Abstract
Objective
This study aimed to identify possible risk factors for external apical root resorption (EARR) in the maxillary incisors after orthodontic treatment.
Methods
The root length of 2,173 maxillary incisors was measured on periapical radiographs of 564 patients who received orthodontic treatment. The Kappa test was performed to evaluate intraexaminer and interexaminer reproducibility. Multiple binary logistic regression was used to determine the association between EARR and various factors. Odds ratios and 95% confidence intervals were reported.
Results
The risk of developing EARR was 70% higher in orthodontic treatment with maxillary premolar extraction (p = 0.004), 58% higher in patients with increased overjet (p = 0.012), 41% lower in two-phase orthodontic treatment (p = 0.037), and 33% lower in patients with deep bite (p = 0.039). The lateral incisors were 54% more likely to develop EARR (p < 0.001), dilacerated roots were 2.26 times more likely to develop EARR (p < 0.001), and for each additional millimeter of root length, the risk of EARR increased by 29% (p < 0.001).
External apical root resorption (EARR) has been associated with orthodontic treatment.123 Its etiology is multifactorial,124567 and some of the possible orthodontic risk factors evaluated are treatment duration, orthodontic forces, extraction treatment, two-phase versus one-phase treatment, maxillary expansion, use of elastics, and bracket prescription. Some malocclusion characteristics were also studied, such as the Angle classification and the severity of overjet and overbite. Many studies have agreed that maxillary incisors are the most frequently resorbed teeth,8910 and teeth with root shapes other than rhomboid are more affected by EARR.811
Extraction treatment is considered a risk factor for EARR, but the findings of studies on this association have been very controversial.91012131415 Differences in the evaluated teeth showing EARR, different extraction patterns, distinct mechanics, and applied forces for space closure may justify this divergence. However, according to Brin et al.,16 two-phase treatment reduces the risk of EARR at the end of orthodontic treatment, since the early modification of growth in patients with Angle Class II malocclusions reduces the severity of overjet, which has been described as a risk factor for EARR. In addition, a pause in the treatment of these patients may contribute to this result, since the disruption of dental movement may favor the cement healing process of the teeth that have developed EARR.17
Among the malocclusion characteristics, increased overjet has been associated with EARR, since this malocclusion presumes a greater root displacement of the maxillary incisors during treatment and has been related to the use of rectangular orthodontic arch wires with active torque. A history of dental trauma has also been described as a risk factor for EARR.18 Similarly, deep bite is associated with the development of EARR in patients treated with incisor intrusion.419
Although many studies have evaluated the association between these variables and the occurrence of EARR, little consensus exists about the influence of factors such as root morphology, adjunctive treatments, and malocclusion traits on EARR. Differences in methodology and small sample sizes may explain this divergence, given that the division into subgroups is limited. Therefore, the interpretation of results is subject to criticism.781220 Another issue that may explain the difference in results is the sample origin. Sameshima and Sinclair8 found differences in the degree of EARR among patients with different backgrounds. They suggested that differences in the dental development process might exist because of the differences in tooth size and shape.
Considering the inconclusive literature on the possible risk factors associated with EARR after orthodontic treatment and the scarcity of research evaluating representative samples, the current study aimed to identify the possible risk factors for EARR in the maxillary incisors after orthodontic treatment.
This multicenter retrospective study was approved by the Research Ethics Committee of the State University of Rio de Janeiro (UERJ) (approval no. 1.605.015). The sample was selected from three institutions: UERJ, Pontifical Catholic University of Minas Gerais, and Federal University of Minas Gerais, where patients received orthodontic treatment between 1980 and 2016. The maxillary central and lateral incisors were evaluated because of their higher susceptibility to root resorption as reported in the literature.8910
