Abstract
This study describes five bilateral anatomical variations in the feet of a 97-year-old male cadaver. Following routine dissection, all variants were measured and documented. Three accessory tendons and two accessory ossicles were identified. Bilateral accessory tendons were present from the tibialis anterior (type II), peroneus tertius (type III), and peroneus brevis muscles. Accessory tendon length was 36–104 mm and width was 1–3 mm each inserting more distally then the main tendon. Accessory ossicles were identified as an accessory navicular and os peroneum, respectively. Individually, each variation has varying prevalence rates in the literature, but to date, no known studies have been published describing the combined presence of all five bilateral variations. The acknowledgement of multi-variant cases such as this one may be helpful in the clinical setting, particularly for patients with pathology or for those undergoing foot and ankle surgery.
Accessory tendons occur in the anterior compartment of the leg in approximately 9%–22% of the population [12] and are present in the lateral compartment in 11% of the population [3]. These accessory tendons also demonstrate a variety of tendon attachments and typically insert separate from the main tendon of the muscle [13]. Other tendinous anomalies include the presence of accessory ossicles: small, additional bones that result from unfused ossification centers and do not serve any function yet are present in the foot with a prevalence as high as 26% [4].
Unless associated with a pathology or noticed in a radiograph, accessory structures often go unnoticed. In surgery, a working knowledge of anatomical variation is key in protecting accessory structures. This knowledge is also important in diagnosis, as an awareness of potential variations is useful in the interpretation of a patient's physical exam, radiographs, computed tomography scans, or magnetic resonance imagings. In educational dissection, students focus on high-yield material with emphasis on the typical presentation of the musculature. An accessory tendon may be disregarded, accidentally removed, or not extensively examined. These tendons often go unreported, resulting in a lack of literature regarding the concordance rates of multiple accessory tendons in the foot. Thus, the purpose of this case study was to detail the unique case of multiple morphological tendon variants and accessory ossicles represented bilaterally in a single human embalmed specimen.
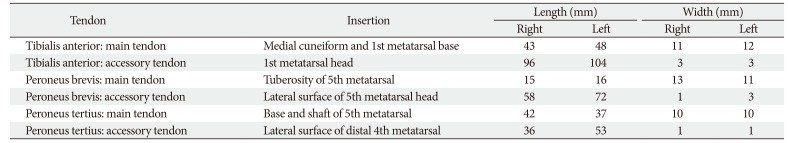
Bilateral routine foot dissection took place on a 97-year-old embalmed male cadaver. Each limb was isolated distally from mid-shaft of the tibia and fibula. Standard dissection of the distal leg, dorsum and plantar surface of the foot was completed bilaterally. Bilaterally, three muscles demonstrated accessory tendons. The tendon of the peroneus tertius (PT) had a prominent main tendon with a broad insertion along the length of the fifth metatarsal and a thin accessory tendon inserting on the base of the fourth proximal phalanx (Fig. 1C, D). The peroneus brevis muscle (PB) had a main tendon that inserted on the tuberosity of the fifth metatarsal and a thin accessory tendon that inserted laterally on the fifth metatarsal head (Fig. 1A). The main tendon of the tibialis anterior (TA) inserted on the base of the first metatarsal and medial cuneiform, while its thin accessory tendon attached at the head of the first metatarsal (Fig. 1B). For each muscle, the accessory tendon was less than 50% of the width of the main tendon and inserted more distally on the foot. Tendon dimensions were measured and recorded (Table 1).
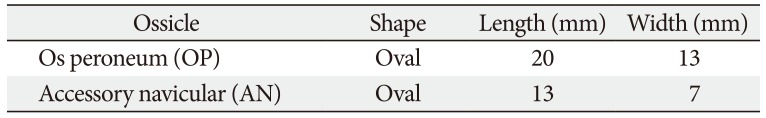
Bilateral ossicles were noted within the tendon of peroneus longus (PL) near the long plantar ligament and within the tendon of the tibialis posterior muscle (TP) distal to the tarsal tunnel. The ossicles were then isolated. The ossicle within the PL was fully embedded in the tendon located just distal to the peroneal sulcus of the cuboid bone (Fig. 2A). The ossicle was slightly concave, coordinating with the convexity of the cuboid (Fig. 2A, B). Located within the tendons of TP, the ossicle was 5 and 6 mm from the navicular tuberosity on the right and left feet, respectively. The ossicle was fully embedded within the tendon, proximal to its division, and was oval (Fig. 2C, D). Ossicle dimensions are found in Table 2.
