Abstract
The human quest to master the anatomy and physiology of living systems started as early as 1600 BC, with documents from the Greeks, Indians, and Romans presenting the earliest systematic studies and advances. Following the fall of the Roman Empire, the progress slowed until the Renaissance renewed scientific interest in anatomy and physiology, ushering in an era of spectacular advances. Alongside the discoveries of modern science, innovations in media such as printing, photography and color reproduction, improved the accuracy of communicating science. Techniques for noninvasively viewing the human body, such as magnetic resonance imaging, opened up new ways of exploring and understanding anatomy, physiology, and disease pathogenesis. Advances in three-dimensional (3D)-technologies, including computer graphics and animation are directly linked to many advances in medicine and surgery. Anatomy education has come a long way from papyrus leaf inscriptions to computerized 3D modeling, holographic representation, and virtual reality-based software. The future presents unlimited options for studying and understanding anatomy as Google glasses, bioprinting, virtual reality, and allied technologies transform the world into a classroom. This review summarizes the journey of mankind to master anatomy and physiology.
The term “anatomy” originates from the Greek “anatomē,” or dissection, and concerns the study of structural organization of organisms and their parts. The production of accurate anatomical images has challenged and allured scientific minds seeking to understand human anatomy, physiology, and disease [1]. Human curiosity has no bounds and the journey of anatomy is an example. This review is a historical journey of the evolution of anatomy from antiquity to present and toward the future. The history of medical education and anatomy involves the evolution of societies and their approach to illness and treating disease from ancient times to the present.
Reports suggest the study of anatomy began as early as 1600 BC in Greece with the examination of sacrificial human bodies. A rare papyrus, popularly called the Edwin Smith Surgical Papyrus (named after the archeologist who bought it), identifies the heart and its vessels, the liver, spleen, kidneys, hypothalamus, uterus, and bladder, and describes blood vessels emanating from the heart [2]. An Egyptian treatise, the Ebers Papyrus (ca. 1550 BC), features prescriptions, drugs, and compounding. It also identifies the heart as the center of the blood supply and vessels that carry fluids (Fig. 1) [3]. Systematic anatomical study started with the work of Greek scientists, including Alcmaeon (ca. 500 BC), Empedocles (ca. 490–430 BC) and Hippocrates (ca. 460–377 BC). Alcmaeon performed human dissections in his research in an attempt to discover the source of human intelligence. Hippocrates was the first to classify or categorize the fluids in the human body. In the next centuries, Aristotle (ca. 384–322 BC), Praxagoras, and several contemporaries produced a more descriptive anatomical system based on animal dissection. The Greek physicians introduced concepts of medical diagnosis, prognosis, and medical ethics [14].
Indian medicine, or Ayurvedic medicine, is considered the oldest system of traditional medicine. Indian medical scholars began practicing medicine ca. 1200 BC. The manuscript Atharvaveda from ca. 700 to 600 BC refers to the use of herbs to treat ailments. The Charakasamhitā, composed by Charaka, and the Suśrutasamhitā, by Sushruta, describe disease treatment and early surgery. Suśrutasamhitā features scientific classifications of medicine, with 184 chapters and 8 branches, of which “kāyācikitsā” (internal medicine) and “śalyacikitsā” (surgery including anatomy) are notable. Sushruta also wrote about different types of surgery and surgical equipment. Anatomy and embryology were part of surgical education, with knowledge passed down by ink on palm leaf manuscripts or by memory - “shruti” (the remembered) [567].
Chinese medicine also developed traditional medicine to treat diseases. Huangdi Neijing is a classical Chinese medicine text written ca. 500–300 BC which forms the basis of traditional Chinese medicine [1]. This book clearly explains that physiological processes of the body follow natural rules and that the disease state can be influenced by natural ageing processes and the environment.
Herophilus (335–280 BC) performed the first systematic vivisections and is widely acknowledged as the “father of anatomy.” Herophilus and Erasistratus (304–250 BC) described the brain as the center of the nervous system, with significant mentions of brain ventricles. Herophilus provided careful accounts of several organs and emphasized the curative powers of drugs, dietetics, and gymnastics [89]. Galen's (ca. 130–200 BC) major contribution was his work on the circulatory system. He was the first to recognize the differences between venous (dark) and arterial (bright) blood. His anatomical experiments on animal models led to an improved understanding of the circulatory system, nervous system, and respiratory system. Galen also wrote treatises on human anatomy, which were presented simply as observations on papyrus or paper without detailed diagrammatic representation [1011]. The ancient Romans created a range of surgical tools, including bone levers, surgical shears, and speculums, which are dated back as early as the first century AD. These tools would have also been used to visualize internal structures for studying anatomy and to perform some surgical techniques [12]. During the next few centuries, the Greek anatomical treatises were lost. Though some were translated later to other languages like Latin, old English, and Arabic. Some works were retained in Byzantium and the Islamic world and contained only rudiments of the original findings [2].