Patients were included if they had diagnostically acceptable pretreatment and posttreatment records, including initial and final periapical radiographs of the maxillary incisors acquired no more than 6 months after the end of active orthodontic treatment. The exclusion criteria were incomplete root formation, dental trauma history, endodontic treatment, presence of restoration at the incisal edge, previous or incomplete orthodontic treatment, and systemic disorders or syndromes.
In total, 2,670 orthodontic records were selected for this study. After applying the inclusion and exclusion criteria, the final sample consisted of 564 patients. Eighty-three incisors were not evaluated because of endodontic treatment (n = 29), incisal edge restorations (n = 11), extraction (n = 10), orthodontic traction (n = 13) during treatment, and missing incisor at the beginning of treatment (n = 20). Hence, the final sample consisted of 2,173 maxillary incisors.
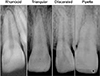
Two examiners (LQPF and NCF) were previously calibrated for record evaluation and radiographic measurements. The variables evaluated were sex, ethnicity, age, Angle malocclusion classification, overjet, overbite, skeletal pattern, treatment time, location of treatment, treatment with or without extraction of the maxillary premolar, one- or two-phase treatment, maxillary expansion, bracket prescription, orthognathic surgery, intermaxillary elastics, and root length and shape. All patients received corrective treatment using 0.022-inch bracket slots. The classification used for evaluating the root shape is shown in Figure 1.
All periapical radiographs were digitalized using a scanner with 300-dpi resolution and 256 levels of gray (Scanjet 4890; Hewlett-Packard, Palo Alto, CA, USA) and imported via the ImageJ software (National Institutes of Health, Bethesda, MD, USA) to better visualize and perform digital measurements of the incisors. The length of the radiographic film (40 mm) was used as reference to calibrate the image size. At measurement, both the examiners were double-blinded to the treatment time (initial or final) and patient. The points used for measurements are shown in Figure 2.
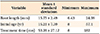
EARR was calculated according to the formula described by Linge and Linge,20 i.e., R1–R2 [C1/C2], with R1 being the root length before treatment; R2, the root length after treatment; C1, the crown length before treatment; and C2, the crown length after treatment. The crown length (C1 and C2) was defined as the distance from the central point of the cementoenamel junction (point C) to the central point of the incisal edge (point IE). For rhomboid, triangular, and pipette roots, the root length (R1 and R2) was defined as the distance from point C to the root apex (point RA). For dilacerated roots, two distances were added to define the root length: the distance from point C to the point of intersection between the long axis of the tooth, from C, and the long axis of the dilacerated root portion, from point RA (point I), and the distance from point I to point RA. The correction factor C1/C2 was applied, assuming the crown length to remain unchanged during the observation period. Incisors with EARR ≥ 2 mm were considered affected.
All statistical tests were performed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). Charts and tables were generated using Microsoft Excel® 2007 (Microsoft Corporation, Redmond, WA, USA). Descriptive analyses yielded the frequency of categorical variables and the mean with standard deviation of continuous variables.
A total of 120 teeth were randomly selected to be evaluated two times for EARR, by both examiners, with a 15-day interval between the evaluations. To evaluate intraexaminer and interexaminer reproducibility, the Kappa test was applied, and the agreement percentage was calculated.
The relationship between the variables was also analyzed. The occurrence of EARR was evaluated using multiple binary logistic regression modeling to estimate the odds ratios (ORs), in association with the generalized estimation equation to consider more than one tooth per patient. Initially, a univariate regression model was used and adjusted for all variables to eliminate possible confounding factors. The final regression model was adjusted only for the variables that showed a significant OR in the two previous steps, considering a significance level of 5%. In the final model, the 95% confidence interval for OR values was estimated.
The descriptive analyses of the sample are shown in Tables 1 and 2. The sample included 1,080 central incisors and 1,093 lateral incisors. In total, 810 teeth (37.3%) were affected by EARR ≥ 2 mm, and the lateral incisors were the most affected (Figure 3). Out of 1,434 rhomboid, 388 triangular, 110 pipette, and 241 dilacerated roots, the dilacerated ones were the most affected by EARR (Figure 4). Table 3 shows the Kappa test results, according to the classification suggested by Landis and Koch.21
