This article has been
cited by other articles in ScienceCentral.
Abstract
From December 2006 to December 2016, 1,429 patients enrolled in the Korea human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) Cohort Study were investigated. Based on the year of diagnosis, the time interval between HIV diagnosis and initiation of antiretroviral therapy (ART) was analyzed by dividing it into 2 years. The more recent the diagnosis, the more likely rapid treatment was initiated (P < 0.001) and the proportion of patients starting ART on the same day of HIV diagnosis was increased in 2016 (6.5%) compared to that in 2006 (1.7%). No significant difference in the median values of CD4+ cell counts according to the diagnosis year was observed. In the past 20 years, the time from the HIV diagnosis to the initiation of ART was significantly reduced. Rapid treatment was being implemented at the HIV diagnosis, regardless of CD4+ cell count. Considering the perspective “treatment is prevention,” access to more rapid treatment is necessary at the time of HIV diagnosis.
Keywords: HIV Infection, Antiretroviral Therapy, Rapid ART, Treatment as Prevention, National Cohort
International guidelines for human immunodeficiency virus (HIV) treatment have recently highlighted the importance of rapid treatment of HIV infection. It is known that rapid antiretroviral therapy (ART) not only reduces the mortality of HIV patients, but also improves treatment outcome.
1 In addition, a growing number of clinical trials and cohort studies indicate that ART is effective in reducing the transmission of HIV.
2 As a result, regional and global HIV prevention efforts are increasingly relying on the HIV treatment as prevention (TasP) approach to address the HIV epidemic. Treatment as early as possible is also crucial in TasP. The approach is expected to play an important role in reducing new HIV infections by transmission. Until now, there has been no emphasis on rapid treatment in HIV infection and there is no basic data on this situation in Korea. Therefore, we investigated the yearly changes in the time from HIV diagnosis to the first ART in Korea.
From December 2006 to December 2016, HIV-infected individuals enrolled in the Korea HIV/AIDS Cohort Study were evaluated. The Korea HIV/AIDS Cohort Study is a multi-centric, prospective study consisting of 15 university hospitals nationwide and managed by the Korean Centers for Disease Control and Prevention (KCDC). This cohort has an ongoing enrollment of HIV-infected adult patients older than 18 years.
Patient's baseline characteristics were investigated based on the CD4+ cell counts (< 200, 200–500, > 500). In addition, the study analyzed the changes in the time taken to start the first ART for HIV in the year of HIV diagnosis. The distribution of the time intervals from HIV diagnosis to the initiation of ART according to the year of entry into care was plotted to examine the overall pattern. Median values and interquartile ranges [IQR] of gender, age, ethnicity, time distribution (< 1 month, 1 month–1 year, > 1 year) and HIV-RNA titer (copies/mL) at the HIV diagnosis were analyzed (
Table 1). Data were expressed as median (IQR) or frequencies (%). A
P value less than 0.05 was considered statistically significant. Statistical analyses were performed using R statistics version 3.5. The present study protocol was approved by the Institutional Review Board of Kyungpook National University College of Medicine (Approval No. 2011-01-048).
There were 1,429 subjects, which included 1,322 (93.2%) men and 97 (6.8%) women. The men-to-women ratio was 13.6. The median age at the time of diagnosis was 37 years old. Most patients were of Korean ethnicity (1,414; 99%).
Of the total patients, CD4+ cell counts 200 cells/mm
3 or more were found in 950 (66.5%) and CD4+ cell counts below 200 cells/mm
3 were found in 479 (33.5%). Regardless of the year at the diagnosis, patients with low CD4+ cell counts < 200 cells/mm
3 showed a tendency to have shorter time taken from HIV diagnosis to first ART compared with the patients who have CD4+cell counts 200 cells/mm
3 or more (
Table 1). However, the total median values and interquartile ranges (IQR) of CD4+ cell count and HIV-RNA titer were 248 cells/mm
3 (IQR 104–384 cells/mm
3) and 39,668 copies/mL (IQR, 7,300–151,500 copies/mL), respectively. Moreover, there were no big differences in the median values of CD4+ cell counts and HIV-RNA titers according to the diagnosis year. It was confirmed that rapid treatment was being implemented at the HIV diagnosis, regardless of CD4+ cell count.