During the Roman rule of the Byzantine Empire, Byzantine physicians composed the first medical textbooks developed from and adding to the knowledge of their Greek and Roman predecessors. They used text and diagrams to elucidate anatomy. Paul of Aegina (625–690) wrote The Medical Compendium in Seven Books and is considered the “father of our medical books.” Meanwhile, the Sassanid Empire in Persia established the first medical centers [13]. Islamic medicine came into prominence as they compiled their own medical knowledge, developed by physicians like Muhammad Ibn Z. Al razi and Ibn Sina based on Arabic translations of Galen's work [14].
The fall of Rome, disease, and socioeconomic turmoil led to widespread apathy towards the study of medicine and anatomy. During the early middle ages, medicine passed into the hands of the Christian church and Arab scholars. During this time religious philosophy overshadowed scientific knowledge and study. The main contributions of this period were extensive translations of Greek texts into Latin, Arabic, and a variety of other languages [15].
With the rebirth of classicism in the Renaissance, medical science, anatomy and medical teaching regained prominence in Europe. Mondino de Luzzi (ca. 1270–1326) founded the first European medical school in Italy in 1235 by incorporating the systematic study of anatomy and dissection into a medical curriculum [16]. The main mediums for portraying anatomical representations were hand drawings on paper and woodcut engraving. The 15th century saw a greater involvement of artists in developing the scientific knowledge and depiction of the human body, including the anatomical paintings by Leonardo da Vinci (1452–1519) (Fig. 2). Medical interest was so high in the Renaissance that many famous artists like Michelangelo (1475–1564) and Rembrandt (1606–1669) also produced anatomical drawings (Fig. 3). Realism a dominant Renaissance artistic style that depended more on perspective to create an illusion of space and depth was also inspired by the growing interest of artists in anatomy. Andreas Vesalius (1514–1564) integrated systematic text with artistic drawings in his influential De humani corporis fabrica (On the Structure of the Human Body), for which he is considered the “father of modern human anatomy” [17] (Fig. 4). Vesalius also practiced hands on teaching methods based on dissecting corpses.
The field of anatomy reached new heights with the contributions of scientists like Realdo Colombo (1515–1559), William Harvey (1578–1657), and Galileo Galilei (1564–1642) [18]. New artistic methods of copperplate engraving, copper plate etching and lithography improved the speed and accuracy of anatomical reproductions. Anatomy was recognized as a unique discipline for its integration of science, art, and technology [19].
The advent of the printing press in the 15th to 17th century helped to better convey anatomy by translating observation to drawing. This was particularly important because the rapid growth of medical schools in the 16th century led to a pressing demand for cadavers. In the absence of available cadavers, anatomical drawings had to serve as substitute teaching tools.
Scientists discovered new techniques in studying and portraying anatomy. Marcello Malpighi (1628–1694) founded microscopic anatomy, the use of magnification to study structures that are invisible to the naked eye [20]. His discoveries formed the basis of the modern disciplines of cytology, cellular anatomy, and histology. Gaetano Zumbo (1656–1701) developed anatomical wax modeling techniques by the end of the 17th century, creating the first method of 3D anatomical modeling [21]. Tissues and organs were dehydrated and put in wax blocks for long term preservation. This would later form the basis of histology, the microscopic analysis of thin slices or sections of these blocks. Improved methods for the storage and preservation of dissected specimens, including drying and wax injection, allowed for more detailed study, which would extend not only to histology but new fields of pathology and developmental biology [22].
During the late 17th to the early 19th century, scientists like [23], and Xavier Bichat developed the fields of morbid anatomy and pathology. Morgagni published observations of over 640 dissections, covering diseases over the entire human body, in his seminal work, De Sedibus et Causis Morborum per Anatomen Indagatis (The Seats and Causes of Diseases Investigated by Anatomy) [1]. Baillie published the first English book on pathology, Morbid Anatomy of Some of the Most Important Parts of the Human Body, in which he records systematic observations of organs in various disease states. Bichat studied the structure of diseased organs and in his Treatise on Membranes, distinguished over twenty types of tissues that form organs [2]. These studies served to demonstrate the importance of “pathological anatomy” in understand disease and treatment [23].
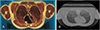
Technological innovations in the past two decades have allowed for significant advances in anatomical research. Discoveries of photography, relief halftone, and color photography revolutionized the illustration and education of anatomy. Scientists were starting on a quest to image the human body in a less invasive way. The discovery of X-ray machines by Wilhelm Rontgen in 1895 finally allowed physicians to visualize the inside of a human body without dissection [24]. In 1930 Felix Bloch discovered the magnetic resonance imaging (MRI) machine, in which magnetic fields and radio waves cause atoms to give off tiny radio signals to generate images of the organs in the body. Godfrey Hounsfield and Allan Cormack's discovery of computed tomography (CT) in 1972 enabled researchers to study organs in unprecedented detail [25] (Fig. 5). An effort to introduce three-dimensional (3D) anatomical representation in anatomy teaching using clay/plastic models were introduced. These 3D models lacked accuracy and were difficult to manipulate, as they were hand or casted with clay, plaster of paris or plastic molded. However, technology would soon build off of this concept to revolutionize anatomy.
