1. Catalona WJ, Smith DS, Ratliff TL, Basler JW. Detection of organ-confined prostate cancer is increased through prostate-specific antigen-based screening. JAMA. 1993; 270(8):948–954.

2. Cooperberg MR, Broering JM, Kantoff PW, Carroll PR. Contemporary trends in low risk prostate cancer: risk assessment and treatment. J Urol. 2007; 178(3 Pt 2):S14–9.

3. Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007; 177(6):2106–2131.

4. Mohler JL, Armstrong AJ, Bahnson RR, D'Amico AV, Davis BJ, Eastham JA, et al. Prostate cancer, version 1.2016. J Natl Compr Canc Netw. 2016; 14(1):19–30.
5. Bahn D, de Castro Abreu AL, Gill IS, Hung AJ, Silverman P, Gross ME, et al. Focal cryotherapy for clinically unilateral, low-intermediate risk prostate cancer in 73 men with a median follow-up of 3.7 years. Eur Urol. 2012; 62(1):55–63.

6. Hurwitz LM, Cullen J, Elsamanoudi S, Kim DJ, Hudak J, Colston M, et al. A prospective cohort study of treatment decision-making for prostate cancer following participation in a multidisciplinary clinic. Urol Oncol. 2016; 34(5):233.e17–233.e25.

7. White S, Hricak H, Forstner R, Kurhanewicz J, Vigneron DB, Zaloudek CJ, et al. Prostate cancer: effect of postbiopsy hemorrhage on interpretation of MR images. Radiology. 1995; 195(2):385–390.

8. Ikonen S, Kivisaari L, Vehmas T, Tervahartiala P, Salo JO, Taari K, et al. Optimal timing of post-biopsy MR imaging of the prostate. Acta Radiol. 2001; 42(1):70–73.

9. Kaji Y, Kurhanewicz J, Hricak H, Sokolov DL, Huang LR, Nelson SJ, et al. Localizing prostate cancer in the presence of postbiopsy changes on MR images: role of proton MR spectroscopic imaging. Radiology. 1998; 206(3):785–790.

10. Rosenkrantz AB, Kopec M, Kong X, Melamed J, Dakwar G, Babb JS, et al. Prostate cancer vs. post-biopsy hemorrhage: diagnosis with T2- and diffusion-weighted imaging. J Magn Reson Imaging. 2010; 31(6):1387–1394.

11. Schaeffer EM, Partin AW, Lepor H. Open radical prostatectomy. In : Wein A, Kavoussi L, Partin A, Peters C, editors. Campbell-Walsh Urology. 11th ed. Philadelphia, PA: Elsevier Inc.;2015. p. 2641–2663.
12. Sokoloff MH, Brendler CB. Indications and contraindications for nerve-sparing radical prostatectomy. Urol Clin North Am. 2001; 28(3):535–543.

13. Chun FK, Steuber T, Erbersdobler A, Currlin E, Walz J, Schlomm T, et al. Development and internal validation of a nomogram predicting the probability of prostate cancer Gleason sum upgrading between biopsy and radical prostatectomy pathology. Eur Urol. 2006; 49(5):820–826.

14. Fukagai T, Namiki T, Namiki H, Carlile RG, Shimada M, Yoshida H. Discrepancies between Gleason scores of needle biopsy and radical prostatectomy specimens. Pathol Int. 2001; 51(5):364–370.

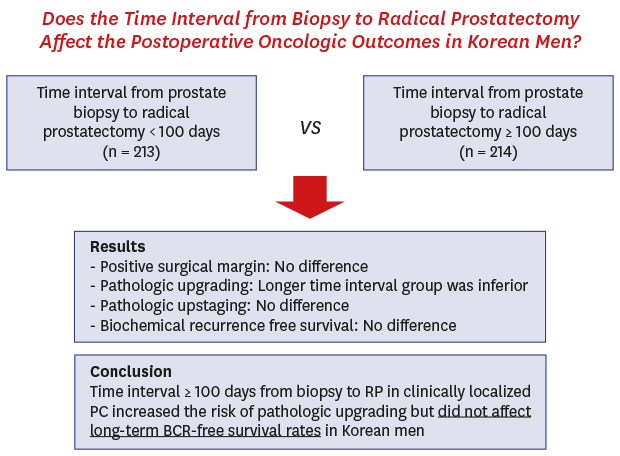
15. Khan MA, Mangold LA, Epstein JI, Boitnott JK, Walsh PC, Partin AW. Impact of surgical delay on long-term cancer control for clinically localized prostate cancer. J Urol. 2004; 172(5 Pt 1):1835–1839.

