Abstract
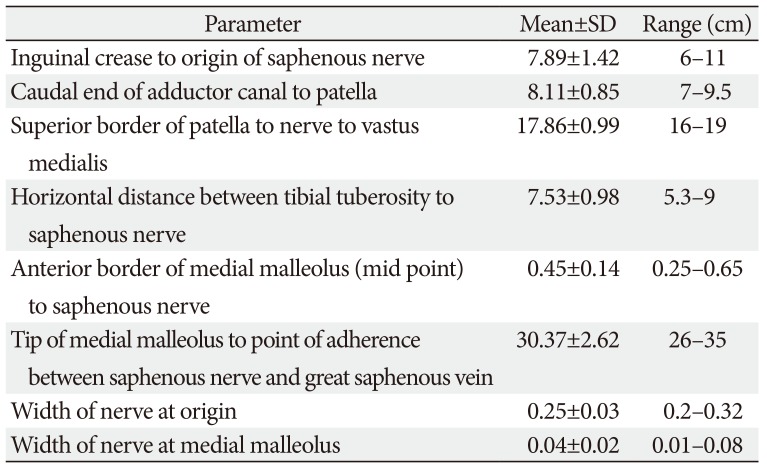
The knowledge about detailed morphology and relation of saphenous nerve is important to obtain successful saphenous nerve regional blocks to achieve pre- and post-operative anesthesia and analgesia, nerve entrapment treatments and to avoid damage of saphenous nerve during knee and ankle surgeries. The literature describing detailed morphology of saphenous nerve is very limited. We dissected 42 formalin fixed well embalmed cadaveric lower limbs to explore detailed anatomy, relation and mode of termination of saphenous nerve and measured the distances from the nearby palpable bony landmarks. The average distance of origin of saphenous nerve from inguinal crease was 7.89±1.42 cm, the distance from upper end of medial border of patella to saphenous nerve at that level was 8.11±0.85 cm, distance from tibial tuberosity was 7.53±0.98 cm and from midpoint of anterior border of medial malleolus was 0.45±0.14 cm. Saphenous nerve provided two infrapatellar branches at the level of mid to lower limit of patellar ligament in 90% cases. It was in close contact or adhered to great saphenous vein across the lower 2/3rd of leg lying either anterior, posterior or deep to the vein. The saphenous nerve terminated by bifurcating proximal to medial malleolus in majority of cases though no obvious bifurcation was observed in 9.52% cases. The detailed morphology, relations and the distances from palpable bony landmarks may be helpful for clinicians to achieve successful saphenous nerve block and to avoid saphenous nerve damage and related complications during orthopedic procedures.
Saphenous nerve (SN) is the longest sensory branch of femoral nerve and provides sensory supply to the medial aspect knee, medial border of leg and medial border foot in humans. The SN arises from femoral nerve within femoral triangle of thigh, travels through the adductor canal and lies subcutaneously along medial border of leg and foot as far as the great toe [12345].
The SN is often utilized for regional nerve block procedures [6] to alleviate perioperative or postoperative pain related to total knee arthroplasty [4] to achieve anesthesia in ankle and foot surgical procedures combined with sciatic nerve block [7] and to provide pain relief in SN entrapment syndromes [8].
The SN injury and related symptoms is quite common during harvesting great saphenous venous grafts for vascular bypass procedures [2910]. Injury to SN or its infrapatellar branches and post-operative paresthesia-numbness has been reported in various knee surgeries-meniscal surgeries of knee by peripatellar incision [1], anterior cruciate ligament reconstruction [11], and arthroscopic knee examination and surgeries [12]. The SN damage may happen during arthroscopic procedures related to ankle at the level of medial malleolus [3] and fasciotomy procedure [13].
All these surgical and anesthetic nerve block procedures need detailed understanding of SN morphology and its relation to nearby palpable and observable anatomical landmarks. The literature providing accurate anatomical distance of SN from nearby anatomical landmarks is limited. This study explored the anatomy of SN in relation to nearby bony and palpable landmarks to provide an anatomical guide to locate the nerve accurately during SN block procedures and to avoid SN injuries during saphenous venous graft and other surgical interventions. We also observed the relation of SN with the great saphenous vein (GSV) along its course and the mode of termination of SN.