Medical and anatomical education is transitioning from black board drawings, text book diagrams, and cadaveric dissection to cutting edge technology in digital 3D anatomy and virtual reality. The complexity and dimension of the human body, coupled with the incredible volume of information in medicine, makes the learning process challenging. Physicians and medical students have reported a disconnect between the cadavers they studied in anatomy classes and the CT scans, radiographs, ultrasound and MRI scans they use in the hospital as patient data [2627]. These new technologies seek to bridge the gap between education and practice. One of the drawbacks with traditional cadaveric dissection is that a student can only reference the cadaver in the anatomy lab. The advantage of using a virtual system is that student can view 3D structures repeatedly, remotely and throughout their training. Many virtual models are available on PCs and smartphones. Complete Anatomy by 3D4Medical and 3D Atlas by Anatomy Learning are free smartphone apps that provide virtual anatomical models.
As our understanding of anatomy and our ability to study structure in detail has evolved, so have the goals of medical research. Current initiatives in anatomy focus on development, evolution, physiology, pathology, and regenerative medicine. One of the technological challenges that the field was facing is the generation of accurate 3D images at the tissue/ cellular level for all the organ systems in a human body.
Cadaveric body donations to anatomy departments have drastically reduced due to religious traditions, disease transmission issues, and government acts in many countries (e.g., the Human Tissue Act 2004 in Britain) [28]. This led to the Visible Human Project (VHP) in America, which set out to create a detailed set of transverse CT, MRI, and cryosectional photographs of the entire human body (Fig. 6). A male and a female cadaver were cryosectioned from head to toe at intervals of one to one-third of a millimeter. CT, MRI, and cryosection images of representative sections were recorded. The VHP project started under the directives of the U.S. National Library of Medicine in 1986. The data set of the human male subject was completed in 1994 and dataset for the female in 1995 [2930]. This incredible collection is a milestone in medical imaging and anatomy education and can be viewed at the National Museum of Health and Medicine near Washington, DC.
To obtain higher resolution images, VHP was repeated as the Korean VHP (2002), and Chinese VHP (2002–03) [313233]. By volumetric reconstruction, these cross-sectional images are transformed into 3D images of anatomic structures and compiled into an invaluable library for medical education and research. The Korean VHP contains data from two serially sectioned cadavers, while the Chinese VHP includes nine. To acquire higher resolution images, cadavers were sectioned by thinner intervals (0.2 mm or less) and advanced image analysis software was used to generate comprehensive structures. VHP and many other databases of 3D anatomy are available for free or upon request. The American VHP, Korean VHP, and Chinese VHP together form the entry terms for the medical subject heading “Visible Human Projects”, by the National Library of Medicine.
VHP was just the beginning. Computerized high-resolution photographs of each VHP cryosection, together with MRI/CT scans, can be over layered and reconstructed into a 3D model to help correlate CT/MRI images to visible anatomy. DICOM Library is another free online site that shares medical CT and MRI images or video file for educational and scientific purposes [34].
The 3D model can be virtually dissected into different planes and angles by using computer graphics. Each layer of the biological system can be added or removed from the 3D model. This is particularly useful in teaching; starting with the skeleton one can overlay the muscle layer, followed by the network of blood vessels and nerves. Medical students can practice electronic dissections [33]. The advent of the 3D renderings led to the concept of virtual surgery and virtual medical procedures like endoscopy, lumbar puncture, and cardiopulmonary resuscitation via the development of virtual dissection software [35]. Cross-sectional images and models are offered for medical education and clinical practice such as electronic anatomy atlas that will transparently link visual knowledge forms to symbolic knowledge formats such as the names of body parts. Resources such as Electronic Anatomy Atlas, an interactive 3D human anatomy model, have also been made available for medical education.
Virtual reality platforms like Anatomage, Biodigital, Netter3DAnatomy, and Visible Body, Primalpictures are amongst the few that have revolutionized anatomical studies [3637]. Anatomage features a highly accurate virtual anatomy visualization and dissection system called the “Anatomage Table.” One of the advantages of virtual reality over cadaveric anatomy is the ability to transition from macroscopic to microscopic and back instantly [37]. Moreover, these virtual platforms are touch-interactive and multi-user friendly to facilitate the team-based learning process that many medical curriculums emphasize [3839].
