INTRODUCTION
Since it was first reported by Lawrence and Johnson in 1941, development of alloantibodies to factor VIII (FVIII) or factor IX (FIX) remains a great problem in the treatment of hemophilia [
1]. This condition makes bleeding control difficult and hinders prophylactic treatment; therefore, more arthropathies and disabilities are observed in patients with such inhibitors. Furthermore, the cost of treatment becomes greatly increased mainly due to the high cost of using bypassing agents [
2]. Inhibitors develop in approximately 30% of patients with hemophilia A (HA) and 1–3% of those with hemophilia B. Most inhibitors develop in patients with severe hemophilia who have mutations causing a CRM-negative state during the first (early) exposure days (EDs) to FVIII or FIX. However, inhibitors rarely develop after the first 150–200 EDs [
345]. In reference to this observation, the International Society on Thrombosis and Haemostasis (ISTH) has defined inhibitors that develop after 150 EDs as previously treated patient (PTP) inhibitors [
6].
In patients with HA, previously untreated patient (PUP) inhibitors develop at a rate of 30% per patient-year. Many patient-oriented and non-patient-oriented risk factors that may be related to the development of inhibitors have been reported [
178910]. On the contrary, PTP inhibitors in patients with HA develop at a rate of 0.1–0.6% per patient-year. Risk factors for the development of these inhibitors have not been elucidated owing to the rareness of these inhibitors and related studies [
1112]. Risk factors associated with the development of PTP inhibitors may differ from those for PUP inhibitors. Presumably, more non-patient-oriented factors may exist in patients who already have immune tolerance to factor VIII (FVIII) during the first EDs. Currently, the number of elderly patients with hemophilia is increasing owing to the increased life expectancy of patients with hemophilia, which is comparable to the life expectancy of healthy patients without hemophilia in developed countries [
1314]. Elderly patients with hemophilia have higher risk of exposure to non-patient-oriented factors such as infection, surgery, and cancer, which may break down their immune tolerance to FVIII or FIX, than in non-elderly patients with hemophilia, and PTP inhibitors may subsequently develop. Recent data in the United Kingdom (UK) support this possibility, showing a second peak of inhibitor development around the 60s in patients with severe HA (SHA), most of whom were PTPs [
15]. Therefore, it is important to elucidate the preventable risk factors related to the development of PTP inhibitors to prevent or at least decrease the incidence of these inhibitors. However, there are few studies that assess the risk factors in PTPs; consequently, the risk factors for the development of these inhibitors have not been elucidated. Therefore, this study aimed to identify risk factors for the development of inhibitors in PTPs.
MATERIALS AND METHODS
This study included patients at a hemophilia treatment center in Korea (Eulji University Hospital) who had a current record or history of alloantibodies to FVIII or FIX. Information on history of inhibitors was obtained from medical records of all patients with hemophilia registered in Eulji University Hospital from 2000 to 2018. An inhibitor titer above 0.6 Bethesda Units (BUs) was defined as positive. Only inhibitors with positive titers on two occasions were considered.
For each patient with an inhibitor, the cumulative number of EDs to FVIII/FIX concentrates before inhibitor development, the dates of detection and titers of the first two positive inhibitors, and the date of resolution of inhibitors were collected from medical records and patient diaries. The cumulative number of EDs was evaluated up to 200 EDs. When inhibitors were observed after 200 EDs, treatment years with clotting factor concentrates before inhibitor development were evaluated instead of EDs.
Each observed inhibitor was classified as a PUP or PTP inhibitor based on the cumulative number of EDs to FVIII/FIX concentrate before inhibitor development. We used the ISTH definitions to define PUP inhibitors as those that developed in a patient within 150 EDs and PTP inhibitors as those that developed after 150 EDs. Additionally, observed inhibitors were classified as high-responding and low-responding inhibitors depending on the inhibitor titer (5 BU) and degree of immune response to FVIII or FIX. Transient inhibitors were defined as inhibitors that disappeared within several months of continuous exposure to FVIII or FIX.
Clinical characteristics, such as type and severity of hemophilia, age at detection of inhibitor, mutation type, family history of inhibitor, and treatment type (prophylaxis vs. on-demand) during the previous 1 year before inhibitor development, were obtained from medical records of patients with inhibitors; these data were compared between PUPs and PTPs. To identify non-patient-related factors for inhibitor development, possible events within 3 months before the first inhibitor detection, such as change of the factor concentrate used, short-term high exposure to factor concentrate to prevent and control bleeding, and continuous infusion of factor concentrate, were obtained from medical records of patients with inhibitors. Additionally, we also obtained as much information as possible on the history of surgery, infection, diagnosis of cancer and/or treatment, use of immunosuppressive and/or immunomodulator agents, and vaccination within 3 months prior to the first inhibitor detection using the medical records of patients with inhibitors. These data were then compared between PUPs and PTPs.
Appropriate IRB approval was obtained for this study (IRB no. 2018-06-011).
DISCUSSION
The prevalence of inhibitors observed in patients with HA in this study was comparable to that in a meta-analysis of prevalence data for inhibitors developed in patients with HA [
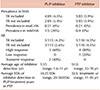
345]. In our study, the prevalence of inhibitors, including transient inhibitors, was 8.7% (10/115) in 115 patients with HA and 10.1% in 89 patients with SHA; this was 7.0% and 7.9% in all patients with HA and SHA, respectively, when transient inhibitors were excluded. Nearly all inhibitors developed in SHA, and only one inhibitor, a high-responding inhibitor in a patient with mild HA, was observed among the 26 patients with non-SHA. The prevalence in non-severe patients with HA was 3.8% (1/26) (
Table 1).