We conducted a dissection based observational study to explore the course and relations of SN. Forty-two cadaveric lower limbs from 21 formalin fixed well embalmed cadavers were dissected at gross anatomy lab of our institution over a period of one and half year (July 2017 to December 2018).We followed the traditional dissection method of lower extremity to expose the course of SN over the entire lower limb.
First horizontal incision was made on the skin along the inguinal crease, second horizontal incision was made at the level of tibial tuberosity, third horizontal incision was made joining the medial and lateral malleoli around the ankle and the fourth horizontal incision was made on dorsum of foot along the base of toes. The midpoints of adjacent horizontal incisions were connected by vertical incisions. The skin was dissected and reflected as superficially as possible along the incision lines. The superficial fascia was dissected and retracted very carefully particularly from the level of patella downwards to expose the whole SN from thigh to foot. Sartorius muscle was retracted to expose the contents of adductor canal in thigh including SN, femoral vessels and nerve to vastus medialis within thigh.
The following distances were measured (Fig. 1): (1) the distance from inguinal crease to the origin of SN from femoral nerve, (2) superior border of patella to nerve to vastus medialis (where it pierced the muscle), (3) caudal opening of adductor canal to upper border of patella, (4) tibial tuberosity to SN, (5) anterior border of medial malleolus to SN, (6) tip of medial malleolus to the point of close contact between SN and GSV, (7, 8) width of SN at origin and at the level of medial malleolus.
All the measurements were done by digital caliper and measuring tape where appropriate.
The relation of the SN and GSV was noted along its course. The infrapatellar branch of SN and its relation to patella was noted. The mode of termination of SN was noted.
We observed that SN arose from medial aspect of femoral nerve within femoral triangle. The point of origin ranged from 6–11 cm distal to inguinal crease (Table 1), it was located in close proximity to other branches of femoral nerve including medial cutaneous nerve of thigh and nerve to vastus medialis. The SN was lying in the same plane of femoral nerve, deep to fascia lata. The nerve travelled into the adductor canal along with femoral vessels and nerve to vastus medialis. (Fig. 2). Within the extent of adductor canal, it crossed the femoral artery from lateral to medial side. The nerve to vastus medialis innervated the vastus medialis muscle by 1–3 ramifications, the lowest one was approximately 16–19 cm proximal from the superior border of patella. In all the cadavers, the nerve to vastus medialis ended by innervating the vastus medialis within middle third of thigh. The SN exited from the adductor canal on the postreo-medial aspect of knee close to medial femoral condyle, the distance from upper border of patella to the SN at this level varied from 6.5–9 cm. Beyond this point, the SN passed between sartorius and gracilis muscles and became subcutaneous, it gave 1–2 infrapatellar branches (Fig. 3) towards patellar ligament at the level of midpoint to lower end of patellar ligament, approximately 5.3–9 cm postero-medial to medial border of patellar ligament.
