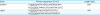
1. Ahmed W, Zheng K, Liu ZF. Small non-coding RNAs: new insights in modulation of host immune response by intracellular bacterial pathogens. Front Immunol. 2016; 7:431.

2. Li ZQ, Gui D, Sun ZH, Zhang JB, Zhang WZ, Zhang H, Guo F, Chen CF. Immunization of BALB/c mice with
Brucella abortus 2308ΔwbkA confers protection against wild-type infection. J Vet Sci. 2015; 16:467–473.

3. Wareth G, Melzer F, Böttcher D, El-Diasty M, El-Beskawy M, Rasheed N, Schmoock G, Roesler U, Sprague LD, Neubauer H. Molecular typing of isolates obtained from aborted foetuses in
Brucella-free Holstein dairy cattle herd after immunisation with
Brucella abortus RB51 vaccine in Egypt. Acta Trop. 2016; 164:267–271.

4. Sun YH, Rolán HG, den Hartigh AB, Sondervan D, Tsolis RM.
Brucella abortus virB12 is expressed during infection but is not an essential component of the type IV secretion system. Infect Immun. 2005; 73:6048–6054.

5. Raman N, Weir E, Müller S. The AAA ATPase MDN1 acts as a SUMO-targeted regulator in mammalian pre-ribosome remodeling. Mol Cell. 2016; 64:607–615.

6. Despras E, Sittewelle M, Pouvelle C, Delrieu N, Cordonnier AM, Kannouche PL. Rad18-dependent SUMOylation of human specialized DNA polymerase eta is required to prevent under-replicated DNA. Nat Commun. 2016; 7:13326.

7. Ryu HY, Wilson NR, Mehta S, Hwang SS, Hochstrasser M. Loss of the SUMO protease Ulp2 triggers a specific multichromosome aneuploidy. Genes Dev. 2016; 30:1881–1894.

8. Kunz K, Wagner K, Mendler L, Hölper S, Dehne N, Müller S. SUMO signaling by hypoxic inactivation of SUMO-specific isopeptidases. Cell Reports. 2016; 16:3075–3086.

9. Ma G, Li S, Han Y, Li S, Yue T, Wang B, Jiang J. Regulation of smoothened trafficking and hedgehog signaling by the SUMO pathway. Dev Cell. 2016; 39:438–451.

10. Brezden A, Mohamed MF, Nepal M, Harwood JS, Kuriakose J, Seleem MN, Chmielewski J. Dual targeting of intracellular pathogenic bacteria with a cleavable conjugate of kanamycin and an antibacterial cell-penetrating peptide. J Am Chem Soc. 2016; 138:10945–10949.

11. Vrioni G, Pappas G, Priavali E, Gartzonika C, Levidiotou S. An eternal microbe: Brucella DNA load persists for years after clinical cure. Clin Infect Dis. 2008; 46:e131–e136.
12. Zhang Y, Li T, Zhang J, Li Z, Zhang Y, Wang Z, Feng H, Wang Y, Chen C, Zhang H. The
Brucella melitensis M5-90 phosphoglucomutase (PGM) mutant is attenuated and confers protection against wild-type challenge in BALB/c mice. World J Microbiol Biotechnol. 2016; 32:58.

13. Ribet D, Hamon M, Gouin E, Nahori MA, Impens F, Neyret-Kahn H, Gevaert K, Vandekerckhove J, Dejean A, Cossart P.
Listeria monocytogenes impairs SUMOylation for efficient infection. Nature. 2010; 464:1192–1195.

14. Alagu J, Itahana Y, Sim F, Chao SH, Bi X, Itahana K. Tumor suppressor p14ARF enhances IFN-γ-activated immune response by inhibiting PIAS1 via SUMOylation. J Immunol. 2018; 201:451–464.

15. Zitti B, Molfetta R, Fionda C, Quatrini L, Stabile H, Lecce M, de Turris V, Ricciardi MR, Petrucci MT, Cippitelli M, Gismondi A, Santoni A, Paolini R. Innate immune activating ligand SUMOylation affects tumor cell recognition by NK cells. Sci Rep. 2017; 7:10445.

16. Athanassakis I, Iconomidou B. Cytokine production in the serum and spleen of mice from day 6 to 14 of gestation: cytokines/placenta/spleen/serum. Dev Immunol. 1996; 4:247–255.

17. Lim JJ, Kim DH, Lee JJ, Kim DG, Min W, Lee HJ, Rhee MH, Kim S. Protective effects of recombinant
Brucella abortus Omp28 against infection with a virulent strain of
Brucella abortus 544 in mice. J Vet Sci. 2012; 13:287–292.

18. Liu Z, Lee J, Krummey S, Lu W, Cai H, Lenardo MJ. The kinase LRRK2 is a regulator of the transcription factor NFAT that modulates the severity of inflammatory bowel disease. Nat Immunol. 2011; 12:1063–1070.

19. Dornand J, Gross A, Lafont V, Liautard J, Oliaro J, Liautard JP. The innate immune response against Brucella in humans. Vet Microbiol. 2002; 90:383–394.
20. von Bargen K, Gorvel JP, Salcedo SP. Internal affairs: investigating the
Brucella intracellular lifestyle. FEMS Microbiol Rev. 2012; 36:533–562.

21. Barquero-Calvo E, Chaves-Olarte E, Weiss DS, Guzmán-Verri C, Chacón-Díaz C, Rucavado A, Moriyón I, Moreno E.
Brucella abortus uses a stealthy strategy to avoid activation of the innate immune system during the onset of infection. PLoS One. 2007; 2:e631.
22. Gross A, Terraza A, Ouahrani-Bettache S, Liautard JP, Dornand J.
In vitro Brucella suis infection prevents the programmed cell death of human monocytic cells. Infect Immun. 2000; 68:342–351.

23. Meinecke I, Wille A, Cinski A, Neumann W, Ink B, Hay R, Gay S, Pap T. Involvement of SUMO-1 in the regulation of apoptosis in prosthesis loosening fibroblasts. Arthritis Res Ther. 2004; 6 Suppl 1:67.
24. Rajashekara G, Eskra L, Mathison A, Petersen E, Yu Q, Harms J, Splitter G. Brucella: functional genomics and host-pathogen interactions. Anim Health Res Rev. 2006; 7:1–11.
25. Haag AF, Myka KK, Arnold MF, Caro-Hernández P, Ferguson GP. Importance of lipopolysaccharide and cyclic β-1,2-glucans in Brucella-mammalian infections. Int J Microbiol. 2010; 2010:124509.
26. Cascales E, Christie PJ. The versatile bacterial type IV secretion systems. Nat Rev Microbiol. 2003; 1:137–149.

27. den Hartigh AB, Sun YH, Sondervan D, Heuvelmans N, Reinders MO, Ficht TA, Tsolis RM. Differential requirements for VirB1 and VirB2 during
Brucella abortus infection. Infect Immun. 2004; 72:5143–5149.

28. Machelart A, Khadrawi A, Demars A, Willemart K, De Trez C, Letesson JJ, Muraille E. Chronic
Brucella infection induces selective and persistent interferon gamma-dependent alterations of marginal zone macrophages in the spleen. Infect Immun. 2017; 85:e00115–e00117.











 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download