Abstract
Objective
The objectives of this study were to evaluate linear and volumetric alveolar changes induced by nasoalveolar molding (NAM) in infants with complete unilateral cleft lip and palate (UCLP) and compare the maxillary dimensions after NAM with the normal dimensions in infants without clefts.
Methods
A total of 26 infants with UCLP treated by NAM (mean age before and after NAM: 14.20 ± 8.09 days and 118.16 ± 10.06 days, respectively) comprised the treatment group, while 26 infants without clefts (mean age: 115.81 ± 8.71 days) comprised the control group. Changes in the maxillary dimensions following NAM were measured on three-dimensional models using Mimics software, version 17.0.
Results
During NAM, there was a decrease in the cleft widths, maxillary arch depths, and rotation of the greater segment. While the anterior alveolar arch width exhibited a significant decrease, the posterior arch width was mostly maintained. There were no changes in the anterior vertical deviations of the alveolar segments. The alveolar crest lengths, arch circumference, and bilateral posterior volumetric measures exhibited an increase. After NAM, the anterior arch width was comparable between the treatment and control groups, whereas the posterior arch width and anterior vertical deviations were greater in the treatment group than in the control group. The maxillary arch depths, alveolar crest lengths, and maxillary volumes were smaller in the NAM group than in the control group.
Conclusions
During NAM in infants with UCLP, the cleft width and anteroposterior and transverse alveolar dimensions exhibited a decrease while the vertical dimensions were maintained. Compared with infants without clefts, those with UCLP treated by NAM exhibited sagittal and vertical alveolar growth deficiencies and tissue insufficiency.
Cleft lip and palate (CLP) is one of the most common congenital deformities. The treatment of this deformity requires an interdisciplinary approach for the restoration of both esthetics and function, starting from birth and continuing until adulthood.123 CLP deformities show high variability according to the affected anatomical structures, amount of tissue deficiency, and segmental displacement.456 In unilateral CLP (UCLP), the maxilla is composed of two segments: greater and lesser. In general, the greater segment shows anterolateral rotation while the lesser segment shows medial rotation at birth.2345678 However, some researchers maintain that the lesser segment shows lateral rotation due to tongue insertion into the cleft area.8910 Both segments also display different amounts of vertical deviation toward the nasal cavity.7 These segmental displacements together with tissue deficiency increase the severity of the deformity. For the achievement of maximum esthetic and functional results with minimal scar tissue after primary surgery, presurgical orthopedic (PSO) treatment involving leveling of the alveolar segments, correction of the arch form, and reduction of the cleft width is performed to decrease the severity of the initial deformity. Several PSO treatment methods have been defined and developed over time. In 1993, Grayson et al.1 introduced nasoalveolar molding (NAM), which differs from conventional PSO treatments. It involves molding of the deformed alar cartilage in addition to alveolar leveling. Because it facilitates both intra- and extraoral corrections, NAM is a preferred treatment method in several clinics.
Although numerous studies have evaluated the transverse and sagittal alveolar changes induced by NAM in patients with UCLP,11121314151617 studies evaluating the vertical deviations of the cleft segments toward the nasal cavity, which may pose a problem for surgical and orthodontic treatment, are limited.161819 The general conclusion in these studies, which involved pre- and post-treatment measurements, is that NAM decreases the alveolar cleft width and improves the arch form by aligning the deviated alveolar segments. However, the lack of control groups prevented the comparison of final arch forms and dimensions with those in patients without clefts.
Therefore, the aims of the present study were to evaluate transverse, sagittal, and vertical alveolar changes induced by NAM in infants with UCLP and compare the maxillary dimensions after NAM with the normal dimensions in infants without clefts.