Many diseases are associated with complex changes in anatomy that require meticulous pre-procedure treatment planning. Scientists from the Stanford University Medical Center have developed a unique visualization software from EchoPixel that renders two-dimensional CT scans into 3D images, giving the doctors a virtual image of the patient's unique arterial anatomy for endovascular repair of splenic artery aneurysms [40]. Scientists at the Duke Cancer Institute successfully developed a software program named automated Bone Scan Index to automatically measure bone metastases and tested in patients with advanced prostate cancer. This new software will ensure effective treatment and reduce the time required to manually assess bone metastases [41].
High-quality 3D models are more promising than cadaverbased studies as they lack the challenges associated with dissection, including structure recognition, cost, repairing fragile structures, ethics, and hygiene. Fig. 7 shows and example where patient specific successive CT scans are deconvoluted to make a 3D model. The virtual human integrates human anatomy, biophysics, physiology and biomechanics into an interactive computer model that can be reused, shared, and [42].
Recent study clearly suggests the importance of human anatomical dissection despite the arrival of new innovations in learning human anatomy [8]. The greatest and most obvious criticism of virtual reality has questioned its ability to replicate the tactile experience of dissection. Can virtual dissection demonstrate, for example, how delicate or resistant a tissue is when touched by an instrument? The development of haptic enabled virtual platforms seeks to bridge this gap between the virtual and corporeal and are currently used in surgical training. ImmersiveTouch, founded in 2005 by a group of engineers and surgeons, developed a virtual reality platform with advanced haptic feedback which was proven to improve training outcomes. The University of Illinois at Chicago found that practice with this platform increased the percentage of successful ventriculostomies performed by neurosurgery residents [43].
One of the newest goals in anatomy is 3D printing of human anatomy models. Charles Hull originally developed 3D printing technology for rapid prototyping of plastic parts in 1986 [44]. 3D printing, or additive printing technology, repeatedly layers printing materials based on a computerized 3D object model, to manufacture an object. The ability of 3D printing technology to precisely reconstruct intricate anatomical structures has led to the increasing use of 3D printing applications, from anatomy education with 3D models to surgical practice and applications in advanced regenerative biology research [454647]. Fig. 8 is an example of a 3D printed hand model showing the skeletal structure (white) and the musculature (transparent) used to teach anatomy. Some of the important players in 3D printing include Stratasys, Formlabs, Carbon, Prusa, GE additive, Mark forged, Lulzbot, BCN3D, and Zortrax.
The current approach to reconstructive surgical problems is engineering-based, such as customized prosthetics. 3D printing is revolutionizing the production of biomaterial scaffolds for application in several fields of medicine [48]. The first step of this process is creating a 3D template; thus, progress in 3D printing has depended on the ability to render precise anatomical detail. Advanced 3D modeling softwares are now available through platforms like Blender, SketchUp, SolidWorks, AutoCAD, and Maya, It is now possible to build entire tissues by 3D printing of biocompatible materials, cells, and supporting components into complex 3D functional living tissues, a process called bioprinting [49]. Though in its infancy, 3D bioprinting raises high hopes for addressing the shortage of tissues for organ transplantation and regenerative medicine. Several hospitals already use 3D bioprinting to generate tissues including multilayered skin, bone, vascular grafts, tracheal splints, heart tissue and cartilaginous structures for transplant [50]. Fig. 9 shows an example of how 3D printing of bone mimic transplant can be used to correct jaw bone defects based on patient specific 3D models.
3D bioprinted mesotissues, microtissues, and organoids are used to develop human disease models for high-throughput screening, drug discovery, and toxicology. 3D bioprinting is an intricate process and several factors must be considered including the choice of materials, sensitivities of cell types, growth and differentiation factors, and technical challenges relating to mimicking the tissue niche [2750]. Fig. 10 describes how bone bio-engineering can be used for knee joint replacement or knee arthroplasty to treat severe arthritis pain or injury. The integration of knowledge from several fields, including engineering, biomaterials science, cell biology, physics, and medicine, is necessary to overcome these challenges. Important companies leading in 3D-bioprinting include Orgnovo, Cyfuse Biomedical, Bio Bots, Aspect Biosystems, 3D printing solutions, Rokit and Nano3D. 3D bioprinting, coupled with virtual reality, will pave the way to future regenerative therapies, as well as improved medical education and surgical procedures.
The potential applications of digital 3D models and 3D printing in medical education are currently limited by cost and safety, but it is expected that with time, cost will decrease and efficacy will increase, leaving us with extraordinary possibilities for the future of medicine.