It is known that most factor of VIII/IX inhibitors arise after relatively few EDs to factor VIII, early in the patient's life in severe and moderate hemophilia; after 150–200 EDs, the subsequent risk of inhibitor development is very low [
34567]. Based on this observation, the ISTH has differentiated inhibitors as PUP inhibitors and PTP inhibitors [
6].
PTP inhibitors rarely develop in patients with HA (0.1–0.6% per patient-year) [
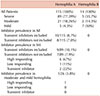
7]. Thus, it had been believed that most inhibitors are observed in PUPs. On the contrary, in our study, the cumulative number of inhibitors was the same for PUPs and PTPs (5 inhibitors each), and the prevalence of PUPs and PTPs was not different: 4.3% in PUPs and 4.5% in PTPs. Furthermore, when excluding two transient inhibitors observed only in PUPs, the prevalence was 2.6% and 4.5% in PUPs and PTPs, respectively (
Table 2). Thus, more inhibitors of significance were observed in PTPs. A recent study on the incidence of inhibitors in patients with SHA in the UK, which analyzed prospective reports in the UK National Hemophilia Database of all new inhibitors reported between 1990 and 2009, showed that new inhibitors may present throughout the life of patients with SHA, with a bimodal risk pattern that is greatest in early childhood (<5 yr) and old age (>60 yr) [
15]. Nearly all inhibitors during this later peak are believed to be PTP inhibitors; inhibitors developed in patients with previously acquired tolerance to FVIII during their first EDs. An increasing frequency of PTP inhibitors among elderly patients with SHA, which is not reflected in earlier reports, may be emerging because patients are living longer [
1314]. Although the ages during the later peak were lesser than those of the UK study, a similar trend was observed in patients with HA in this study, with an average age of inhibitor development of 5.15 (1.6–11) years and 51.0 (33–70) years in PUPs and PTPs, respectively, and no inhibitors developed in patients aged 11–33 years.
The mechanism for the development of inhibitors in PTPs is unknown, except in the case of new FVIII antigen exposure owing to a change in antigenic factor concentrates. The risk of new FVIII antigen exposure in PTPs was first witnessed in Austria and the Netherlands after exposure to new plasma-derived pasteurized FVIII concentrate (FVIII CPS-P) during 1990–1991 [
16]. This was also observed after the introduction of recombinant factors in the early 2000s, although the incidence was very low in PTPs (0–1.2% of the cohorts under investigation) [
1112]. In addition to the known risk of new antigen exposure, presumably, a breakdown of previous tolerance may be another mechanism for the development of inhibitors in PTPs because these patients have had many hundreds of FVIII EDs. This breakdown of tolerance may reflect circumstances (danger signals such as surgery and intensive replacement therapy) and/or deterioration in immune regulation with advancing age. Anecdotal evidence suggests that these inhibitors frequently arise after intense replacement therapy during surgery or to control bleeding (“peak treatment moments”), a risk factor that has been established in children with SHA and patients with mild HA [
1718]. Thus, nongenetic factors that would break down tolerance may contribute to the development of PTP inhibitors more than genetic factors. However, only a few studies on this issue have been conducted among PTPs; furthermore, nongenetic factors that would lead to the breakdown of tolerance were not included in most of these studies. Consequently, no risk factors, except the previously known risk of new antigen exposure, have been elucidated [
1112].
In this study, anecdotal events that might be related to the development of inhibitors in PTPs were observed in all 5 PTPs with inhibitors. On the contrary, no such events were observed in any of the 5 PUPs with inhibitors. The observed events were a change in factor concentrate, colon cancer surgery and chemotherapy, trauma due to a car accident and subsequent short-term high exposure to factor concentrate, and orthopedic surgery (
Table 3). Except for one case of new antigen exposure, all the other events may have contributed to the breakdown of tolerance to FVIII. Although our study population included a small number of cases at a single center, these results suggest that nongenetic factors may contribute to the development of inhibitors to a greater degree in PTPs than in PUPs because patient-oriented factors, such as hemophilia severity and mutation types, were not different between these groups (
Table 3).
Despite these findings, reflecting the anecdotal risk factors of inhibitor development in patients with mild and moderate HA [
18], some patient-oriented factors, such as family history of inhibitor and certain high-risk mutations, may presumably contribute to the development of PTP inhibitor. For example, 3 PTP inhibitors, all high-responding inhibitors, were observed in three brothers with SHA in this study. They had been treated on-demand for years, and inhibitors developed over age 55 years after events such as surgery, chemotherapy, and trauma with subsequent short-term high exposure to factor concentrate. The observed mutation among these family members was the Arg1997Trp missense mutation, which has been reported in moderate and SHA [
19]. This finding suggests that there may be certain high-risk F8 gene mutations and/or immunologic genetic factors in patients who are prone to developing PTP inhibitors. This may lead a patient with HA to break down tolerance easier than other patients, when nongenetic risk factors are superimposed on genetic risks, with subsequent PTP inhibitor development. Arg1997Trp may be such a high-risk mutation for the development of PTP inhibitor in patients with HA. However, this mutation has not been reported as a high-risk mutation, and neither type of inhibitor has been previously reported in patients with this mutation [
19]. Therefore, this should be confirmed in studies including more patients who have this missense mutation.
The present study was conducted in a relatively small number of patients at a single center in Korea. Thus, it is necessary to conduct national study in Korea to confirm the bimodal risk of inhibitor development during a patient's life, especially for the later peak of inhibitors, most of which developed in PTPs. Although our study findings suggest a greater role of nongenetic factors in inhibitor development among PTPs, a national study would serve to confirm these findings.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download