This retrospective study was approved by the Institutional Review Board of Yeditepe University (58/490). The parents of all patients were informed about the study and provided their consent. The records of potential subjects whose parents refused to participate in the study were not included. The archive of the Craniofacial Clinic of Yeditepe University was searched for records of patients who were treated by NAM performed by two senior orthodontists according to the method of Grayson et al.2 between 2010 and 2015. The records were screened, and patients who fulfilled the following inclusion criteria were enrolled in the NAM group: nonsyndromic complete UCLP without any Simonart band, regular attendance for all treatment visits, and good-quality records. From the same archive, the records of infants without clefts, which were collected for study purposes, were retrieved and included in the study for comparisons. The inclusion criteria for patients in the control group were as follows: absence of CLP or any craniofacial deformity and an age matched with the post-NAM age of the infants in the treatment group. According to Grayson and Maull,19 the NAM treatment protocol involves gradual approximation of the alveolar segments by modification of the molding plate at weekly intervals; this is achieved through the selective removal of acrylic (no more than 1 mm) from the area into which the alveolar bone should grow and the addition of a soft liner on the contralateral side. When vertical deviation is present, vertical trimming at the poles of the greater and lesser alveolar segments is performed for the guidance of vertical bone growth. After fabrication, the appliance is secured by surgical retention tapes and orthodontic elastics (1/4 inch heavy elastics). The tapes are diagonally applied on the cheeks with vertical and horizontal force vectors. For the generation of an appropriate activation force of 2 ounce, the elastic should be stretched to approximately two times the diameter at rest. The tapes should be changed daily. A horizontal tape is also applied for approximation of the lips. When the cleft width is reduced to 5 mm, a nasal stent is added for molding of the septal cartilage. Following delivery of the plate, oral and written instructions concerning appropriate insertion of the plate and application of the tapes are provided to the parents/guardians, because NAM therapy requires caregiver compliance and proper application of the tapes and plate. The patient is recalled every week for the evaluation of changes and adjustment of the plate.
Dental casts were scanned by a D700 laser model scanner (3Shape, Copenhagen, Denmark), which exhibits a 20-µm accuracy. The obtained virtual models in stereolithographic format were imported into a three-dimensional (3D) CAD software program (ver. 17.0, Mimics; Materialise, Leuven, Belgium) for measurements. A total of 19 points (one artificial, 18 anatomical) were defined and marked on the digital models (Table 1 and Figure 1A).
The positions of all landmarks on the 3D models were two-dimensionally checked in the sagittal, coronal, and axial planes (Figure 1A). Subsequently, 10 reference planes based on the landmarks were defined (Table 1). As described by Börnert et al.,18 a horizontal plane (HP) based on the bilateral tuberosity points and the noncleft canine point was used for evaluation of the anterior vertical deviations of the alveolar segments toward the nasal cavity (Figure 1B). For volumetric measurements, differential analysis was performed by segmentation of the alveolar structures by vertical reference planes and a horizontal reference plane (HRP) passing through the bilateral tuberosity points and gingival groove point on the greater segment (Figure 2), because Braumann et al.20 reported that morphological changes in the alveolar segments in patients with clefts are not uniform. Using these landmarks and reference planes, we obtained linear, angular, and volumetric measurements as shown in Table 2 and Figure 3. Pre- (T0) and post-NAM (T1) measurements were compared for the patients in the treatment group. In addition, the maxillary dimensions after NAM in the treatment group were compared with the dimensions in the infants in the control group.
To compare the alveolar crest lengths between post-NAM (T1) and the control group, the maxillary alveolar crest as divided into two parts with reference to incisal (I) point.
According to this segmentation, in the treatment group we named the half of the maxillary alveolar crest including cleft as ‘cleft side’ and the contralateral crest as ‘non-cleft side’. As shown in the Table 3, the cleft side alveolar crest length of the NAM group was compared to the right side alveolar crest length of the control group, whereas the non-cleft side alveolar crest length of the NAM group was compared to left side alveolar crest length of the control group.
All statistical analyses were performed using the Number Cruncher Statistical System, 2007 (NCSS, LLC., Kaysville, UT, USA).
Descriptive statistics (mean, standard deviation) were performed, and normal distribution of the data was tested using the Shapiro–Wilk test. Normally distributed pre- and post-NAM data were compared using paired t-tests, while post-NAM data were compared with the control group values using independent t-tests. A p-value of < 0.05 was considered statistically significant. Pearson's correlation analysis was used to determine the association between two variables.