In the age of the phone-as-computer, smartphone usage has exploded worldwide and has become an indispensable part of modern medicine. Interesting and fascinating apps are already in the market like “Essential Anatomy,” “Anatomy Learning -3D Atlas,” “Muscle and Bone Anatomy 3D,” “Teach Me Anatomy,” to study human anatomy in stunning 3D details. Peer reviewed digital 3D model libraries can provide print models to educators globally. Projection mapping, interactive projections complexed with computer graphic realism, will take center stage. Learning with interactive replicas and 3D or 4D-printed anatomical models will open hybrid learning options [5152]. The new field of medical animation seeks to capture attention and break down anatomical complexity. Anatomic classrooms will use 3D holographic three or four-sided projections of anatomical models to project not only visual, but also auditory and haptic outputs to truly simulate patient interaction [53]. 3D stereoscopic formats will be introduced. Robust and fully searchable terminology databases, game-based exercises, quizzing, real-time interactive and accessible platforms will link medical education globally. Google glasses may become a teaching tool to link multimedia information to anatomical models, such as positioning a live ultrasound image over a patient [5455]. Google glasses are currently being tested for their effectiveness in aiding surgery.
Physicians continue to seek minimally invasive techniques. Nano robots which self-assemble from nanoscopic parts will help in drug delivery, physiological data collection (including video), sensor, survey, and provide live update [55]. Artificial intelligence (AI) or machine intelligence is the process by which an electronic device sensor perceives its environment and maximizes the chances of achieving its goal. AI uses statistical approaches, computational intelligence, and symbolic AI to effectively achieve programmed goals [32]. AI is already used in refining diagnostic tools. MRI and other imaging modalities require the patient to stay still to avoid artifacts or noise, which may misleadingly influence the physician's decision and subsequent treatment. AI can help remove the noise and artifact to increase the effectiveness of patient care [27]. Personalized student education based on AI will create hybrid lessons with different styles of teaching for a user-friendly learning experience. Thus the future holds great promise in the field of anatomy and physiology. The applications are far reaching, including space science, sports science, and global health. We have come a long way from ink diagrams scrawled on papyrus, but there is still progress to be made and great promise for the role of technology in advancing medicine.
Figures and Tables
 | Fig. 1Edwin Smith Papyrus. Recto Columns 8 and 9. Picture from the archives of U.S. National Library of Medicine, https://ceb.nlm.nih.gov/projects/ttp/. |
 | Fig. 2Drawing (c. 1507) by Leonardo da Vinci showing the principal organs, vasculature, and the female urinogenital system. Source: http://www.visi.com/~reuteler/leonardo.html{{pd}}Category:LeonardodaVinci. |
 | Fig. 3An excerpt of Michelangelo's anatomical studies of the muscular system. Source: http://classicalpulse.blogspot.com/2013/06/michelangeloanatomy-studies.html. |
 | Fig. 4Vesalius drew accurate illustrations, with. Figures drawn in the artistic style of Renaissance realism. This figure of the musculoskeletal system stands in controposto. De Humani Corporis Fabrica. Basel, 1543. Woodcut. Picture from the archives of U.S. National Library of Medicine, https://www.nlm.nih.gov/dreamanatomy/da_g_I-B-1-07.html. |
 | Fig. 5A typical computed tomography scan through the coronal plane, showing the details of the cavity and parts of the abdomen. Right bottom: as seen through the Axial plane. A great improvement from century old paintings. Source: https://commons.wikimedia.org/w/index.php?title=Scrollable_highresolution_computed_tomography_images_of_a_normal_thorax&oldid=255941168. |
 | Fig. 6This is from the thorax subset of the VHP project. (A) Photograph showing a section through Visible Human Male: thorax, including heart, lungs, spinal column, major vessels, musculature. (B) Computed tomography scan image of the same plane of the thorax. Source: from the archives of National Library of Medicine, https://www.nlm.nih.gov/research/visible/visible_gallery.html. |
 | Fig. 7Patient specific successive computed tomography (CT) scans are deconvoluted to make a 3D model. (A) Successive CT scans are placed back to back to create depth in an artistic way. (B–H) CT scan deconvolution. The 3D model created is rotated and shown from different angels and showing different layers, complexity of organ system. Multi-material FDM 3D printing can elucidate the skin and underlying organs. CT scan database: Lung Image Database Consortium image collection (LIDC). |
 | Fig. 83D printed model showing the skeletal structure (white) and the musculature (transparent). The template was made using a computed tomography bone scan and 3D hand scan and printed by dual extruder printing. Model organs can also be printed for students and practitioners. |
 | Fig. 9Jaw bone defect corrected with a bone mimic transplant made 3D printed from a computed tomography scan (shown by arrows). |
 | Fig. 10Bone bio-engineering. Knee joint replacement or knee arthroplasty is commonly used to treat severe arthritis pain or injury. The prosthetic is 3D printed from a model based on the patient's computed tomography (CT) scan by metal laser sintering, CAD files: grab CAD. Alternatively, 3D printed bone scaffolds can be seeded with osteogenic cells derived from bone marrow stem cells or iPSCs and allowed to integrate normally. CT Database: Lung Image Database Consortium image collection. |
References
1. Persaud TV, Loukas M, Tubbs RS. A history of human anatomy. Springfield, IL: Charles C Thomas Publisher Ltd.;2014.
2. Aldersey-Williams H. Anatomies: a cultural history of the human body. New York: Norton & Company;2014.
3. Vargas A, López M, Lillo C, Vargas MJ. The Edwin Smith papyrus in the history of medicine. Rev Med Chil. 2012; 140:1357–1362.
4. Hallmann-MikoXMLLink_XYZajczak A. Ebers Papyrus. The book of medical knowledge of the 16th century B.C. Egyptians. Arch Hist Filoz Med. 2004; 67:5–14.
5. Loukas M, Lanteri A, Ferrauiola J, Tubbs RS, Maharaja G, Shoja MM, Yadav A, Rao VC. Anatomy in ancient India: a focus on the Susruta Samhita. J Anat. 2010; 217:646–650.