Variations in tendon morphology are common, but the concordance and bilateral presentation of the structures make this an interesting case. The PT is absent in approximately 4% to 15% of the population [5]. Two broad categories of PT tendon are reported: a single tendon (type I) and a double tendon with a slip (type II) [1]. The PTs observed in this case study fit the type II classification, with a main tendon inserting on the fifth metatarsal base and shaft, and an accessory tendon inserting on the lateral head of the fourth metatarsal. The prevalence of type II tendons is near 9% [1]. In about half of all cases, PT inserts exclusively at the base of the fifth metatarsal but may have a varied insertion on the lateral aspect of the foot [15].
In about 11% of the cases, PB demonstrates a double tendon with a slip, with the main tendon inserting on the base of the fifth metatarsal and the thin accessory tendon inserting laterally on the distal fifth metatarsal [3]. Both tendons of PB in this study match this description. Interestingly, the peroneus digiti quinti (PDQ) is an accessory peroneal muscle of the lateral compartment of the leg and is described as a tendon without a muscle belly off the tendon of PB to an insertion near the fourth and fifth metatarsal heads [67]. The tendons of PB observed in this case study fits both descriptions. However, PDQ's lack of a muscle belly suggests that it is simply an accessory tendon of PB.
One of the most common muscles with an accessory tendon is the TA muscle, with an incidence of approximately 22% [2]. Nearly 7% of the accessory insertions of the TA have an attachment on the distal shaft of the first metatarsal [2]. Musial (1963) [8] classified the tendon of TA into four types. The tendons of this study fit the description of type III tendons. Type III has an estimated prevalence of 4% and present with a principal insertion on the medial cuneiform and first metatarsal and possess supernumerary tendons [8].
The accessory ossicles observed in the tendon of PL can be classified as os peroneum (OP), which has a prevalence between 15% and 88% [49]. OP is located within the tendon of PL in the cuboid tunnel at the cuboidocalcaneal joint. With age, the incidence of OP increases, with a 10% increase in each decade of life. The highest incidence reported is around 42% between ages 60–69 [9]. Thus, OP development may be related to cumulative biomechanical stresses through the lifespan. The OP may cause inflammation in the tendon of PL and painful OP syndrome [4]. Due to its location, the OP can easily be misinterpreted as a Jones fracture or styloid fracture of the fifth metatarsal by those less familiar with this ossicle [9].
The bones that were present in the tendon of TP match the description of the accessory navicular (AN). The AN has varying prevalence rates in the literature, ranging from 2% to 21% [4] and has three types based on its location and morphology [4]. In this study, the accessory ossicle presented within the distal TP tendon, classifying it as a type I AN, which accounts for 30% of all ANs [4]. Located adjacent to the spring ligament and talar head, a type I AN tend to be hypertrophic, indicating that the development of the accessory bone has a biomechanical stress component [10].
Other reports have demonstrated the concurrence of tendon anomalies. Sonmez et al. (2000) [11] reported on the bilateral concurrence of two accessory peroneal muscles—peroneus quartus and PDQ—as well as the presence of an accessory tendon from TA. Additionally, Raheja et al. (2005) [12] described a PB variation similar to PDQ, with concurrent variant morphology of the PT and PL tendons. Considering the concurrent variations of the same three tendons in this study and the anomalies noted by Sonmez, it is plausible that accessory structures of the foot are associated.
Developmentally, the accessory tendons may be explained by the differentiation of muscles from their primordia, which begins by week 9 of development. During this time there is evidence of spontaneous cell death during tissue morphogenesis [13]. Specifically, degeneration in fetal myotubes has been documented during the 10th–16th week of development [1415]. Alterations in this degeneration may allow for clusters of muscle cells to develop into imperfect, altered, or accessory muscles [14]. Persistence of some of these cells may account for some of the anomalous tendon formation observed in this study.