Experimental statistical power analyses using the G*Power 3.1 program (Heinrich Heine Universitat, Dusseldorf, Germany) were used to determine the study power. In accordance with the study of Yu et al.,16 the sample size was calculated on the basis of a 2.04-mm mean difference (standard deviation, 1.79 mm) in the anterior arch depth between the treatment and control groups. The calculation revealed that 24 patients per group were required for a study with a power of 0.80 and an alpha of 0.05.
For evaluation of the measurement error and intraoperator reliability, the same investigator repeated the landmark positioning and measurement procedures for the maxillary virtual models of 10 randomly selected patients (pre- and post-treatment models) and controls at 30 days after the original measurements. The calculated interclass correlation coefficients were between 0.763 and 0.997, which indicated consistency in the repeated measurements.
The treatment group included 26 patients with UCLP (nine girls and 17 boys) who underwent NAM. The mean ages before and after NAM were 14.20 ± 8.09 and 118.16 ± 10.06 days, respectively. The control group included 26 infants without clefts (eight girls and 18 boys; mean age, 115.81 ± 8.71 days).
The mean anterior and posterior cleft widths significantly decreased after NAM (p < 0.001; Table 4). Although the anterior arch width exhibited a significant decrease, with a mean value of 3.4 mm (p < 0.001) after NAM, the posterior arch width exhibited only a slight increase (p > 0.05; Table 4). While the anterior arch widths after NAM were not significantly different from the anterior arch width in the control group, the posterior arch width after NAM was significantly greater than the control value (p < 0.05; Table 3).
The transverse distance from the A point to the midline was considered negative (−) if the A point was positioned on the noncleft side of the midline and positive (+) if the A point was positioned on the cleft side. Accordingly, this distance exhibited a negative value before NAM and a positive value after NAM, which was achieved by movement of the A point toward the cleft side. The transverse distances from the I, C2, and A′ points to the midline exhibited a significant decrease after treatment (p < 0.001; Table 4). The distance between the midline and the T and T′ points were greater in the NAM group than in the control group, while the distance between the midline and the C2′ point was smaller in the former than in the latter (p < 0.01 for all; Table 3).
The IZT angle increased while the ZTC2 and ZT′C2′ angles decreased after NAM, with significant differences between pre- and post-NAM values (p < 0.001, p < 0.01, and p < 0.05, respectively; Table 4). In addition, the T-PP/T′-PP ratio significantly increased from 0.47 to 0.82 (p < 0.001; Table 4).
The anterior arch depth, total arch depth, and I-Z distance exhibited a significant decrease after NAM (p < 0.001, p < 0.05 and p < 0.01, respectively; Table 4). Comparison between the NAM and control groups revealed that the anterior and total arch depths were 2.16 and 4.57 mm lesser, respectively, in the NAM group (p < 0.001; Table 3). The sagittal distance from the A point to the posterior plane showed a significant decrease after NAM because of posteromedial rotation of the greater segment (p < 0.01). On the other hand, the sagittal distance between the A′ and C2′ points significantly increased after NAM (p < 0.001 and p < 0.05; Table 4).
The mean vertical distances between HP and the A, I, and A′ points showed no changes after NAM (Table 4). However, the vertical distance between the I point and HP was significantly greater in the NAM group than in the control group (p < 0.001; Table 3).
The alveolar crest length, which was measured segmentally between the anatomical landmarks to comprise greater and lesser segment lengths; and the arch circumference, was calculated from the sum of greater and lesser segments (Table 2). The lengths of the greater and lesser segments significantly increased after NAM (p < 0.05; Table 4). The arch circumference also showed a significant increase, with a mean value of 2.96 mm after NAM (p < 0.05). All three post-NAM values were significantly smaller than the control values (p < 0.001, p < 0.01, and p < 0.05, respectively; Table 3).
During the NAM, only the posterior regions of the greater and the lesser segments showed significant volumetric increases (p < 0.01, and p < 0.05, respectively) (Table 4). All volumetric measurements were smaller in the NAM group than in the control group (Table 3).