6. Deepa B, Pushpalatha K. Contributions of Sushruta to anatomy. Anat J Afr. 2014; 3:362–365.
7. Mahabir RC, Son-Hing J, Tam AL, Vastardis AD. Ancient Indian civilization: ahead by a nose. J Invest Surg. 2001; 14:3–5.
8. Reverón RR. Herophilus and Erasistratus, pioneers of human anatomical dissection. Vesalius. 2014; 20:55–58.
9. Bay NS, Bay BH. Greek anatomist herophilus: the father of anatomy. Anat Cell Biol. 2010; 43:280–283.

10. Fortuna S. The Latin editions of Galen's Opera omnia (1490-1625) and their prefaces. Early Sci Med. 2012; 17:391–412.

11. Trkalj G. Galen, macaques and the growth of the discipline of human anatomy. Am J Phys Anthropol. 2018; 165:277.
12. Lascaratos J, Voros D, Tsiamis C. Paul of Aegina: landmark in surgical progress. World J Surg. 2003; 27:1336.
13. Malomo AO, Idowu OE, Osuagwu FC. Lessons from history: human anatomy, from the origin to the Renaissance. Int J Morphol. 2006; 24:99–104.

15. Mavrodi A, Paraskevas G. Mondino de Luzzi: a luminous figure in the darkness of the Middle Ages. Croat Med J. 2014; 55:50–53.