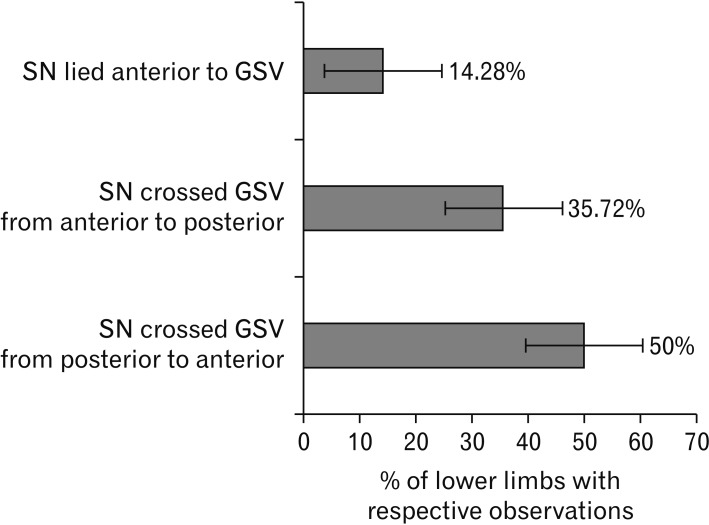
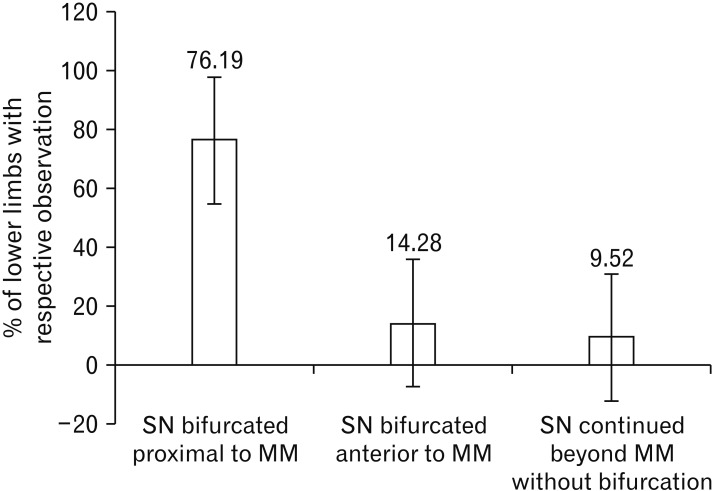
The distance of SN from tibial tuberosity ranged from 5.3 to 9 cm postero-medially. The SN travelled almost vertically along the tibia in a subcutaneous plane along with the GSV (Fig. 4). At upper end of leg or tibia, the SN was separated from the vein by a strip of adipose tissue measuring 0.5–2.5 cm which diminished downward and the nerve and vein came in close contact or most of the time adhered with each-other approximately at the junction of upper and middle third of leg (range, 25–31 cm from tip of medial malleolus). In 50% cases (n=21) SN was posterior to GSV in upper third of leg, it remained deep to the GSV for a variable distance and it lay anterior to the vein in lower third of the leg or close to medial malleolus. In 35.72% cases (n=15), the SN was anterior to the vein in upper third of leg, crossed the vein at variable distance superficial or deep to vein and lay posterior to GSV in lower third of leg, in 14.28% cases (n=6), the SN was noted anterior to GSV throughout its course from upper leg to foot (Fig. 5). SN divided into two terminal branches proximal to medial malleolus in 76.19% cadavers (n=32) (Fig. 6) in 14.28% cadavers (n=6), the bifurcation happened anterior to anterior border of medial malleolus (Fig. 7) in 9.52% cases (n=4), no prominent bifurcation was visible and the main trunk of SN continued anterior to medial malleolus (Fig. 8).
The average distance from midpoint of anterior border of medial malleolus to anterior terminal branch of SN ranged from 0.25 to 0.65 cm, the distance was lesser at upper end of medial malleolus (<0.2 cm) and increased toward tip of medial malleolus up to 0.08 cm. The course of SN could not be traced clearly beyond tip of medial malleolus in most of our dissected specimens except one where the anterior terminal branch ended at ball of the great toe.
The current study provides a set of data of cadaveric measurements of SN in relation to palpable anatomical landmarks along its course, the relation of SN to GSV in leg and the mode of termination of SN.
SN block can be performed by various approaches [6]. The current study recommended the needle should be placed approximately 6–11 cm distal to inguinal crease, and approximately 0.5–4.5 cm deep to skin depending on adipose tissue content at the same plane of femoral nerve within femoral triangle for perifemoral approach. However, close proximity to other branches of femoral nerve may prevent isolated SN block at this place which was also mentioned by Benzon et al. [6].