Correlations between the amount of reduction in the anterior cleft width and the changes during NAM treatment were evaluated using Pearson's correlation analysis. Changes in the distances between the midline and the I, C2, and A′ points; anterior arch depth; distance between the I and Z points; and lesser segment volume exhibited positive correlations, whereas the change in the distance between the A point and the midline exhibited a negative correlation (Table 5). Description of the landmarks used in this study are depicted in Tables 1 and 2.
The goals of NAM therapy are to normalize the maxillary morphology by reducing the severity of the initial cleft deformity and achieve optimal surgical outcomes with minimal scar formation.231314151617 Moreover, leveling of the alveolar structures, which support the nose and lip segments, provides a better environment for appropriate soft tissue molding.19 While a few studies have investigated the effects of NAM at the level of the alveolus,1112131415161721 they mostly evaluated transverse and sagittal alveolar changes induced by the treatment.1314151617 However, assessment of the vertical dimensions of the alveolar segments after treatment, which can result in vertical malalignment or insufficient vertical growth, is very crucial. In addition, volumetric measurements may present valuable information about possible tissue deficiency and the osteogenic growth potential. Two-dimensional (2D) analyses are not capable of evaluating vertical and volumetric changes in an accurate manner. Therefore, the present study performed 3D analysis on virtual models by using specialized software in order to increase the measurement variability and overcome the methodological limitations of direct measurements on plaster models and indirect 2D measurements.
Studies evaluating the effects of NAM are generally based on the comparison of pre- and post-treatment variables.1113141516 However, the main criteria for judging the effectiveness of any PSO treatment is concordance of the post-treatment maxillary arch form and dimensions in infants with CLP with the arch form and dimensions in age-matched infants without clefts. Accordingly, we included a control group of age-matched infants without CLP for post-treatment comparisons.
The amount of decrease in the alveolar cleft width is also considered an indicator of the effectiveness of PSO treatment.231517222324 As expected, anterior and posterior cleft widths decreased significantly following NAM in the present study. Alveolar molding is mainly effective in the anterior region.11 Our correlation analysis revealed that the decrease in the anterior cleft width was particularly caused by posteromedial rotation of the greater segment during molding.8152125 On the other hand, no segmental movement was seen in the posterior region, and the decrease in the posterior cleft width can be attributed to growth and remodeling at the medial borders of the cleft segments.1126 We observed a decrease of approximately 3 mm in the anterior alveolar arch width in our patients. The results for changes in the anterior arch width during treatment in previous studies are controversial. While Baek and Son11 reported a significant decrease in the anterior arch width, other authors found no significant changes in this parameter.1416 These discrepancies in results may be caused by differences in the severity of the initial deformity, the amount and direction of correction by appliance therapy, and variations in individual growth potentials. Although the anterior alveolar arch widths decreased after NAM, it was not significantly different from the value for the control group. This finding suggests that NAM does not cause overconstriction of the maxillary arch. We also found a slight increase in the posterior arch width after NAM. In general, studies on NAM have reported no change or a slight decrease in the posterior arch width.111516 In fact, in the present study, the post-NAM posterior arch was about 1.7 mm wider than the posterior arch in the control group. These findings strongly support the belief that neonatal orthopedic treatment has no constrictive effects on the posterior arch width.
In the present study, linear and angular measurements were performed for the evaluation of segmental movements. The most prominent movement toward the midline was observed at the pole of the greater segment, with a progressive decrease in the posterior direction and negligible movement at the tuberosity points (Table 4). As stated by Baek and Son,11 the posterior alveolar structures serve as a hinge point during posteromedial rotation of the greater segment by NAM, which results in midline correction and improvement in the arch symmetry (Table 4).
In the sagittal plane, although the inward and backward movement of the greater segment resulted in a significant decrease in the arch depth, the arch depth of the lesser segment increased either because of growth or anterior displacement.2728 The arch depths after NAM were smaller than the arch depths in the control group, probably because of the limiting effects of the retention tapes on growth of the greater segment, possible tissue deficiency, or growth insufficiency.