Accessory structures of the foot have clinical significance. While the tendons of this study likely had minimal impact on foot and ankle biomechanics, structures such as these can be associated with pain and swelling of the ankle, increase risk of tendon injury due to crowding within tendon sheaths [14], and may present possible challenges or complications during surgery. Accessory ossicles of the foot are associated with pathological conditions such fractures, osteonecrosis, osteomyelitis, and osteoarthritis. Furthermore, due to their locations within the tendons of TP and PL, the AN and OP can be classified as sesamoid bones that could potentially cause sesamoiditis [4]. Thus, cases such as this are important educational tools for anatomists, physicians, and therapists, as they provide examples of many anatomical variations that may be present in our patient populations.
Presently, there is no known literature regarding the concurrent observation of these accessory structures. Thus, these five bilateral accessory structures are a noteworthy finding. While the individual contribution to biomechanics is not known for each anomaly, it is possible that the combined presence of these five accessory structures carried clinical significance and may have resulted in a unique biomechanical footprint.
References
1. Ercikti N, Apaydin N, Kocabiyik N, Yazar F. Insertional characteristics of the peroneus tertius tendon: revisiting the anatomy of an underestimated m uscle. J Foot Ankle Surg. 2016; 55:709–713. PMID: 26860045.
2. Luchansky E, Paz Z. Variations in the insertion of tibialis anterior muscle. Anat Anz. 1986; 162:129–136. PMID: 3789411.
3. Imre N, Kocabiyik N, Sanal HT, Uysal M, Ozan H, Yazar F. The peroneus brevis tendon at its insertion site on fifth metatarsal bone. Foot Ankle Surg. 2016; 22:41–45. PMID: 26869499.
4. Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF 3rd, Roemer FW, Malguria N, Guermazi A. Sesamoids and accessory ossicles of the foot: anatomical variability and related pathology. Insights Imaging. 2013; 4:581–593. PMID: 24006205.
5. Joshi SD, Joshi SS, Athavale SA. Morphology of peroneus tertius muscle. Clin Anat. 2006; 19:611–614. PMID: 16317742.
6. Demir BT, Gümüşalan Y, Üzel M, Çevik HB. The variations of peroneus digiti quinti muscle and its contribution to the extension of the fifth toe. A cadaveric study. Saudi Med J. 2015; 36:1285–1289. PMID: 26593160.
7. Yammine K. The accessory peroneal (fibular) muscles: peroneus quartus and peroneus digiti quinti. A systematic review and meta-analysis. Surg Radiol Anat. 2015; 37:617–627. PMID: 25638531.
8. Musial WW. Variations of the terminal insertions of the anterior and posterior tibial muscles in man. Folia Morphol. 1963; 26:237–247.
9. Benninger B, Kloenne J. The clinical importance of the os peroneum: a dissection of 156 limbs comparing the incidence rates in cadavers versus chronological roentgenograms. Foot Ankle Online J. 2011; 2:2.
10. Bareither DJ, Muehleman CM, Feldman NJ. Os tibiale externum or sesamoid in the tendon of tibialis posterior. J Foot Ankle Surg. 1995; 34:429–434. PMID: 8590876.
11. Sonmez M, Kosar I, Cimen M. The supernumerary peroneal muscles: case report and review of the literature. Foot Ankle Surg. 2000; 6:125–129.
12. Raheja S, Choudhry R, Singh P, Tuli A, Kumar H. Morphological description of combined variation of distal attachments of fibulares in a foot. Surg Radiol Anat. 2005; 27:158–160. PMID: 15580345.
13. Fidziańska A, Goebel HH. Human ontogenesis. 3. Cell death in fetal muscle. Acta Neuropathol. 1991; 81:572–577. PMID: 1858485.
14. Webb JN. The development of human skeletal muscle with particular reference to muscle cell death. J Pathol. 1972; 106:221–228. PMID: 5046933.
15. Webb JN. Cell death in developing skeletal muscle: histochemistry and ultrastructure. J Pathol. 1977; 123:175–180. PMID: 592022.
