Measles is an airborne infectious disease that requires rigorous control measures to prevent outbreaks. Measles prevention is particularly important among healthcare workers (HCWs), because large-scale outbreaks of measles can occur in medical institutions and can result in fatalities [
1].
The United States Centers for Disease Control and Prevention (CDC) guidelines recommend that HCWs should be given 2 doses of measles-containing vaccine (MCV) [
2]. Likewise, the Korea CDC (KCDC) accepts documentation of 2 doses of measles-mumps-rubella (MMR) vaccination as confirmation of immunity among HCWs [
3]. However, there is insufficient evidence to confirm that 2 doses of MCV confer immunity.
We witnessed measles in an HCW who had received 2 doses of MCV but was anti-measles immunoglobulin G (IgG) negative. She became infected following exposure to a patient with measles. We were able to prevent further transmission by isolating the HCW. We report on this experience.
The index patient was a previously-healthy, 33-year-old male. He had traveled to Suzhou, China on August 28, 2016 and returned to Cheonan, Korea on August 31. On September 10, 2016, he visited the emergency room (ER) of Soonchunhyang university hospital, an 899-bed tertiary hospital in Cheonan, Korea. His symptoms, which had started 5 days prior to admission, included fever, sore throat, and a rash on the back of his neck. Before he was admitted to the hospital, he was found to have lesions suggestive of Koplik spots inside his mouth, but he did not have cough, coryza or conjunctivitis, the specific symptom combination that is characteristic of measles. During the patient’s initial ER visit, a doctor suspected that he had hand-foot-and-mouth disease, and isolated him in a negative-pressure room. However, the doctor in charge of the ward disagreed with this diagnosis, and the patient was released from isolation and admitted to a general multi-bed hospital room. Two days after admission, an infectious disease doctor made a clinical diagnosis of measles, and recommended that the patient have a measles laboratory test included measles polymerase chain reaction (PCR) and anti-measles IgG test. The test result was positive, and the infection control team screened all exposed HCWs, to prevent measles transmission.
Exposed HCWs were defined as HCWs working in the wards where the patient had been hospitalized, and physicians who had cared for the patient between September 10 and October 2, 2016. We traced the movement history of the patient to identify exposed HCWs, and identified 31 HCWs who had been exposed in the ER, 26 HCWs who had been exposed in the general ward, and 5 exposed radiology HCWs.
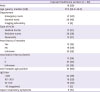
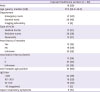
We interviewed each of the exposed HCWs to check their measles history and confirmed their MCV history based on infant scheduled immunization and checking the immunization records provided by the KCDC, and tested them for anti-measles IgG (Liaison, Saluggia, Vercelli, Italy) using a chemiluminescence immunoassay (CLIA, Saluggia, Vercelli, Italy). The characteristics of the exposed HCWs are shown in
Table 1. Of the 62 exposed HCWs, 12 (19%) had a history of measles, and 27 (44%) had received 2 doses of MCV. All except one HCW had detectable anti-measles IgG.
The HCW who was anti-measles IgG negative was a 25-year old resident nurse working in the ER. She had received 2 doses of MCV. She had only had brief contact with the index patient when measuring his blood pressure. We quarantined her, contrary to the KCDC recommendation, because we assumed that she was not immune to measles.
Fourteen days after the measles exposure, the nurse developed fever and a rash that began on the back of her neck. She had a cough but did not have any Koplik spots, coryza, or conjunctivitis. Although her respiratory symptoms could be classified as atypical measles, her skin rash resembled that of typical measles. We tested her anti-measles IgM and tested her for measles virus using PCR. Both test results were positive. We isolated her to prevent any further measles exposure of the HCWs and patients.
Although both the CDC and KCDC consider documentation of 2 doses of MCV as confirmation of immunity, the experience reveals that documentation on 2 doses of MCV does not guarantee immunity, and is insufficient for hospital infection control. In our investigation, none of the HCWs with measles IgG antibodies developed measles, but the one IgG-negative nurse became infected, despite having received 2 doses of MCV.
Measles is one of the most highly contagious human viral infections, and approximately 90% of exposed individuals become infected following exposure. According to a World Health Organization (WHO) report, 545,000 people worldwide died of measles in 2000, but the global number of deaths due to measles declined by 80% between 2000 and 2017 due to the increase in MMR vaccine coverage and increased awareness of measles infection control [
4].
In the Korea, a massive measles outbreak occurred in 2000 – 2001. The epidemic ended once 97.1% of primary or middle school students across the country had received an additional dose of MCV [
5]. Subsequently, WHO confirmed the elimination of measles in Korea. However, in 2014 there was an outbreak of measles among university students. Although the index patient had documentation of having received 2 doses of MCV, there were 143 secondary cases [
6]. Measles outbreaks have also occurred in other countries, among individuals with written confirmation of having received 2 doses of MCV [
78].
Secondary vaccine failure could not be demonstrated experimentally during the 2 previous measles outbreaks in Korea because, the measles IgG avidity test was unavailable. However, almost all of those who were eligible received a second dose of MCV in 2001, and epidemiologists determined that the vaccine was sufficiently effective to prevent a major epidemic [
5]. We propose that decreasing vaccine-induced immunity over a lengthy period, in the absence of a boosting effect of natural infection, could be the main cause of an epidemics in general [
9].
In some measles epidemics, even individuals who were considered immune to measles have become infected as a result of massive measles virus exposure [
10]. This case illustrates that measles can be transmitted to IgG-negative individuals, even when they have limited exposure and have received 2 doses of MCV. As there have been no large-scale measles epidemics in Korea since the 2000-2001 epidemic, the chance of boosting immunity by natural infection has become much smaller than in previous generations. This probably explains why the nurse was susceptible to measles, despite having received 2 doses of MCV.
Cases of measles in individuals who have previously received MCV, are generally milder than those in unvaccinated individuals. Nevertheless, such cases still require the same infection control efforts to detect contact history, and prevent further transmission as in unvaccinated cases [
11]. Recently, a hospital in Korea shut down the emergency room during a measles outbreak as an infection control measure [
12]. If we had not implemented preventive measures by isolating the nurse according to the CDC guidelines that were current at that time, there could have been additional exposed individuals, which would have made it difficult to contain spread in the hospital. Therefore, we suggest that HCWs who are anti-measles IgG-negative, should be considered non-immune, even if they have received 2 doses of the MCV. A work restriction may be one way to prevent further interruption of medical services, and further measles transmission.
In our hospital and the affiliated medical centers, it is not possible to test all HCWs for anti-measles IgG; therefore, only the HCWs who worked at the high-risk departments were tested. In addition, new employees should be tested for anti-measles IgG when they start working in the hospital. If the test is negative, the employee should be given an additional dose of MCV. When a new test was conducted on new employees and employees at high-risk departments, 92.6% were positive for anti-measles IgG. Especially in individuals aged in their 20s, anti-measles IgG was shown positive for only 87.4% of HCWs, which was below average.
In summary, we report a case of measles occurred in a nurse who had been considered to be immune to measles based only on documentation of having received 2 doses of MCV. Isolating her preemptively, prevented further exposure among non-immune individuals. We suggest that immunity of HCW to measles be confirmed by screening them for anti-measles IgG.