The vertical deviations of the anterior portion of both segments remained largely unchanged after NAM. However, the deviations were larger in the treatment group than in the control group. Yu et al.16 reported a significant increase in the anterior vertical deviations toward the nasal cavity after modified NAM therapy, which was greater than that in untreated patients with UCLP. The authors concluded that vertical growth of the alveolar segments was inhibited by the vertical forces of the retention tapes during treatment. However, a study showed that the anterior vertical deviations of the alveolar segments remain unchanged during PSO treatment without retention tape application.18 Therefore, the application of mild extraoral forces may eliminate or at least minimize the negative effects of the retention tapes on vertical growth. In the present study, evaluation of individual casts showed variable vertical movements induced by NAM, even though a similar treatment protocol was followed for every patient in terms of activation, interappointment intervals, and retention tape application. For example, some patients with increased initial vertical deviations showed a significant decrease as a result of vertical trimming within the appliance and growth during treatment, whereas some showed opposing findings possibly caused by inappropriate application of the retention tapes (Figure 4). During the treatment of infants with CLP, one should consider the likelihood of individual differences between patients in terms of the severity of the initial deformity and the response to treatment, which is also partly related to caregiver compliance. Although all caregivers receive the same oral and written instructions, some may experience difficulties in tape application. As mentioned earlier, the vertical deviations after NAM were greater than those in the control group. Börnert et al.18 reported that initial nasal deviations of the segments should be taken into account during vertical dimensional evaluations. Accordingly, these individual differences may be a result of variations in the amount of tissue deficiency and individual growth potential.
The present study found significant increases in the alveolar crest lengths and arch circumference after NAM. Previous studies have shown similar length increases, which were explained by growth. The researchers concluded that PSO treatment does not inhibit alveolar segmental growth.14152029 However, we found that the crest lengths in all regions were significantly smaller in the NAM group than in the control group. Because the control included infants without clefts, we could not determine whether this difference was caused by tissue deficiency or the limiting effect of the appliance on alveolar growth.
After NAM, significant increases were seen in volumetric measurements, particularly in the posterior region of the alveolar segments. As mentioned by Berkowitz,30 most of the growth occurs posteriorly so that the developing primary and permanent molars can be accommodated. Similarly, Braumann et al.20 reported larger volume increases in the molar region during PSO treatment using passive plates. The segment volumes are, to a large degree, determined by the number and size of developing tooth germs.
In volumetric evaluations, the vertical dimensions and growth of segments must be considered. The vertical deviation increases continuously from the posterior to the anterior region, with the maximum deviation in the pole region. Moreover, it is more prominent on the cleft side than on the noncleft side in patients with UCLP.20 Therefore, in volumetric segmentation, the amount of tissue loss increases toward the anterior region, particularly in the pole region. Thus, the variability in the vertical deviations in the present study could cause some data loss during segmentation. Further studies with larger samples are required to overcome the limitation of individual variations.
All volumetric measurements obtained after NAM were significantly smaller than the control measurements in the present study. These dimensional differences were uniform throughout the noncleft side, whereas they were more prominent in the anterior region on the cleft side. This may be indicative of the lack of adequate tissue due to the alveolar cleft in this region.516202528 We found that volumetric measurements on the noncleft side were also smaller in the NAM group than in the control group. This indicated not only some amount of tissue deficiency on the noncleft side but also maxillary hypoplasia.28