16. Toledo-Pereyra LH. Leonardo da Vinci: the hidden father of modern anatomy. J Invest Surg. 2002; 15:247–249.

17. Zampieri F, ElMaghawry M, Zanatta A, Thiene G. Andreas vesalius: celebrating 500 years of dissecting nature. Glob Cardiol Sci Pract. 2015; 2015:66.

18. Van Hee R, Wells FC, Ballestriero R, Richardson R, Mazzarello P, Cani V, Catani M. The art of human anatomy: Renaissance to 21st century. Vesalius. 2014; 20:25–29.
19. Pearson AS. Art and anatomy in Renaissance Italy: images from a scientific revolution. Sixteenth Century J. 2013; 44:601–602.
20. DiDio LJ. Marcello Malpighi: the father of microscopic anatomy. Ital J Anat Embryol. 1995; 100 Suppl 1:3–9.
21. Puccetti ML, Perugi L, Scarani P. Gaetano Giulio Zumbo. The founder of anatomic wax modeling. Pathol Annu. 1995; 30 Pt 2:269–281.
22. Hajdu SI. A note from history: Rudolph Virchow, pathologist, armed revolutionist, politician, and anthropologist. Ann Clin Lab Sci. 2005; 35:203–205.
23. Ghosh SK. Giovanni Battista Morgagni (1682–1771): father of pathologic anatomy and pioneer of modern medicine. Anat Sci Int. 2017; 92:305–312.

24. Doi K. Diagnostic imaging over the last 50 years: research and development in medical imaging science and technology. Phys Med Biol. 2006; 51:R5–R27.

25. Dong Z, Andrews T, Xie C, Yokoo T. Advances in MRI Techniques and Applications. Biomed Res Int. 2015; 2015:139043.

26. Fasel JH, Aguiar D, Kiss-Bodolay D, Montet X, Kalangos A, Stimec BV, Ratib O. Adapting anatomy teaching to surgical trends: a combination of classical dissection, medical imaging, and 3D-printing technologies. Surg Radiol Anat. 2016; 38:361–367.

27. Grignon B, Oldrini G, Walter F. Teaching medical anatomy: what is the role of imaging today? Surg Radiol Anat. 2016; 38:253–260.

28. Juanes JA, Prats A, Lagandara ML, Riesco JM. Application of the "Visible Human Project" in the field of anatomy: a review. Eur J Anat. 2003; 7:147–159.
29. Spitzer VM, Whitlock DG. The Visible Human Dataset: the anatomical platform for human simulation. Anat Rec. 1998; 253:49–57.

30. Dai JX, Chung MS, Qu RM, Yuan L, Liu SW, Shin DS. The Visible Human Projects in Korea and China with improved images and diverse applications. Surg Radiol Anat. 2012; 34:527–534.

32. Murgitroyd E, Madurska M, Gonzalez J, Watson A. 3D digital anatomy modelling: practical or pretty? Surgeon. 2015; 13:177–180.
33. McMenamin PG, Quayle MR, McHenry CR, Adams JW. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ. 2014; 7:479–486.

34. Chen B, Leng S, Yu L, Holmes D 3rd, Fletcher J, McCollough C. An open library of CT patient projection data. Proc SPIE Int Soc Opt Eng. 2016; 9783:97831B.