Among the clinical characteristics, the final multivariate regression model showed that patients with increased overjet had a 58% greater chance of developing EARR during orthodontic treatment than did patients with normal overjet (p = 0.012), and patients with deep bite were 33% less likely to have EARR than were patients with normal overbite (p = 0.039). Among the variables related to orthodontic treatment, extraction of the maxillary premolars increased the chance of EARR by 70% (p = 0.004). However, patients who underwent two-phase treatment had a 41% lower chance of developing EARR than did patients who underwent singlephase treatment (p = 0.037). The maxillary lateral incisors were 54% more likely to be affected by EARR than were the central incisors (p < 0.001). As for root shape, the incisors with dilacerated roots had a 2.26 times greater chance of developing EARR during orthodontic treatment (p < 0.001), and the risk of EARR increased by 29% for each additional millimeter of root length (p < 0.001). The other variables evaluated in this study did not present statistically significant ORs (Table 4).
The aim of this investigation was to identify possible risk factors for the incidence of EARR in the maxillary incisors after orthodontic treatment. Hence, we used periapical radiographs, which are more reliable in estimating EARR than are panoramic films.22 Cone-beam computed tomography (CBCT) studies could be considered more accurate. However, this examination is not part of the routinely requested orthodontic documentation, and the cost and radiation exposure are greater in CBCT than in conventional two-dimensional examinations. The method proposed by Linge and Linge20 was reported as the most accurate one for evaluating EARR in periapical radiographs,23 thus supporting its use in this study. Moreover, the cutoff point of 2 mm to determine EARR was methodologically chosen to prevent potential overestimation of the occurrence of EARR because of the limitations of radiographic imaging.24
On the basis of the literature, our study evaluated the variables related to EARR in patients receiving orthodontic treatment. According to the descriptive analysis of the sample, we observed that some variables presented a great discrepancy in the number of participants in each group; therefore, these variables (indigenous ethnicity, Angle Class II Division 2 and Class III, negative overjet, Class III skeletal pattern, maxillary expansion, and orthognathic surgery) should be evaluated with caution.
The following nine variables were evaluated in the final regression model: overjet, overbite, maxillary premolar extraction, two-phase treatment, location and time of treatment, central and lateral incisors, and root length and shape. A greater chance of EARR is observed in patients with increased overjet, thus corroborating the findings of other studies.8101625 This malocclusion presumes a greater root displacement of the maxillary incisors during treatment, which explains why it is a high-risk factor for EARR. Regarding overbite, patients with deep bite present a less chance of EARR. Although some studies have already associated the development of EARR with incisor intrusion during the correction of deep bite,419 differences in the mechanics used to correct this malocclusion, which are associated with the force magnitude implemented and the required treatment time, can promote different degrees of EARR in these patients.
Our findings show that treatment with maxillary premolar extraction is the greatest risk factor for the occurrence of EARR, which is a controversial conclusion in the literature.91012131415 Differences in evaluated teeth showing EARR, extraction patterns, and the mechanics and forces applied for space closure may justify this divergence. According to Artun et al.,25 treatment with extractions is a factor that represents a greater amount of orthodontic movement; therefore, it is a risk factor for EARR. Nevertheless, in cases of severe crowding, a large retraction of the anterior teeth does not always occur; hence, this could be another possible confounding factor in the studies that evaluated the relationship between orthodontic treatment with extractions and EARR.
The lowest susceptibility to EARR is observed in patients treated in two phases, and this finding corroborates with those of Brin et al.16 The reduction of the initially increased overjet in these patients and the interval between the two phases of treatment, which favors the cement healing process of the teeth that have developed EARR, can justify this finding.1617