A reference plane is particularly required for evaluation of volumetric changes and the 3D topography of the maxilla. Previous studies used intra- or extramaxillary planes for this purpose.1020293132 In the present study, HRP was set to pass through the bilateral tuberosity points and gingival groove point on the greater segment, similar to the method used by Braumann et al.202931 for volumetric evaluation of the alveolus after PSO treatment in infants with CLP. The tuberosity points reportedly exhibit high reliability and reproducibility; moreover, the distance between these landmarks seems to be the most stable because it is correlated with the distance between the pterygoid processes.43133 Furthermore, during NAM, significant changes in the relative vertical positions of the tuberosity points on the lesser and greater segments are not expected because there is no vertical trimming in these regions. Vertical adjustment is only made anterior to the canine region, i.e., at the poles of the greater and lesser segments, when necessary. Therefore, we considered the tuberosity points as relatively stable landmarks. On the other hand, reference planes constructed using extramaxillary structures are advantageous because they are not affected by alveolar molding. However, this necessitates more complicated and invasive methods, such as preparation of maxillary and facial casts from intra- and extraoral impressions and a procedure similar to facebow transfer, which is inconvenient in infants.1032
1. In infants with UCLP, NAM treatment decreased the anterior cleft width primarily by posteromedial rotation of the greater segment. The posterior cleft width also decreased as a result of growth and remodeling at the cleft margins.
2. The arch depth decreased and the midline deviation and arch symmetry were improved by posteromedial rotation of the greater segment.
3. There were no adverse effects on the transverse growth of the maxilla; furthermore, the anterior vertical dimensions were unchanged.
4. Compared with the alveolar dimensions in infants without clefts, alveolar segments in infants with UCLP treated by NAM remained hypoplastic despite an increase in their dimensions.
Figures and Tables
 | Figure 1Positioning of landmarks for the measurement of alveolar changes after nasoalveolar molding in infants with unilateral cleft lip and palate. A, The landmarks are positioned on a maxillary virtual model using Mimics software, version 17.0 (Materialise, Leuven, Belgium). After positioning on the three-dimensional model, the location of each landmark (in this figure, B point) was two-dimensionally checked in the axial, sagittal, and coronal planes. B, For evaluation of the vertical deviations, a horizontal plane is constructed using the following three points: 1) greater segment tuberosity point (T), 2) lesser segment tuberosity point (T′), and 3) greater segment canine point (C2).See Table 1 for definitions of each landmark.
|
 | Figure 2Alveolar segmentation for the measurement of changes after nasoalveolar molding in infants with unilateral cleft lip and palate. The alveolar segments are separated from the maxillary virtual model 5 mm below the horizontal reference plane. For volumetric measurements, the segments are sectioned using the I, C1, C2, and C2′ volumetric planes.See Table 1 for definitions of each landmark.
|
 | Figure 3Transverse and sagittal measurements after nasoalveolar molding in infants with unilateral cleft lip and palate. A, Transverse linear and angular measurements. B, Sagittal measurements.1, Anterior cleft width (A-A′); 2, anterior arch width (C2-C2′); 3, inferior anterior arch width (G-G′); 4, posterior cleft width (P-P′); 5, posterior arch width (T-T′); 6, posterior position of the greater segment (Z-T-C2); 7, posterior position of the lesser segment (Z-T′-C2′); 8, greater segment rotation (I-Z-T); 9, anterior arch depth (I-AnP); 10, anterior position of the greater segment (I-Z); 11, total arch depth (I-PoP); 12, alveolar arch length in the lesser segment (A′-PoP); 13, canine-posterior plane distance in the greater segment (C2-PoP); 14, canine-posterior plane distance in the lesser segment (C2′-PoP).
|
 | Figure 4Vertical deviations after nasoalveolar molding (NAM) in two different representative cases with unilateral cleft lip and palate. A, Increased vertical deviations after treatment. In this patient, the initial vertical deviations did not improve with treatment, probably because of the excessive vertical component of the extraoral force caused by inappropriate use of the retention tapes or individual differences in the amount of tissue deficiency and growth potential. B, Decreased vertical deviations after treatment. In this patient, a significant decrease has occurred as a result of vertical trimming inside the appliance and growth during the treatment.T0, Before treatment; T1, after treatment.
|
Table 1
Definition of landmarks used for the measurement of alveolar changes after nasoalveolar molding in infants with unilateral cleft lip and palate

