. 2008; 191(4):1057–1069.

15. Li F, Engelmann R, Doi K, MacMahon H. Improved detection of small lung cancers with dual-energy subtraction chest radiography. AJR Am J Roentgenol. 2008; 190(4):886–891.

16. MacMahon H, Li F, Engelmann R, Roberts R, Armato S. Dual energy subtraction and temporal subtraction chest radiography. J Thorac Imaging. 2008; 23(2):77–85.

17. Dobbins JT 3rd, McAdams HP. Chest tomosynthesis: technical principles and clinical update. Eur J Radiol. 2009; 72(2):244–251.

18. Oda S, Awai K, Suzuki K, Yanaga Y, Funama Y, MacMahon H, et al. Performance of radiologists in detection of small pulmonary nodules on chest radiographs: effect of rib suppression with a massive-training artificial neural network. AJR Am J Roentgenol. 2009; 193(5):W397–402.

19. Li F, Hara T, Shiraishi J, Engelmann R, MacMahon H, Doi K. Improved detection of subtle lung nodules by use of chest radiographs with bone suppression imaging: receiver operating characteristic analysis with and without localization. AJR Am J Roentgenol. 2011; 196(5):W535–41.

20. Li F, Engelmann R, Pesce L, Armato SG 3rd, Macmahon H. Improved detection of focal pneumonia by chest radiography with bone suppression imaging. Eur Radiol. 2012; 22(12):2729–2735.

21. Suzuki K, Abe H, MacMahon H, Doi K. Image-processing technique for suppressing ribs in chest radiographs by means of massive training artificial neural network (MTANN). IEEE Trans Med Imaging. 2006; 25(4):406–416.

22. Freedman MT, Lo SC, Seibel JC, Bromley CM. Lung nodules: improved detection with software that suppresses the rib and clavicle on chest radiographs. Radiology. 2011; 260(1):265–273.

23. Li F, Engelmann R, Pesce LL, Doi K, Metz CE, Macmahon H. Small lung cancers: improved detection by use of bone suppression imaging--comparison with dual-energy subtraction chest radiography. Radiology. 2011; 261(3):937–949.

24. Schalekamp S, van Ginneken B, Meiss L, Peters-Bax L, Quekel LG, Snoeren MM, et al. Bone suppressed images improve radiologists' detection performance for pulmonary nodules in chest radiographs. Eur J Radiol. 2013; 82(12):2399–2405.

25. Miyoshi T, Yoshida J, Aramaki N, Matsumura Y, Aokage K, Hishida T, et al. Effectiveness of bone suppression imaging in the detection of lung nodules on chest radiographs: relevance to anatomic location and observer's experience. J Thorac Imaging. 2017; 32(6):398–405.
26. Szucs-Farkas Z, Patak MA, Yuksel-Hatz S, Ruder T, Vock P. Single-exposure dual-energy subtraction chest radiography: detection of pulmonary nodules and masses in clinical practice. Eur Radiol. 2008; 18(1):24–31.

27. Urbaneja A, Dodin G, Hossu G, Bakour O, Kechidi R, Gondim Teixeira P, et al. Added value of bone subtraction in dual-energy digital radiography in the detection of pneumothorax: impact of reader expertise and medical specialty. Acad Radiol. 2018; 25(1):82–87.
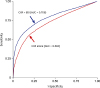
28. Dorfman DD, Berbaum KS, Metz CE. Receiver operating characteristic rating analysis. Generalization to the population of readers and patients with the jackknife method. Invest Radiol. 1992; 27(9):723–731.
29. Hillis SL, Berbaum KS, Metz CE. Recent developments in the Dorfman-Berbaum-Metz procedure for multireader ROC study analysis. Acad Radiol. 2008; 15(5):647–661.

30. Freedman MT, Osicka T. Heat maps: an aid for data analysis and understanding of ROC CAD experiments. Acad Radiol. 2008; 15(2):249–259.
31. MacMahon H, Engelmann R, Behlen FM, Hoffmann KR, Ishida T, Roe C, et al. Computer-aided diagnosis of pulmonary nodules: results of a large-scale observer test. Radiology. 1999; 213(3):723–726.

32. Quekel LG, Kessels AG, Goei R, van Engelshoven JM. Detection of lung cancer on the chest radiograph: a study on observer performance. Eur J Radiol. 2001; 39(2):111–116.

33. Monnier-Cholley L, Carrat F, Cholley BP, Tubiana JM, Arrivé L. Detection of lung cancer on radiographs: receiver operating characteristic analyses of radiologists', pulmonologists', and anesthesiologists' performance. Radiology. 2004; 233(3):799–805.

34. Del Ciello A, Franchi P, Contegiacomo A, Cicchetti G, Bonomo L, Larici AR. Missed lung cancer: when, where, and why? Diagn Interv Radiol. 2017; 23(2):118–126.











 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download