Fig. 1
(A) Accessory tendon morphology. The accessory tendon of peroneus brevis muscle (PB) (arrowheads) extended from the main tendon of PB to attach laterally on the head of the fifth metatarsal. Also visible are the tendons of peroneus longus (PL), peroneus tertius (PT), and extensor digitorum longus (EDL). (B) The main tendon of the tibialis anterior (TA) inserts on the medial cuneiform and first metatarsal base, while the accessory tendon of TA (arrowheads) inserts at the head of the first metatarsal (**). Also visible is the tendon of extensor hallucis longus (EHL), the tendon of tibialis posterior muscle (TP), and the tendon of flexor digitorum longus (FDL). (C, D) Anomalous bifurcation in the tendon of PT indicated by black arrowheads. Image C demonstrates the lateral view of the tendon, while Image D demonstrates the dorsolateral view of the tendon as it attached to the lateral base of the fourth proximal phalanx. Also visible are the muscle belly of extensor digitorum brevis (EDB), tendon of PB, and tendons of EDL.
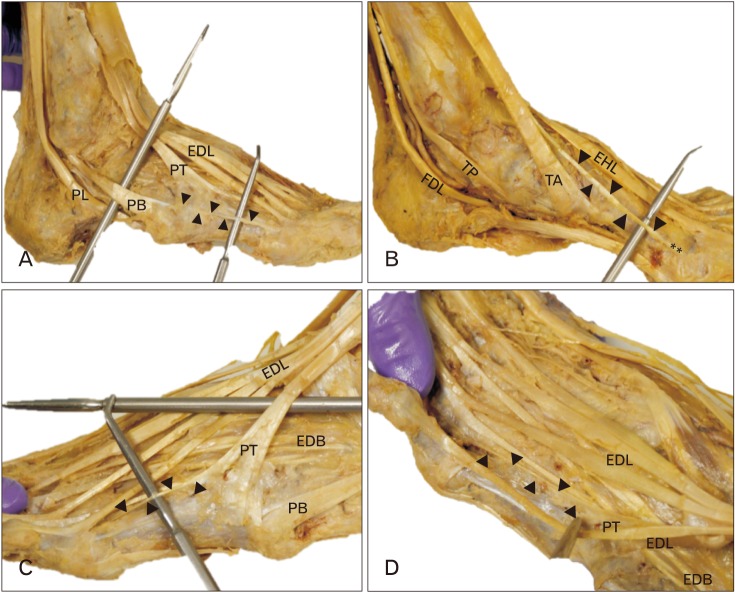
Fig. 2
(A) Ossicle morphology. The os peroneum (OP, *) within the tendon of peroneus longus (PL), adjacent to the cuboid. Arrow indicates the convex facet on the cuboid bone at the site of articulation with the sesamoid bone. Also visible is the tendon of peroneus brevis muscle (PB). (B) Isolated OP, measuring 20 mm long and 13 mm wide. (C) Accessory navicular (AN; indicated by tip of probe) located within the tendon of tibialis posterior muscle (TP), proximal to its division and adjacent to the navicular tuberosity (NT). Also visible are the long plantar ligament (LPL), short plantar ligament (SPL), and spring ligament (SL). (D) Isolated AN, measuring 13 mm long and 7 mm wide.
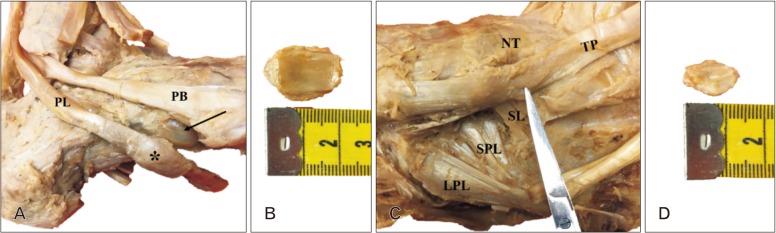
Table 1
Tendon insertions, lengths, and widths for the main and accessory tendons of the left and right tibialis anterior, peroneus brevis, and peroneus tertius muscles




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download