Table 2
Abbreviations and definitions of measurements used for the assessment of alveolar changes after nasoalveolar molding in infants with unilateral cleft lip and palate

Table 3
Comparison between maxillary dimensions after nasoalveolar molding in infants with unilateral cleft lip and palate (UCLP) and the maxillary dimensions in age-matched infants without clefts (independent t-test)
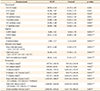
Table 4
Comparison of variables before and after nasoalveolar molding in infants with unilateral cleft lip and palate

Table 5
Correlations between changes in maxillary variables and the decrease in the anterior cleft width after nasoalveolar molding in infants with unilateral cleft lip and palate

T0, Before treatment; T1, after treatment.
*p < 0.05, **p < 0.01, ***p < 0.001.
See Table 2 for definition of each landmark.
Notes
References
1. Grayson BH, Cutting C, Wood R. Preoperative columella lengthening in bilateral cleft lip and palate. Plast Reconstr Surg. 1993; 92:1422–1423.
2. Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999; 36:486–498.

3. Grayson BH, Cutting CB. Presurgical nasoalveolar orthopedic molding in primary correction of the nose, lip, and alveolus of infants born with unilateral and bilateral clefts. Cleft Palate Craniofac J. 2001; 38:193–198.

4. Kriens O. Data-objective diagnosis of infant cleft lip, alveolus, and palate. Morphologic data guiding understanding and treatment concepts. Cleft Palate Craniofac J. 1991; 28:157–168.

5. Mazaheri M, Athanasiou AE, Long RE Jr, Kolokitha OG. Evaluation of maxillary dental arch form in unilateral clefts of lip, alveolus, and palate from one month to four years. Cleft Palate Craniofac J. 1993; 30:90–93.

6. Berkowitz S. Facial and palatal growth. In : Berkowitz S, editor. Cleft lip and palate. 2nd ed. Heidelberg: Springer;2006. p. 23–34.
7. Huddart AG, MacCauley FJ, Davis ME. Maxillary arch dimensions in normal and unilateral cleft palate subjects. Cleft Palate J. 1969; 6:471–487.
8. Mishima K, Sugahara T, Mori Y, Sakuda M. Three-dimensional comparison between the palatal forms in infants with complete unilateral cleft lip, alveolus, and palate (UCLP) with and without Hotz's plate. Cleft Palate Craniofac J. 1996; 33:77–83.

9. Wada T, Miyazaki T. Growth and changes in maxillary arch form in complete unilateral cleft lip and cleft palate children. Cleft Palate J. 1975; 12:115–130.
10. Bacher M, Göz G, Pham T, Bacher U, Werner O, Buchner P, et al. Three-dimensional analysis of cleft palate topology in newborn infants with reference to the cranial skeleton. Cleft Palate Craniofac J. 1998; 35:379–395.

11. Baek SH, Son WS. Difference in alveolar molding effect and growth in the cleft segments: 3-dimensional analysis of unilateral cleft lip and palate patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:160–168.

12. Ezzat CF, Chavarria C, Teichgraeber JF, Chen JW, Stratmann RG, Gateno J, et al. Presurgical nasoalveolar molding therapy for the treatment of unilateral cleft lip and palate: a preliminary study. Cleft Palate Craniofac J. 2007; 44:8–12.

13. Yağcı A, Uysal T. Evaluation of the effects of nasoalveolar molding method on cleft segments and alveolar widths of babies with unilateral cleft lip and palate. Sağlık Bilimleri Dergisi. 2007; 16:1–10.
14. Keçik D, Enacar A. Effects of nasoalveolar molding therapy on nasal and alveolar morphology in unilateral cleft lip and palate. J Craniofac Surg. 2009; 20:2075–2080.