16. Abern MR, Aronson WJ, Terris MK, Kane CJ, Presti JC Jr, Amling CL, et al. Delayed RP for intermediate-risk Pca is associated with BCR-Possible implications for AS from the SEARCH database. Prostate. 2013; 73(4):409–417.
17. Phillips JJ, Hall MC, Lee WR, Clark PE. Does a delay in initiating definitive therapy affect biochemical recurrence rates in men with clinically localized prostate cancer? Urol Oncol. 2007; 25(3):196–200.

18. Weiner AB, Patel SG, Eggener SE. Pathologic outcomes for low-risk prostate cancer after delayed radical prostatectomy in the United States. Urol Oncol. 2015; 33(4):164.e11–164.e17.

19. Shibata A, Mohanasundaram UM, Terris MK. Interval from prostate biopsy to RP-effect on PSA,GS and risk of recurrence. Urology. 2005; 66(4):808–813.
20. van den Bergh RC, Steyerberg EW, Khatami A, Aus G, Pihl CG, Wolters T, et al. Is delayed radical prostatectomy in men with low-risk screen-detected prostate cancer associated with a higher risk of unfavorable outcomes? Cancer. 2010; 116(5):1281–1290.

21. Nam RK, Jewett MA, Krahn MD, Robinette MA, Tsihlias J, Toi A, et al. Delay in surgical therapy for clinically localized prostate cancer and biochemical recurrence after radical prostatectomy. Can J Urol. 2003; 10(3):1891–1898.
22. O'Brien D, Loeb S, Carvalhal GF, McGuire BB, Kan D, Hofer MD, et al. Delay of surgery in men with low risk prostate cancer. J Urol. 2011; 185(6):2143–2147.
23. Eroglu M, Doluoglu OG, Sarici H, Telli O, Ozgur BC, Bozkurt S. Does the time from biopsy to radical prostatectomy affect Gleason score upgrading in patients with clinical t1c prostate cancer? Korean J Urol. 2014; 55(6):395–399.

24. Robbins AS, Koppie TM, Gomez SL, Parikh-Patel A, Mills PK. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995–2004. Cancer. 2007; 110(6):1255–1263.

25. Man A, Pickles T, Chi KN; British Columbia Cancer Agency Prostate Cohort Outcomes Initiative. Asian race and impact on outcomes after radical radiotherapy for localized prostate cancer. J Urol. 2003; 170(3):901–904.

26. Zlotta AR, Egawa S, Pushkar D, Govorov A, Kimura T, Kido M, et al. Prevalence of prostate cancer on autopsy: cross-sectional study on unscreened Caucasian and Asian men. J Natl Cancer Inst. 2013; 105(14):1050–1058.

27. Heo JE, Ahn HK, Kim J, Chung BH, Lee KS. Changes in Clinical characteristics of patients with an initial diagnosis of prostate cancer in Korea: 10-year trends reported by a tertiary center. J Korean Med Sci. 2018; 33(6):e42.

28. Jeong IG, Dajani D, Verghese M, Hwang J, Cho YM, Hong JH, et al. Differences in the aggressiveness of prostate cancer among Korean, Caucasian, and African American men: a retrospective cohort study of radical prostatectomy. Urol Oncol. 2016; 34(1):3.e9–3.e14.

29. Kang DI, Chung JI, Ha HK, Min K, Yoon J, Kim W, et al. Korean prostate cancer patients have worse disease characteristics than their American counterparts. Asian Pac J Cancer Prev. 2013; 14(11):6913–6917.

30. Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT. Cancer control with radical prostatectomy alone in 1,000 consecutive patients. J Urol. 2002; 167(2 Pt 1):528–534.










 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download