The distal most branch of nerve to vastus medialis ended by innervating the muscle approximately 16–19 cm above the superior border of patella. So, application of anesthetic drug by sub sartorial approach below this level will prevent simultaneous blockage of nerve to vastus medialis and will reduce the delay in post-operative ambulation and recovery [4]. In a study by Kapoor et al. [14], the distance between upper border of patella from most distal visible branch of nerve to vastus medialis was reported as 16.8–16.6 (±3.6) cm which corresponds with our finding. At the caudal end of adductor canal, the SN lay approximately 8.11±0.85 cm postero- medial to the upper end of patellar medial border, medial to femoral artery, postero-medial to sartorius muscle. This location of SN deep to sartorius muscle and close to femoral artery within adductor canal has been reported advantageous to access and locate the nerve in relation to femoral artery or descending branch of femoral artery by ultrasound guidance in previous studies [415161718]. In a study by Manickam et al. [19], SN was identified at 12.2±2.2 cm proximal to knee joint by ultrasound guidance and consistently blocked in all cases indicating the simplicity and reliability of SN block at adductor canal.
In a study by Romanoff et al. [8], series of SN block at adductor canal resulted considerable pain relief in patients with SN entrapment at adductor canal. At below knee level, the SN lay 5.3–9 cm postero-medially from the tibial tuberosity, subcutaneous infiltration of anesthetic around this area could be utilized to block SN, as a below knee approach [67], and this location has been used in blind subcutaneous approach by some researchers [20]. Blocking SN by a paravenous approach mentioned by De Mey et al. [20] would be more successful at junction of upper and middle third of leg, within 26–35 cm above the tip of medial malleolus as the SN lay in close contact with GSV posterior or anterior to the vein.
The terminal continuation of SN was observed 0.25–0.65 cm anterior to the mid-point of anterior border of medial malleolus. The distance was less at upper end of medial malleolus and gradually increased towards its tip. Anesthetic should be injected 3–4.5 cm proximal to tip of medial malleolus and immediately anterior to anterior border to block SN, GSV could be a good guide to block this nerve at this level. The nerve often lies immediately deep to GSV, so needle can be put parallel to GSV in anterior and posterior direction. Benzon et al. [6] mentioned the effectiveness of block at medial malleolar level, injection placed above and anterior to medial malleolus was able to provide complete sensory blockade in 60% volunteers.
The thickness of SN was noted as 0.25±0.03 cm in average at its origin, the thickness reduced to approximately 0.04±0.02 cm at the level of medial malleolus. Approximate width of SN might help in calculating the safe distances accordingly from the nearby anatomical landmarks, it would possibly reduce the incidences of nerve punctures and related complications during regional blocks or other procedures [71321].
In thigh, within femoral triangle and adductor canal, the SN lay in a deeper plane in comparison to GSV and remained separated from the vein by considerable amount of fat, fascia and sartorius muscle. Beyond the adductor canal, the SN passed between sartorius and gracilis muscles and became subcutaneous. At the medial aspect of knee and along approximately upper third of leg, SN and GSV remained separated by connective tissue sleeves of varying thickness ranging 0.5–2.5 cm depending on the thickness of adipose layer. Along the middle third and lower third of leg, the SN and GSV lay in close contact, sometimes inseparably adhered to each-other, the nerve lying either anterior, posterior or hidden deep to the GSV (Fig. 9). The point from where SN and GSV had an intimately related course ranged between 26 and 35 cm from the tip of medial malleolus. This study recommends to avoid lower 2/3rd of leg while harvesting saphenous venous graft to avoid damage to SN and subsequent neuropathy [910]. Although Dayan et al. [2] suggested the lower third of tibia as most vulnerable region for harvesting GSV.
We observed the SN provides usually two (90% cases) infrapatellar branches towards inferior aspect of patella approximately at the level of midpoint to lower end of patellar ligament, arising from SN 4–7 cm medial to midpoint of patellar ligament. Some variation of infrapatellar branches has been reported in previous studies [22]. This anatomic relation should be kept in mind to avoid damage to these branches during knee surgeries to avoid postoperative neuropathy [11112].
The SN divided into two terminal branches at 3–4.5 cm proximal to the upper limit of medial malleolus in 76.1% cadavers, the individual branches were very thin (<0.01 cm) beyond medial malleolus and ended by innervating the integument, in only one of our cadaveric specimen, the anterior terminal branch could be traced up to ball of the great toe. Though previous studies reported SN [23] terminated by bifurcating 3–5.5 cm proximal to medial malleolus in 100% cases, we observed bifurcation at the level of midpoint of medial malleolus in 14.28% and no bifurcation was observed in 9.52% cases.