15. Sabarinath VP, Thombare P, Hazarey PV, Radhakrishnan V, Agrekar S. Changes in maxillary alveolar morphology with nasoalveolar molding. J Clin Pediatr Dent. 2010; 35:207–212.

16. Yu Q, Gong X, Shen G. CAD presurgical nasoalveolar molding effects on the maxillary morphology in infants with UCLP. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:418–426.

17. Mandwe RS, Puri S, Shingane S, Pawar G, Kolhe VR, Alsi A. Presurgical nasoalveolar remodeling - an experience in the journey of cleft lip and palate. Clin Cosmet Investig Dent. 2015; 7:1–7.
18. Börnert H, Dannhauer KH, Schmalzried D. Vertical changes in the positions of the cleft segments of patients with unilateral cleft lip and palate. Changes from birth to palatoplasty at the age of 10–14 months. J Orofac Orthop. 2002; 63:51–61.

19. Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus and palate. In : Berkowitz S, editor. Cleft lip and palate. 2nd ed. Heidelberg: Springer;2006. p. 451–458.
20. Braumann B, Keilig L, Stellzig-Eisenhauer A, Bourauel C, Bergé S, Jäger A. Patterns of maxillary alveolar arch growth changes of infants with unilateral cleft lip and palate: preliminary findings. Cleft Palate Craniofac J. 2003; 40:363–372.

21. Isogawa N, Ochiai S, Mito T, Kindaichi J, Ishibashi N, Takagi Y, et al. Three-dimensional comparison in palatal forms between modified presurgical nasoalveolar molding plate and Hotz's plate applied to the infants with unilateral cleft lip and palate. Singapore Dent J. 2010; 31:36–42.

22. Hotz MM, Gnoinski WM. Effects of early maxillary orthopaedics in coordination with delayed surgery for cleft lip and palate. J Maxillofac Surg. 1979; 7:201–210.

23. Millard DR Jr, Latham RA. Improved primary surgical and dental treatment of clefts. Plast Reconstr Surg. 1990; 86:856–871.

24. Adali N, Mars M, Petrie A, Noar J, Sommerlad B. Presurgical orthopedics has no effect on archform in unilateral cleft lip and palate. Cleft Palate Craniofac J. 2012; 49:5–13.

25. Prahl C, Kuijpers-Jagtman AM, Van't Hof MA, Prahl-Andersen B. A randomized prospective clinical trial of the effect of infant orthopedics in unilateral cleft lip and palate: prevention of collapse of the alveolar segments (Dutchcleft). Cleft Palate Craniofac J. 2003; 40:337–342.

26. Berkowitz S, Duncan R, Evans C, Friede H, Kuijpers-Jagtman AM, Prahl-Anderson B, et al. Timing of cleft palate closure should be based on the ratio of the area of the cleft to that of the palatal segments and not on age alone. Plast Reconstr Surg. 2005; 115:1483–1499.

27. Burston WR. The early orthodontic treatment of cleft palate conditions. Dent Pract. 1958; 9:41–52.
28. Huddart AG. Presurgical changes in unilateral cleft palate subjects. Cleft Palate J. 1979; 16:147–157.
29. Braumann B, Rosenhayn SE, Bourauel C, Jäger A. Two- or three-dimensional cast analysis in patients with cleft lip and palate? J Orofac Orthop. 2001; 62:451–465.

30. Berkowitz S. The effect of clefting of the lip and palate an the palatal arch form. In : Berkowitz S, editor. Cleft lip and palate. 2nd ed. Heidelberg: Springer;2006. p. 43–54.
31. Braumann B, Keilig L, Bourauel C, Jäger A. Three-dimensional analysis of morphological changes in the maxilla of patients with cleft lip and palate. Cleft Palate Craniofac J. 2002; 39:1–11.

32. Wada T, Mizokawa N, Miyazaki T, Ergen G. Maxillary dental arch growth in different types of cleft. Cleft Palate J. 1984; 21:180–192.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download