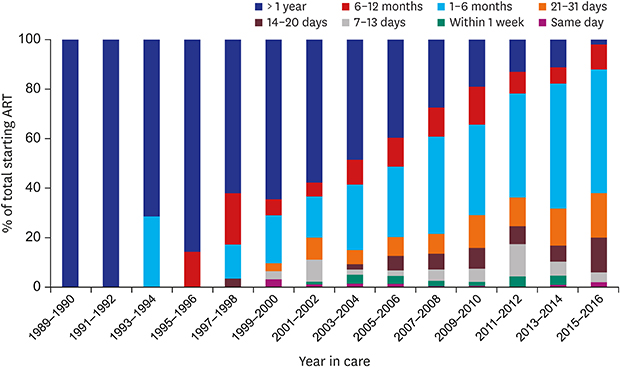
Over the years, the time from the HIV diagnosis to the initiation of ART was reduced significantly year by year; more than a 5-fold decrease was observed in 2015–2016 compared with 2005–2006 (37 days and 201 days, respectively;
P < 0.001) (
Fig. 1). The more recent the diagnosis, the more likely rapid treatment was initiated. For patients recently diagnosed in 2015–2016, the proportion of patients who began treatment within 2 weeks was still less than 10% (around 6%). Nevertheless, the proportion of patients starting treatment on the day of HIV diagnosis was increased up to 6.5% in 2016. In 2006, the proportion of patients who began ART on the same day of diagnosis, within 2 weeks, and within 1 month was measured as 1.7%, 5.1%, and 22.7%, respectively. After 10 years, when the WHO guidelines were changed, the proportion of patients who began ART on the same day of diagnosis, within 2 weeks, and within 1 month in 2016 was measured as 6.5%, 12.5%, and 50%, respectively (
Fig. 2).
Based on the Korea HIV/AIDS Cohort Study data, we found that the proportion of patients who started treatment within a month of diagnosis and the proportion of patients who started treatment at the same time have been increasing regardless of CD4+ cell counts (following the 2016 WHO guidelines).
In several randomized controlled studies, recommending ART immediately following the diagnosis of HIV has been shown to result in both earlier ART initiation and higher rates of retention in care and virologic suppression at 10–12 months compared with the standard of care without compromising safety.
345 A previous study showed that in a RAPID program, participants had earlier linkage to care, earlier ART initiation, and a shorter time to HIV RNA suppression, and high rates of virologic suppression were observed for more than 90% of the patients over a median of 1.09 years (1.09, 0–3.92 years) compared with the delayed referral group (30 days to 6 months after HIV diagnosis).
6 Currently, Rapid Initiation of Treatment (RapIT) programs are conducted in many countries around the world. A large HIV clinic in Atlanta implemented rapid access to ART on the day of the initial visit. The median time required from initial diagnosis to a HIV-1 RNA level of below 200 copies/mL was decreased from 67 days to 41 days.
7 From 2013 to 2016, a citywide rapid ART program was implemented within 5 days of diagnosis with the start of ART at the first care visit in San Francisco, and a decreasing pattern was observed in the time from diagnosis to care (38%, from 8 days to 5 days), care to ART initiation (96%, from 27 days to 1 day), and ART to first suppression (46%, from 70 days to 38 days).
89 In Korea, which does not have a rapid ART program, it has been confirmed that it takes around 37 days from diagnosis to treatment in 2015–2016, which is around 7 times longer compared with countries with a rapid ART program. It is important to develop suitable RAPID programs in Korea so that HIV patients can have access to rapid treatment at the same time following HIV diagnosis.
In the Netherlands HIV cohort study, by 2016, the median CD4+ cell count at the start of ART was increased to 410 cells/mm
3, and the majority of people started ART within 1 month of diagnosis.
10 In our study, the number of patients who started ART within a month was gradually increased up to 50% in 2016 (similar to the Netherlands cohort study). However, unlike the study in the Netherlands, a continuous annual increase in the median CD4+ cell count was not observed in our study; nevertheless, the proportion of CD4+ cell counts of 500 or more has been increased. Patients diagnosed in 2015–2016 showed that the proportion of CD4+ cell counts less than 200 cells/mm
3 still accounts for about 20% and the median value and IQR of CD4+ cells were reported to 259 (IQR, 190–363 cells/mm
3). It is possible that HIV is still not diagnosed early in Korea. A previous study also reported that the number of CD4+ cells was reported to be less than 350 cells/mm
3, accounting for around 46% of the total Korean HIV/AIDS cohort patients.
11 As early diagnosis is not easy, if diagnosed with HIV, rapid treatment is important to prevent the spread of HIV infection and to improve clinical outcomes.
1213
To achieve epidemic control, the annual number of new infections must be below the number of deaths among individuals with HIV.
14 Because no single approach can reduce the number of cases to a level required for epidemic control, improving HIV testing coverage to identify HIV-positive individuals as soon as possible after infection and linkage to care should be provided with rapid ART.
15
In conclusion, in the past 20 years, the time from HIV diagnosis to ART initiation has significantly decreased regardless of CD4+ cell counts in Korea. Since the announcement of the 2016 WHO guidelines, the rate at which treatment is initiated on the day of diagnosis has increased; however, our study found that the proportion of patients who start treatment within 1 month of diagnosis was still less than 10% in 2015–2016. Considering the perspective “treatment is prevention,” access to rapid treatment is necessary at the time of HIV diagnosis. The shorter time to viral suppression will offer both clinical benefits to HIV patients and prevention benefits to the community.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download