In average, the terminal part of SN lay 0.45±0.14 cm anterior to midpoint of anterior border of medial malleolus, the incision for ankle surgeries and arthroscopic ports should be made accordingly to avoid SN damage at this level. In a study by Mercer et al. [3], it was suggested to make arthroscopic portals posterior to medial malleolus and close to tendon of tibialis anterior to avoid damage to SN.
The one limitation of this study was embalming induced alteration of water and fat content in cadavers which might have altered some measurements in comparison to living though the course of nerve and palpable anatomical landmarks remain unaltered. We did minimal cleaning and handling of fascial structures around SN to keep anatomic relations intact as much as possible while dissecting and recording measurements. Another limitation was inability to apply these set of data in clinical setting to prove its effectiveness.
Findings of this study corroborated with previous studies which indicate our specimen represented the general population.
Current study measured the distances and relations of SN from palpable and observable anatomical landmarks along its course which would be helpful for clinicians including anesthetists and orthopedic surgeons.
Acknowledgements
We sincerely thank the kind people who donated their bodies for medical education and research, without whom our work would not be possible.
References
1. Hunter LY, Louis DS, Ricciardi JR, O'Connor GA. The saphenous nerve: its course and importance in medial arthrotomy. Am J Sports Med. 1979; 7:227–230. PMID: 474860.
2. Dayan V, Cura L, Cubas S, Carriquiry G. Surgical anatomy of the saphenous nerve. Ann Thorac Surg. 2008; 85:896–900. PMID: 18291167.
3. Mercer D, Morrell NT, Fitzpatrick J, Silva S, Child Z, Miller R, DeCoster TA. The course of the distal saphenous nerve: a cadaveric investigation and clinical implications. Iowa Orthop J. 2011; 31:231–235. PMID: 22096447.
4. Jenstrup MT, Jaeger P, Lund J, Fomsgaard JS, Bache S, Mathiesen O, Larsen TK, Dahl JB. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand. 2012; 56:357–364. PMID: 22221014.
5. Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 3rd ed. Philadelphia, PA: Wolters Kluwer;2018.
6. Benzon HT, Sharma S, Calimaran A. Comparison of the different approaches to saphenous nerve block. Anesthesiology. 2005; 102:633–638. PMID: 15731603.
7. Donohue CM, Goss LR, Metz S, Weingarten MS, Dyal LB Jr. Combined popliteal and saphenous nerve blocks at the knee: an underused alternative to general or spinal anesthesia for foot and ankle surgery. J Am Podiatr Med Assoc. 2004; 94:368–374. PMID: 15265996.
8. Romanoff ME, Cory PC Jr, Kalenak A, Keyser GC, Marshall WK. Saphenous nerve entrapment at the adductor canal. Am J Sports Med. 1989; 17:478–481. PMID: 2782531.
9. Chauhan BM, Kim DJ, Wainapel SF. Saphenous neuropathy: following coronary artery bypass surgery. N Y State J Med. 1981; 81:222–223. PMID: 6258112.
10. Nair UR, Griffiths G, Lawson RA. Postoperative neuralgia in the leg after saphenous vein coronary artery bypass graft: a prospective study. Thorax. 1988; 43:41–43. PMID: 3281308.
11. Portland GH, Martin D, Keene G, Menz T. Injury to the infrapatellar branch of the saphenous nerve in anterior cruciate ligament reconstruction: comparison of horizontal versus vertical harvest site incisions. Arthroscopy. 2005; 21:281–285. PMID: 15756180.
12. Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res. 1995; (320):88–94. PMID: 7586847.
13. Pyne D, Jawad AS, Padhiar N. Saphenous nerve injury after fasciotomy for compartment syndrome. Br J Sports Med. 2003; 37:541–542. PMID: 14665597.
14. Kapoor R, Adhikary SD, Siefring C, McQuillan PM. The saphenous nerve and its relationship to the nerve to the vastus medialis in and around the adductor canal: an anatomical study. Acta Anaesthesiol Scand. 2012; 56:365–367. PMID: 22335278.
15. Saranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, Nakou M, Anagnostopoulou S, Kostopanagiotou G. Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 2011; 36:399–402. PMID: 21697687.
16. Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate during saphenous nerve block at the adductor canal: a cadaver study. Acta Anaesthesiol Scand. 2015; 59:238–245. PMID: 25496028.
17. van der Wal M, Lang SA, Yip RW. Transsartorial approach for saphenous nerve block. Can J Anaesth. 1993; 40:542–546. PMID: 8403121.
18. Krombach J, Gray AT. Sonography for saphenous nerve block near the adductor canal. Reg Anesth Pain Med. 2007; 32:369–370. PMID: 17720129.
19. Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009; 34:578–580. PMID: 19916251.
20. De Mey JC, Deruyck LJ, Cammu G, De Baerdemaeker LE, Mortier EP. A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med. 2001; 26:504–506. PMID: 11707786.
21. Bonner SM, Pridie AK. Sciatic nerve palsy following uneventful sciatic nerve block. Anaesthesia. 1997; 52:1205–1207. PMID: 9485977.
22. Pannell WC, Wisco JJ. A novel saphenous nerve plexus with important clinical correlations. Clin Anat. 2011; 24:994–996. PMID: 21800370.
Fig. 1
Schematic diagram showing measurement points. AB, distance from inguinal crease to origin of SN from femoral nerve; AH, adductor hiatus; BC, diameter of SN at origin; DE, distance from upper margin of patella to lowest branch of NVM; FA, femoral artery; FN, femoral nerve; FV, femoral vein; GH, distance from tip of medial malleolus to point of adherence between SN and GSV; GSV, great saphenous vein; LK, distance between patella to caudal limit of adductor canal; MM, medial malleolus; NVM, nerve to vastus medialis; OP, distance between anterior border of MM to SN; PT, patella; QR, diameter of SN at level of MM; SN, saphenous nerve; SR, sertorius; TT, tibial tuberosity; VL, vastus lateralis; VM, vastus medialis; MN, horizontal distance between TT and SN.
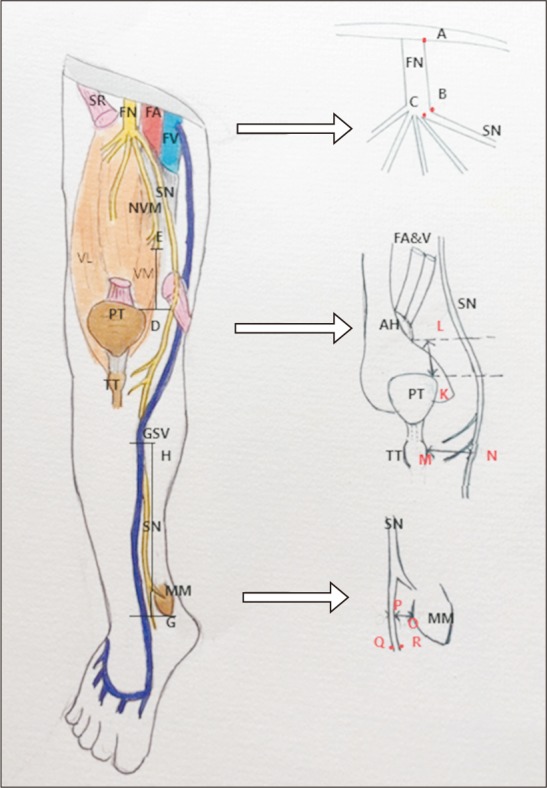
Fig. 2
Close proximity of saphenous nerve (SN) and nerve to vastus medialis (VM) muscle (at tip of the probe) in middle third of thigh. GSV, great saphenous vein; NVM, nerve to vastus medialis; RF, rectus femoris.

Fig. 3
Infrapatellar branches of saphenous nerve (SN) at lower limit of patellar ligament (PL). TT, tibial tuberosity; IPB 1&2, infrapatellar branch 1&2.