35. Zilverschoon M, Vincken KL, Bleys RL. The virtual dissecting room: Creating highly detailed anatomy models for educational purposes. J Biomed Inform. 2017; 65:58–75.

36. Fredieu JR, Kerbo J, Herron M, Klatte RS, Cooke M. Anatomical models: a digital revolution. Med Sci Educ. 2015; 25:183–194.

37. Ward TM, Wertz CI, Mickelsen W. Anatomage table enhances radiologic technology education. Radiol Technol. 2018; 89:304–306.
38. Nicholson DT, Chalk C, Funnell WR, Daniel SJ. Can virtual reality improve anatomy education? A randomised controlled study of a computer-generated three-dimensional anatomical ear model. Med Educ. 2006; 40:1081–1087.

39. Olasky J, Sankaranarayanan G, Seymour NE, Magee JH, Enquobahrie A, Lin MC, Aggarwal R, Brunt LM, Schwaitzberg SD, Cao CG, De S, Jones DB. Identifying opportunities for virtual reality simulation in surgical education: a review of the Proceedings from the Innovation, Design, and Emerging Alliances in Surgery (IDEAS) Conference: VR Surgery. Surg Innov. 2015; 22:514–521.
40. Devcic Z, Kesselman A, Shah R, AbdelRazek M, Kothary N. Augmented virtual reality assisted treatment planning for splenic artery aneurysms: a pilot study. J Vasc Interv Radiol. 2018; 29:S17.
41. Armstrong AJ, Anand A, Edenbrandt L, Bondesson E, Bjartell A, Widmark A, Sternberg CN, Pili R, Tuvesson H, Nordle O, Carducci MA, Morris MJ. Phase 3 assessment of the automated bone scan index as a prognostic imaging biomarker of overall survival in men with metastatic castration-resistant prostate cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018; 4:944–951.
42. Li L, Yu F, Shi D, Shi J, Tian Z, Yang J, Wang X, Jiang Q. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017; 9:3867–3880.
43. Yudkowsky R, Luciano C, Banerjee P, Schwartz A, Alaraj A, Lemole GM Jr, Charbel F, Smith K, Rizzi S, Byrne R, Bendok B, Frim D. Practice on an augmented reality/haptic simulator and library of virtual brains improves residents' ability to perform a ventriculostomy. Simul Healthc. 2013; 8:25–31.

44. Heller TB, Hill RM, Saggal AF. 3D Systems, Inc. Google patent WO1991012120A1. 1991. 08. 22.
45. Ventola CL. Medical Applications for 3D printing: current and projected uses. P T. 2014; 39:704–711.
46. Garcia J, Yang Z, Mongrain R, Leask RL, Lachapelle K. 3D printing materials and their use in medical education: a review of current technology and trends for the future. BMJ Simul Technol Enhanc Learn. 2018; 4:27–40.

48. Seol YJ, Kang HW, Lee SJ, Atala A, Yoo JJ. Bioprinting technology and its applications. Eur J Cardiothorac Surg. 2014; 46:342–348.

49. Dababneh AB, Ozbolat IT. Bioprinting technology: a current state-of-the-art review. J Manuf Sci Eng. 2014; 136:061016.

50. Morris S. Future of 3D printing: How 3D bioprinting technology can revolutionize healthcare? Birth Defects Res. 2018; 110:1098–1101.

51. Brazina D, Fojtik R, Rombova Z. 3D visualization in teaching anatomy. Procedia Soc Behav Sci. 2014; 143:367–371.

52. Melo JS, Brasil LM, Balaniuk R, Ferneda E, Santana JS. Intelligent tutoring systems based on ontologies and 3D visualization platforms in the teaching of the human anatomy. In : Dössel O, Schlegel WC, editors. World Congress on Medical Physics and Biomedical Engineering, 2009 Sep 7-12, Munich, Germany. IFMBE Proceedings, Vol. 25. Berli: Springer;2009. p. 16–17.
53. Negi S, Dhiman S, Sharma RK. Basics and applications of rapid prototyping medical models. Rapid Prototyp J. 2014; 20:256–267.

54. Carter Y, Allard TT, Moore NC, Goertzen AL, Klonisch T, Hoppa RD. The role of 3D printing in teaching and education in human skeletal anatomy. FASEB J. 2009; 23:1 Suppl. 479.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download