The location of treatment is not a statistically significant risk factor for EARR, as reported by Artun et al.25 All three educational institutions involved in this study have similar orthodontic philosophies, which may explain this finding. Despite the long mean treatment time of this study, it does not present a statistically significant OR in the final regression model. This finding is not in agreement with those of previous studies reporting that prolonged treatment time is a risk factor for EARR.101214151626 Considering that this sample comprised patients treated at educational institutions, the recess during the academic calendar could increase the total treatment time; however, this does not necessarily mean that the patients were undergoing active orthodontic treatment the entire time. Moreover, these interruptions of some weeks in active treatment could favor the cement healing process. According to Mehta et al.,17 60% of the teeth retained for 6 weeks as a rest period showed anatomical repair, and the remaining 40% showed functional repair. A systematic review also concluded that a pause in orthodontic treatment for patients experiencing root resorption can reduce the severity of this condition.27
The lateral incisors are more affected by EARR than are the central incisors, as shown in previous studies.89 In general, these teeth are exposed to greater root displacement during correction and improvement of malocclusion, function, and smile aesthetics. In addition, root morphology tends to transfer the forces mainly to the root apex, thus promoting EARR in these teeth.5 We observed that longer roots are more likely to develop EARR, thereby confirming the findings of other studies,1325 which reported that the greater the distance from the root apex to the point of orthodontic force application, the greater the tipping displacement. The incisors with root shapes other than rhomboid are more affected by EARR, especially the dilacerated roots, as reported by other studies.811 Although there is no direct proof, studies have suggested that the deviation in development that caused the abnormal shape may be associated with increased susceptibility to EARR in this region.8
The present study evaluated 564 patients who received orthodontic treatment at three institutions, and evaluated 19 risk factors for EARR after orthodontic treatment quantified in a total of 2,173 incisors. Many studies with a limited number of participants are found in the literature.7 However, since sample size may influence the results, one of the advantages of the present study is its larger sample size. The retrospective design and use of radiographs can also be cited as limitations of this work. In addition, it is important to consider that the inherent characteristics of each study population may interfere with the EARR process, since differences in the frequency of EARR as well as in the risk factors associated with EARR among populations have already been described in the literature.8 Recent studies also reported a genetic predisposition that may explain why one patient is more likely to develop EARR during orthodontic treatment than does another2829; therefore, individual variability should also be considered, even though it has not been evaluated in the present study.
On the basis of the current results, we can conclude that the risk of developing EARR ≥ 2 mm in the maxillary incisors is 70% higher in patients treated with maxillary premolar extraction; 58% higher in patients with increased overjet at the beginning of treatment; 41% lower in patients treated in two phases; and greater in the lateral incisors, dilacerated roots, and longer roots.
Figures and Tables
 | Figure 2References to the measurement of external apical root resorption in rhomboid, triangular, pipette (A), and dilacerated roots (B).RA, Root apex; M, mesial point of the cementoenamel junction (CEJ); D, distal point of the CEJ; C, central point of the line joining M and D; IE, central point of the incisal edge; I, point of intersection between the long axis of the tooth, from C, and the long axis of the dilacerated root portion, from the RA; R1, the root length before treatment; R2, the root length after treatment; C1, the crown length before treatment; C2, the crown length after treatment; Measurement 1, distance from point C to I; Measurement 2, distance from point I to the RA.
|
ACKNOWLEDGEMENTS
We would like to especially thank Dr Ronir Raggio Luiz for assistance with the statistical tests. This work was supported in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (CAPES) - [Finance Code 001].
Notes
References
1. Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part II: the clinical aspects. Angle Orthod. 2002; 72:180–184.
2. Hartsfield JK Jr, Everett ET, Al-Qawasmi RA. Genetic factors in external apical root resorption and orthodontic treatment. Crit Rev Oral Biol Med. 2004; 15:115–122.

3. Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod. 2002; 72:175–179.
4. Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010; 137:462–476. discussion 12A.

5. Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993; 103:138–146.

6. Roscoe MG, Meira JB, Cattaneo PM. Association of orthodontic force system and root resorption: a systematic review. Am J Orthod Dentofacial Orthop. 2015; 147:610–626.

7. Segal GR, Schiffman PH, Tuncay OC. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004; 7:71–78.

8. Sameshima GT, Sinclair PM. Predicting and preventing root resorption: part I. Diagnostic factors. Am J Orthod Dentofacial Orthop. 2001; 119:505–510.

9. de Freitas JC, Lyra OC, de Alencar AH, Estrela C. Long-term evaluation of apical root resorption after orthodontic treatment using periapical radiography and cone beam computed tomography. Dental Press J Orthod. 2013; 18:104–112.

10. Maués CP, do Nascimento RR, Vilella Ode V. Severe root resorption resulting from orthodontic treatment: prevalence and risk factors. Dental Press J Orthod. 2015; 20:52–58.

11. Levander E, Malmgren O, Stenback K. Apical root resorption during orthodontic treatment of patients with multiple aplasia: a study of maxillary incisors. Eur J Orthod. 1998; 20:427–434.

12. Picanço GV, de Freitas KM, Cançado RH, Valarelli FP, Picanço PR, Feijão CP. Predisposing factors to severe external root resorption associated to orthodontic treatment. Dental Press J Orthod. 2013; 18:110–120.

13. Fontana ML, de Souza CM, Bernardino JF, Hoette F, Hoette ML, Thum L, et al. Association analysis of clinical aspects and vitamin D receptor gene polymorphism with external apical root resorption in orthodontic patients. Am J Orthod Dentofacial Orthop. 2012; 142:339–347.

14. Lee YJ, Lee TY. External root resorption during orthodontic treatment in root-filled teeth and contralateral teeth with vital pulp: a clinical study of contributing factors. Am J Orthod Dentofacial Orthop. 2016; 149:84–91.

15. Sharab LY, Morford LA, Dempsey J, Falcão-Alencar G, Mason A, Jacobson E, et al. Genetic and treatmentrelated risk factors associated with external apical root resorption (EARR) concurrent with orthodontia. Orthod Craniofac Res. 2015; 18 Suppl 1:71–82.

16. Brin I, Tulloch JF, Koroluk L, Philips C. External apical root resorption in Class II malocclusion: a retrospective review of 1- versus 2-phase treatment. Am J Orthod Dentofacial Orthop. 2003; 124:151–156.

17. Mehta SA, Deshmukh SV, Sable RB, Patil AS. Comparison of 4 and 6 weeks of rest period for repair of root resorption. Prog Orthod. 2017; 18:18.

18. Linge L, Linge BO. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991; 99:35–43.

19. Aras I, Tuncer AV. Comparison of anterior and posterior mini-implant-assisted maxillary incisor intrusion: root resorption and treatment efficiency. Angle Orthod. 2016; 86:746–752.

20. Linge BO, Linge L. Apical root resorption in upper anterior teeth. Eur J Orthod. 1983; 5:173–183.

21. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.

22. Sameshima GT, Asgarifar KO. Assessment of root resorption and root shape: periapical vs panoramic films. Angle Orthod. 2001; 71:185–189.
23. Brezniak N, Goren S, Zoizner R, Dinbar A, Arad A, Wasserstein A, et al. A comparison of three methods to accurately measure root length. Angle Orthod. 2004; 74:786–791.
24. Bastos Lages EM, Drummond AF, Pretti H, Costa FO, Lages EJ, Gontijo AI, et al. Association of functional gene polymorphism IL-1beta in patients with external apical root resorption. Am J Orthod Dentofacial Orthop. 2009; 136:542–546.

25. Artun J, Van 't Hullenaar R, Doppel D, Kuijpers-Jagtman AM. Identification of orthodontic patients at risk of severe apical root resorption. Am J Orthod Dentofacial Orthop. 2009; 135:448–455.

26. Jiang F, Chen J, Kula K, Gu H, Du Y, Eckert G. Root resorptions associated with canine retraction treatment. Am J Orthod Dentofacial Orthop. 2017; 152:348–354.

27. Currell SD, Liaw A, Blackmore Grant PD, Esterman A, Nimmo A. Orthodontic mechanotherapies and their influence on external root resorption: a systematic review. Am J Orthod Dentofacial Orthop. 2019; 155:313–329.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download