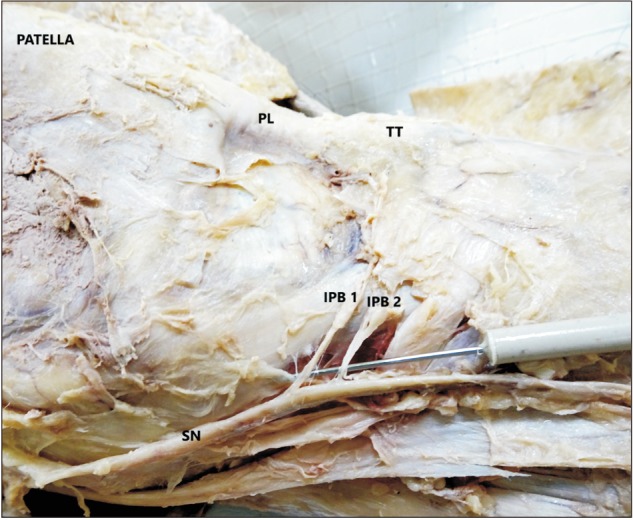
Fig. 4
Figure showing the course of saphenous nerve and great saphenous vein through lower limb. SN, saphenous nerve; GSV, great saphenous vein.
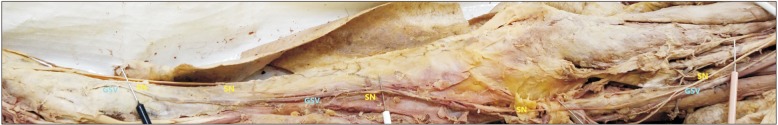
Fig. 6
Terminal divisions of saphenous nerve (SN) proximal to medial malleolus. SN AD, anterior division of saphenous nerve; SN PD, posterior division of saphenous nerve; GSV, great saphenous vein; MM, medial malleolus; TP, tibialis posterior tendon.
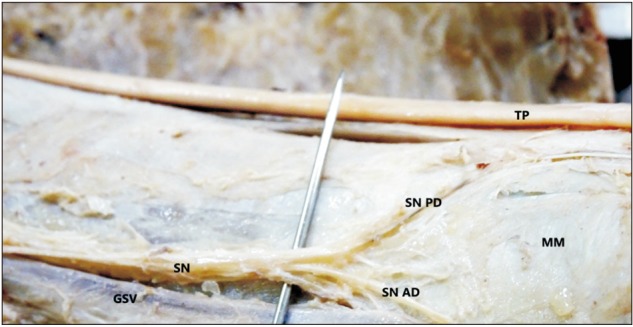
Fig. 7
Terminal divisions of saphenous nerve along anterior border of medial malleolus. SN AD, anterior division of saphenous nerve; SN PD, posterior division of saphenous nerve; GSV, great saphenous vein; MM, medial malleolus; TP, tibialis posterior tendon; TA,- tibialis anterior tendon.
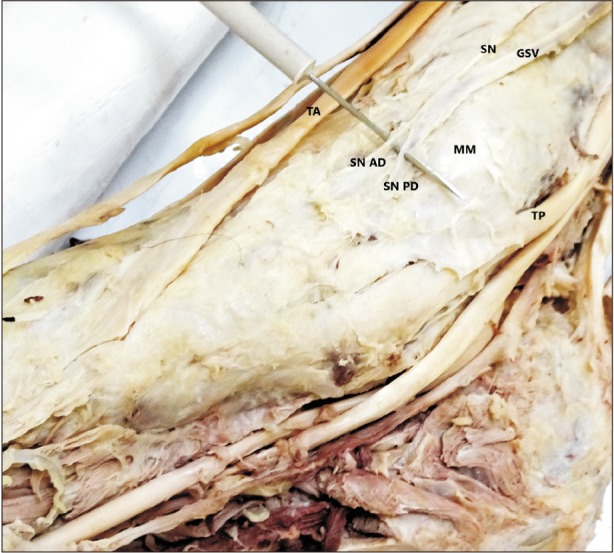
Fig. 9
Saphenous nerve crossing the great saphenous vein from anterior to posterior deep to vein in lower leg. SN, saphenous nerve; GSV, great saphenous vein.

Table 1
Distances and measurements related to saphenous nerve




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download